Abstract
Purpose of Review
Impacts from climate change and use of toxic chemicals that contaminate our environment continue to pose a threat to the health of human populations. The field of wastewater-based epidemiology (WBE) has evolved significantly in recent years due to the COVID-19 global pandemic, however, investigating the utility of this application to fit within a broader environmental public health framework remains relatively unexplored. This review offers a comprehensive summary of the historical progression of WBE and highlights recent notable advancements to support its use for assessing environmental exposures in human populations.
Recent Findings
Early pioneering studies confirmed feasibility of this application, including measuring pesticides, plasticizers, and flame retardants in influent wastewater, that offered foundational knowledge to support successful expansion in recent work, including exposure to heavy metals and mycotoxins. Collectively, it was identified that evaluating biomarker suitability (e.g., in-sewer degradation, specificity) and pharmacokinetic data of excreted metabolites are crucial for accurate interpretation of results. Additionally, measurements of contaminants differed between catchment areas, indicating disproportionate exposures across populations.
Summary
The use of WBE offers a near real-time approach to address public health priorities, with strong evidence suggesting it can be applied to generate population-level environmental exposure assessments. Research gaps such as biomarker selection, near real-time intervention efficacy assessment, and data analysis approaches are identified in this review and encouraged to be addressed in future work, informing key areas to support the use of WBE towards a precision-based model for environmental public health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human populations are persistently exposed to a variety of environmental pollutants, with complex structural and individual factors influencing one’s susceptibility to exposure and vulnerability to disease [1]. Globally, it is estimated that one quarter of all deaths per year are related to unhealthy environments, with air, water, and soil pollution serving as vital environmental risk factors contributing to these premature deaths and morbidities [2]. Increasing natural disaster events and other related impacts from climate change are exacerbating these risks, facilitating more severe consequences at unprecedented rates, and more greatly impacting vulnerable communities, leading to disparate health outcomes across populations and contributing to the complexities of understanding environmental causes of disease and death [2, 3].
Human biomonitoring (HBM) strategies have traditionally been implemented at both individual- and population-level to measure and assess human exposures to pollutants in environmental and occupational settings and related health impacts [4, 5]. This technique generally relies on the collection of individualized human biological specimens (e.g., urine, blood) which are then analyzed for a selection of chemical contaminants and may also be supported by self-reported surveys [4]. While HBM provides useful and pertinent information for understanding human health outcomes as it relates to environmental conditions and exposures, these methods are often faced with limitations such as high costs and sampling biases, indicating a greater need to integrate alternative methods that can overcome these challenges to acquiring human exposure data [6].
Wastewater-based epidemiology (WBE) has proven to be a remarkable tool to support public health strategies by generating near real-time, inclusive, and minimally invasive population-level exposure and health assessments, and has undergone significant growth and advancement as a scientific discipline in recent years [7]. The use of community wastewater as a source of public health information is accomplished by analyzing captured human excreted biomarkers (i.e., urine, stool) contributed from populations in composited wastewater that are indicative of various aspects of human health, behavior, exposure, and activity [7,8,9]. Used as a complementary data source alongside current methods, these quantitative and objective community-level assessments can be used to support evidenced-based decision making, offer novel insights into efficient and effective resource deployment, and drive positive policy change [10]. In the early 2000s, WBE was most widely recognized as an informative tool for monitoring population-level trends in substance use, however, it was not until the COVID-19 global pandemic where SARS-CoV-2 monitoring in wastewater to support rapid and targeted public health strategies launched significant acceptance of the field that continues to evolve as public health priorities shift, particularly within the context of infectious diseases [11, 12].
As the world continues to experience more frequent and severe climate-change events, current HBM methods for assessing the human–environment interface will continue to be challenged, thus, the use of wastewater as an inclusive, community-level approach to biomonitoring to understand the human condition as a function of our surrounding environment may serve as a viable candidate to complement existing efforts and support a precision-based model for environmental public health. This narrative review summarizes the pre-pandemic success of applying WBE within the context of environmental epidemiology and exposure assessment, highlights recent and notable findings that significantly contribute to advancing the scientific rigor of the field, and identifies key areas to encourage further investigation and engagement.
Wastewater-Based Epidemiology: A Brief Historical Review
The overall concept of using wastewater to detect a potential threat in support of public health surveillance is not new, as early demonstrations of using community wastewater to trace pathogen outbreaks occurred over a century ago [13]. Wastewater was also used to support surveillance strategies for outbreaks of poliovirus and enterovirus in the early 1960s [14, 15], and later used to continuously assess immunization campaign efficacy for poliovirus in Havana, Cuba in the late 1990s [16]. Despite this, it was not until 2001 where this concept was more formally introduced as a scientific discipline, adopting the term “Sewage Chemical Information Mining (SCIM),” and was proposed as a non-intrusive and anonymous approach to acquire population-level data for illicit substance use through the analysis of chemical residues in wastewater[8]. Rigorous scientific and technical development of the methodology subsequently commenced that encompassed a wide range of applications, including measuring particular environmental contaminants such as pesticides [17, 18], pharmaceuticals [19,20,21], personal care products [22, 23], plasticizers [24], diet and dietary-related constituents [25,26,27,28], and licit and illicit substances (tobacco, alcohol, cannabis, opioids) [29,30,31,32,33,34,35,36,37] in untreated, influent wastewater to understand trends in population-level exposure and burden. Highly debated topics amongst experts in the field were rigorously evaluated to establish best practice protocols, which included methods for estimating population size (i.e., population normalization) [38,39,40,41], back-calculations for determining consumption, dose, and/or exposure rates to enhance data interpretation [42, 43], and early conversations that considered the potential ethical implications of WBE, particularly in the realm of substance use [10]. Globally-recognized WBE programs, such as the Sewage Analysis Core Group (SCORE), were implemented to monitor city-level trends of substance use and encourage the establishment of standardized sample collection, laboratory processing, and analysis protocols amongst WBE practitioners [11, 44].
Despite this progress, the use of WBE to operate in parallel with clinical or case-based surveillance methods as a complementary data source was not common practice and remained relatively siloed as a niche consortium of researchers until the COVID-19 global pandemic. The initial stages of the pandemic highlighted vulnerabilities in the global response to a novel viral outbreak, and identified a clear need for alternative strategies that were able to operate at a comparable pace to the rapid rate of viral transmission within and across populations [45]. This positioned WBE as a prime candidate given its historical success of providing rapid and objective information of population-level activity and exposures, prompting global initiatives and interdisciplinary partnerships to encourage rapid development and deployment of methods for SARS-CoV-2 monitoring in wastewater, employing a new wave of experts within the field such as environmental microbiologists [12]. Collectively, these efforts brought unprecedented attention and interest to the field that offered widespread acceptance for inclusion into the public health model. Major scientific contributions as a result included quantifying the early-warning capabilities of using wastewater to detect viral presence and monitor transmission within and between communities in near real-time [46], the ability to determine hotspots of infection in areas that would have otherwise been undetected with individualized testing methods [45], and identified WBE as an efficient and cost-effective approach to obtaining public health data [47]. Transitioning into a post-COVID-19 era, continuous advancements in methodology has allowed for the successful expansion to other pathogen targets, such as influenza, respiratory syncytial virus, and Mpox virus, all of which have either been onboarded into national surveillance systems, or are in process of such [48], thus opening up the opportunity to address other urgent public health priorities, such as antimicrobial resistance [49,50,51,52,53]. While the use of WBE to support global COVID-19 surveillance is one of the first major demonstrations of broad acceptance and implementation alongside public health strategies, it is important to acknowledge the pre-pandemic efforts that, in part, contributed to that success, and further, leverage the recent lessons learned to continue momentum in gaining an in-depth understanding of utilizing WBE to assess environmental exposures and related health outcomes in human populations.
Bridging the Past to Present in Using WBE for Environmental Exposure Assessments
The era of using WBE to measure and assess trends of population-level exposure to environmental pollutants began in the early-mid 2000s, in parallel with other prominent and rapidly develo** applications such as substance use. The dominant processing and analytical pipeline for measuring chemical analytes in untreated wastewater typically begins with solid phase extraction followed by liquid chromatography-tandem mass spectrometry (LC–MS/MS) [31]. Successful investigations thus far include a wide range of chemical constituents, including pesticides, pharmaceuticals, plasticizers, xenoestrogens, flame retardants, nicotine, heavy metals, and mycotoxins (Table 1).
One pioneering study reported the measurement of Salbutamol, a commonly prescribed short-acting beta-agonist (SABA) for asthma patients and compared to select air pollutants and other environmental conditions (PM10 and PM2.5, ozone, nitrogen dioxide, sulfur dioxide, benzene, relative humidity, and temperature) in overlap** regions. Results from this work revealed strong positive correlations between the wastewater-derived daily consumed dose of Salbutamol and reported concentrations of PM10 and PM2.5 [54, 55]. Briefly, to achieve this, measured concentrations in wastewater were transformed to a population-normalized mass load of the chemical analyte, then divided by the product of the metabolic excretion rate of Salbutamol reported in literature and the defined daily dose (DDD) reported by the World Health Organization (WHO)) [55]. This was amongst one of the first to report comparisons between WBE measurements of asthma-related medication and external data sets of pollutant concentrations to assess trends and provide epidemiological insights into the human health impacts of air pollution. To date, there has yet to be a similar study with this level of novelty, though it is heavily encouraged to continue to explore this in future work [56].
Biomarker selection is a crucial aspect of successfully conducting WBE, particularly for human specificity reasons. Wastewater is a complex matrix that may contain contributions from humans as well as industrial or commercial inputs, environmental runoff, or even animals in some instances [57]. Additionally, within-sewer metabolite transformations and degradation as a result from microbial activity and biofilm formation is also a common factor of uncertainty known within the field [58]. Thus, a rigorous investigation of these characteristics is necessary to interpret WBE data most accurately as a function of human population activity, exposure, and behavior. One study demonstrated this by critically evaluating several metabolites of certain classes of pesticides (triazines, organophosphates, pyrethroids) based on human specificity to serve as potential biomarkers for the assessment of population pesticide exposure in over 40 influent wastewater samples from wastewater treatment plants (WWTPs) across cities in Italy [17]. Wastewater-derived reported concentrations were similar to HBM reports of the same analytes in human urine, with the highest concentrations in the organophosphate group, followed by pyrethroids, then triazines. These results were consistent with agricultural practices, suggesting that the data derived from wastewater served as a rapid, comprehensive, and accurate source of population-level exposure data which could, in future work, inform policy structures to assist in mitigating these exposures [17]. Subsequently, a similar study was conducted in Norway where spatial differences between pyrethroids and organophosphates were observed, and select analyte measurements were also comparable to HBM studies in urine, strengthening this application of WBE [59].
Reports of using WBE to assess human exposure to environmental pollutants include measuring phosphorous flame retardants and plasticizers (PFRs), where measured loads of PFRs in wastewater were in alignment with HBM studies in urine [60, 61], as well as wastewater measurements of phthalate plasticizers, bisphenols, triclosan, and nicotine [24, 31, 32, 62]. Notably, in a novel approach to WBE, a recent study explored the feasibility of measuring population-level exposure to over twenty heavy metals using inductively coupled plasma quadrupole mass spectrometry (ICP-MS) in twenty-six sample locations across a single county within Kentucky, USA. Variability in measurements between catchments indicate potential differential exposure across populations, particularly in sampled locations with known risks for adverse environmental exposures, suggesting the use of wastewater to understand environmental exposures and health equity is feasible, and should warrant further investigation [63] (Table 1).
Collectively, these reports demonstrate profound competency for the ability of WBE to assess environmental pollutant exposure within human populations and serve as a strong platform to facilitate continued investigation and expansion. Given the limitations of traditional HBM methods and techniques, WBE appears well-positioned to provide population-level, near real-time, objective, and inclusive epidemiological information. Recent studies have acknowledged this potential and have elected WBE to be utilized in an integrated WBE-HBM model to encourage ‘One Health’ initiatives, as well as a complementary data source for assessing the community-level exposome [56, 64]. Despite this recent progress, there remain several key gaps in our current understanding of how WBE can continue to progress to accomplish these newly proposed models.
Addressing Key Gaps in Future Implementation
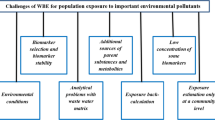
There are several focal points that must be addressed in future work to continue to advance the field of WBE in the context of environmental contaminant exposures, which are summarized in Fig. 1. First, further testing of potential biomarkers to expand current knowledge of what is possible to assess in wastewater to indicate human exposure and subsequent metabolism is needed. This will involve investigating the stability and human specificity of existing biomarkers, as well as proposing new biomarker targets. Additionally, leveraging wastewater-derived measurements to make stronger epidemiological connections to human health outcomes is needed. This was preliminarily accomplished in a few studies (Table 1), for example, the associations reported between increased wastewater measurements of Salbutamol and increased concentrations of select air pollutants, serving as a strong platform to assess this observation with other metabolites [55]. Incorporating endogenous biomarkers that may indicate acute human physiological disruption due to an exposure to a pollutant and are measured in tandem with exogenous stressors may serve to fill this gap, such as biomarkers of inflammation or stress hormones [9, 57, 65]. Conceptually, these sewage-borne biomarkers would all be measured as a unified suite, which could bolster interpretations of investigating population-level exposure and contextualize the direct human impact.
The field of WBE is inherently interdisciplinary, which has been continuously demonstrated in multiple applications. However, engaging in partnerships with formally trained epidemiologists with a diverse portfolio of specialization (e.g., environmental, infectious disease) is lacking. While this was evident during COVID-19, encouraging these partnerships in the context of environmentally influenced illnesses from chemical pollutant exposure is recommended. Additionally, experts in qualitative and community-based participatory methods will serve to transform quantitative results into meaningful and contextualized information and may strengthen epidemiological insights and drive relevant policy change. Reports of comparing wastewater data with comparable datasets informing social vulnerability and other socio-demographic data demonstrate these are important factors to properly interpret and assess WBE data [66,67,68]. Inquiring community need and chief concerns prior to study implementation may assist to support matters of environmental injustice and health disparities, highlighting the non-intrusive and inclusive benefits of conducting a community-scale human biomonitoring assessment, promote citizen engagement, and overall contribute irrefutable power behind the reported results. Encouraging cooperative studies where primary data collection between different methods is employed simultaneously could significantly enhance comparative assessments between data sets. For example, this could include measuring indicators of air pollution in wastewater, such as asthma medications as proxy, and compare to data collected by air pollution monitors or sensors distributed in overlap** catchments.
Recent advances in analytical techniques harnessing untargeted and large-molecule analyses of wastewater could serve to unlock tremendous potential for understanding the many pollutants human populations encounter daily, and resultant physiological impacts. This has been proposed on several recent occasions within the field spanning several applications, such as non-targeted drug analysis and suspect screening for cancer in community sewage [57, 69, 70]. These methods could be adopted in the context of environmental exposures, with subsequent rigorous critical evaluation of onboarding protein biomarkers to assess human impact [57, 71, 72]. However, given the exploratory nature of this analytical technique, careful consideration of potential unique limitations to this type of methodological approach is recommended.
A major strength of WBE is the ability to continuously assess population-level trends in near real-time that is often a fraction of operating costs of traditional HBM methods, affording the ability to rapidly inform intervention efficacy. While this was demonstrated during COVID-19, reports of this are lacking with relation to environmental contaminants. Sample collection within the sewer infrastructure as opposed to macro-level collection, such as from a WWTP, can serve to accomplish this. Pre-pandemic reports of conducting WBE at neighborhood- or building-level were rare, however, this shifted in response to the need for greater spatial resolution to track rapid viral transmission [73]. With greater acceptance of monitoring at this scale, this can be expanded to chemical targets of environmental origin. Of course, being mindful of potential ethical implications of conducting neighborhood-level or near-source applications is crucial in order to not only protect the privacy of the community, but also the integrity of the field [74]. Overall, these key areas share similar overarching themes of enhancing back-calculation strategies for estimating human excretion and dose of exposure or consumption, as well as evaluating stability of each biomarker in several circumstances to inform appropriate correction factors and improve interpretations by WBE. These studies are listed in Table 1, which summarizes the biomarkers/environmental exposures selected, notable reported conclusions, and important limitations to consider in future experimental work.
A Call to Action to Encourage Broader Engagement and Continued Expansion
These identified gaps serve to support a call to action for broader engagement of experts who can address these areas in collaborative research partnerships using WBE to assess population-level environmental exposures (Fig. 1). As demonstrated for substance use and COVID-19 monitoring, the use of WBE is most useful when implemented in team-based interdisciplinary groups to offer enhanced insights and interpretations to WBE-derived data and provide sound conclusions and recommendations to influence policy and informed decision making. This approach may serve to continue to advance the field as well as provide increasingly impactful solutions for global issues. It is greatly encouraged for community-leaders, epidemiologists, policy experts, and advocates for environmental justice and health equity to engage with current WBE practitioners to offer valuable context and unique perspectives to wastewater measurements and overall produce meaningful results that aim to support the health and integrity of our populations and the environment.
Conclusion
Wastewater-based epidemiology has proven to serve as a comprehensive, adaptable, cost-effective, and inclusive source of public health information in a variety of applications. Historical efforts of using this methodology for substance use monitoring enabled rapid deployment of SARS-CoV-2 surveillance within populations across the globe that support public health mitigation strategies. Strong evidence suggests this approach can successfully address the growing incidence of environmentally influenced adverse health outcomes as impacts from climate change and persistent toxic chemicals continue to pose a significant threat to the health of our societies and surrounding environments. Careful consideration of the key gaps identified to inform future investigation is needed to continue to advance the field of WBE in this area in support of moving towards a precision-based model for environmental public health.
References
Noppert GA, Hegde ST, Kubale JT. Exposure, susceptibility, and recovery: a framework for examining the intersection of the social and physical environments and infectious disease risk. Am J Epidemiol. 2023;192(3):475–82. https://doi.org/10.1093/aje/kwac186.
Pruss-Ustun A, Wolf J, Corvalan C, Bos R, Neira M. Preventing disease through healthy environments: a global assessment of the burden of disease from environmental risks. World Health Organization; 2018. p. 147.
EPA. Climate change and social vulnerability in the United States: a focus on six impacts. U.S. Environmental Protection Agency. 2021.
Bocato MZ, et al. An overview of the current progress, challenges, and prospects of human biomonitoring and exposome studies. J Toxicol Environ Health B Crit Rev. 2019;22(5–6):131–56. https://doi.org/10.1080/10937404.2019.1661588.
Virgolino A, et al. Challenges to Evidence Synthesis and Identification of Data Gaps in Human Biomonitoring. Int J Environ Res Public Health. 2021;18(6):2830.
Rousis NI, et al. Wastewater-based epidemiology to assess pan-European pesticide exposure. Water Res. 2017;121:270–9.
Daughton CG. Monitoring wastewater for assessing community health: Sewage Chemical-Information Mining (SCIM). Sci Total Environ. 2018;619–620:748–64. https://doi.org/10.1016/j.scitotenv.2017.11.102.
Daughton CG. Illicit drugs in Municipal Sewage. In: Pharmaceuticals and care products in the environment. American Chemical Society; 2001. p. 348–64.
Vitale D, Morales Suárez-Varela M, Picó Y. Wastewater-based epidemiology, a tool to bridge biomarkers of exposure, contaminants, and human health. Curr Opin Environ Sci Health. 2021;20:100229. https://doi.org/10.1016/j.coesh.2021.100229.
Prichard J, et al. Ethical research guidelines for wastewater-based epidemiology and related fields. Sewage Analysis Core Group Europe (SCORE). 2016;1–13.
SCORE. Bringing together experts and knowledge on wastewater-based epidemiology. 2011. 2024; Available from: https://score-network.eu. Accessed 5 Mar 2024
Bivins A, et al. Wastewater-based epidemiology: global collaborative to maximize contributions in the fight against COVID-19. Environ Sci Technol. 2020;54(13):7754–7. https://doi.org/10.1021/acs.est.0c02388.
Tulchinsky TH. John Snow, Cholera, the Broad Street Pump; waterborne diseases then and now. Case Studies in Public Health, 2018;77–99. https://doi.org/10.1016/b978-0-12-804571-8.00017-2.
Böttiger M. Experiences from investigations of virus isolations from sewage over a two year period with special regard to polioviruses. Arch Gesamte Virusforsch. 1973;41(1):80–5. https://doi.org/10.1007/bf01249932.
Gravelle CR, Chin TDY. Enterovirus Isolations from Sewage Comparison of Three Methods*. J Infect Dis. 1961;109(2):205–9. https://doi.org/10.1093/infdis/109.2.205.
Lago PM, et al. Poliovirus detection in wastewater and stools following an immunization campaign in Havana, Cuba. Int J Epidemiol. 2003;32(5):772–7. https://doi.org/10.1093/ije/dyg185.
Rousis NI, Zuccato E, Castiglioni S. Monitoring population exposure to pesticides based on liquid chromatography-tandem mass spectrometry measurement of their urinary metabolites in urban wastewater: A novel biomonitoring approach. Sci Total Environ. 2016;571:1349–57. https://doi.org/10.1016/j.scitotenv.2016.07.036.
Rousis NI, Zuccato E, Castiglioni S. Wastewater-based epidemiology to assess human exposure to pyrethroid pesticides. Environ Int. 2017;99:213–20. https://doi.org/10.1016/j.envint.2016.11.020.
Castiglioni S, et al. A multiresidue analytical method using solid-phase extraction and high-pressure liquid chromatography tandem mass spectrometry to measure pharmaceuticals of different therapeutic classes in urban wastewaters. J Chromatogr A. 2005;1092(2):206–15. https://doi.org/10.1016/j.chroma.2005.07.012.
Escolà Casas M, et al. Showcasing the potential of wastewater-based epidemiology to track pharmaceuticals consumption in cities: Comparison against prescription data collected at fine spatial resolution. Environ Int. 2021;150:106404. https://doi.org/10.1016/j.envint.2021.106404.
Burgard DA, et al. Potential trends in Attention Deficit Hyperactivity Disorder (ADHD) drug use on a college campus: Wastewater analysis of amphetamine and ritalinic acid. Sci Total Environ. 2013;450–451:242–9. https://doi.org/10.1016/j.scitotenv.2013.02.020.
Lopardo L, et al. Verifying community-wide exposure to endocrine disruptors in personal care products - In quest for metabolic biomarkers of exposure via in vitro studies and wastewater-based epidemiology. Water Res. 2018;143:117–26. https://doi.org/10.1016/j.watres.2018.06.028.
Lopardo L, et al. Estimation of community-wide exposure to bisphenol A via water fingerprinting. Environ Int. 2019;125:1–8. https://doi.org/10.1016/j.envint.2018.12.048.
González-Mariño I, et al. Wastewater-based epidemiology as a new tool for estimating population exposure to phthalate plasticizers. Environ Sci Technol. 2017;51(7):3902–10. https://doi.org/10.1021/acs.est.6b05612.
Choi PM, et al. Do food and stress biomarkers work for wastewater-based epidemiology? A critical evaluation. Sci Total Environ. 2020;736:139654. https://doi.org/10.1016/j.scitotenv.2020.139654.
Berzina Z, et al. Application of wastewater-based epidemiology for tracking human exposure to deoxynivalenol and enniatins. Toxins (Basel) 2022;14(2). https://doi.org/10.3390/toxins14020091. Findings from this study suggest that use of WBE to assess population-level exposure to mycotoxins is feasible, using enniatins and deoxynivalenol as prototype targets.
Gracia-Lor E, et al. Wastewater-based epidemiology for tracking human exposure to mycotoxins. J Hazard Mater. 2020;382:121108. https://doi.org/10.1016/j.jhazmat.2019.121108.
Venkatesan AK, et al. Assessing the Potential To Monitor Plant-Based Diet Trends in Communities Using a Wastewater-Based Epidemiology Approach. In: Wastewater-based epidemiology: estimation of community consumption of drugs and diets. American Chemical Society; 2019. p. 187–98.
Baz-Lomba JA, et al. Comparison of pharmaceutical, illicit drug, alcohol, nicotine and caffeine levels in wastewater with sale, seizure and consumption data for 8 European cities. BMC Public Health. 2016;16(1):1035. https://doi.org/10.1186/s12889-016-3686-5.
Castiglioni S, et al. A novel approach for monitoring tobacco use in local communities by wastewater analysis. Tob Control. 2015;24(1):38–42. https://doi.org/10.1136/tobaccocontrol-2014-051553.
Chen J, Venkatesan AK, Halden RU. Alcohol and nicotine consumption trends in three U.S. communities determined by wastewater-based epidemiology. Sci Total Environ. 2019;656:174–83. https://doi.org/10.1016/j.scitotenv.2018.11.350.
Driver EM, et al. Alcohol, nicotine, and caffeine consumption on a public U.S. university campus determined by wastewater-based epidemiology. Sci Total Environ. 2020;727:138492. https://doi.org/10.1016/j.scitotenv.2020.138492.
Banta-Green CJ, et al. The spatial epidemiology of cocaine, methamphetamine and 3,4-methylenedioxymethamphetamine (MDMA) use: a demonstration using a population measure of community drug load derived from municipal wastewater. Addiction. 2009;104(11):1874–80. https://doi.org/10.1111/j.1360-0443.2009.02678.x.
van Dyken E, et al. Monitoring substance use in prisons: Assessing the potential value of wastewater analysis. Sci Justice. 2014;54(5):338–45. https://doi.org/10.1016/j.scijus.2014.06.006.
Zuccato E, et al. Estimating community drug abuse by wastewater analysis. Environ Health Perspect. 2008;116(8):1027–32. https://doi.org/10.1289/ehp.11022.
Gushgari AJ, et al. Tracking narcotics consumption at a Southwestern U.S. university campus by wastewater-based epidemiology. J Hazard Mater. 2018;359:437–44. https://doi.org/10.1016/j.jhazmat.2018.07.073.
Ort C, et al. Spatial differences and temporal changes in illicit drug use in Europe quantified by wastewater analysis. Addiction. 2014;109(8):1338–52. https://doi.org/10.1111/add.12570.
Daughton CG. Real-time estimation of small-area populations with human biomarkers in sewage. Sci Total Environ. 2012;414:6–21. https://doi.org/10.1016/j.scitotenv.2011.11.015.
Chen C, et al. Towards finding a population biomarker for wastewater epidemiology studies. Sci Total Environ. 2014;487:621–8. https://doi.org/10.1016/j.scitotenv.2013.11.075.
Thomas KV, et al. Use of mobile device data to better estimate dynamic population size for wastewater-based epidemiology. Environ Sci Technol. 2017;51(19):11363–70. https://doi.org/10.1021/acs.est.7b02538.
Rico M, Andrés-Costa MJ, Picó Y. Estimating population size in wastewater-based epidemiology. Valencia metropolitan area as a case study. J Hazard Mater. 2017;323(Pt A):156–65. https://doi.org/10.1016/j.jhazmat.2016.05.079.
Gracia-Lor E, Zuccato E, Castiglioni S. Refining correction factors for back-calculation of illicit drug use. Sci Total Environ. 2016;573:1648–59. https://doi.org/10.1016/j.scitotenv.2016.09.179.
van Nuijs ALN, et al. Sewage epidemiology — A real-time approach to estimate the consumption of illicit drugs in Brussels Belgium. Environ Int. 2011;37(3):612–21. https://doi.org/10.1016/j.envint.2010.12.006.
(EMCDDA), E.M.C.f.D.a.D.A. 1995; Available from: https://www.emcdda.europa.eu/index_en. Accessed 13 Mar 2024
Bowes DA, et al. Leveraging an established neighbourhood-level, open access wastewater monitoring network to address public health priorities: a population-based study. The Lancet Microbe. 2023;4(1):e29–37. https://doi.org/10.1016/S2666-5247(22)00289-0.
Olesen SW, Imakaev M, Duvallet C. Making waves: Defining the lead time of wastewater-based epidemiology for COVID-19. Water Res. 2021;202:117433. https://doi.org/10.1016/j.watres.2021.117433.
Wright J, et al. Comparison of high-frequency in-pipe SARS-CoV-2 wastewater-based surveillance to concurrent COVID-19 random clinical testing on a public U.S. university campus. Sci Total Environ. 2022;152877. https://doi.org/10.1016/j.scitotenv.2021.152877.
CDC. National wastewater surveillance system (NWSS). 2023 November 28, 2023; Available from: https://www.cdc.gov/nwss/about.html. Accessed 13 Mar 2024
Robins K, et al. Research needs for optimising wastewater-based epidemiology monitoring for public health protection. J Water Health. 2022;20(9):1284–313. https://doi.org/10.2166/wh.2022.026.
Sims N, Kasprzyk-Hordern B. Future perspectives of wastewater-based epidemiology: Monitoring infectious disease spread and resistance to the community level. Environ Int. 2020;139:105689. https://doi.org/10.1016/j.envint.2020.105689.
Holton E, et al. Quantifying community-wide antimicrobials usage via wastewater-based epidemiology. J Hazard Mater. 2022;436:129001. https://doi.org/10.1016/j.jhazmat.2022.129001.
Su J-Q, et al. Metagenomics of urban sewage identifies an extensively shared antibiotic resistome in China. Microbiome. 2017;5(1):84. https://doi.org/10.1186/s40168-017-0298-y.
Holton E, et al. Quantifying community-wide antibiotic usage via urban water fingerprinting: Focus on contrasting resource settings in South Africa. Water Res. 2023;240:120110. https://doi.org/10.1016/j.watres.2023.120110.
Castiglioni S, et al. Testing wastewater to detect illicit drugs: State of the art, potential and research needs. Sci Total Environ. 2014;487:613–20. https://doi.org/10.1016/j.scitotenv.2013.10.034.
Fattore E, et al. Wastewater-based epidemiological evaluation of the effect of air pollution on short-acting beta-agonist consumption for acute asthma treatment. Environ Res. 2016;150:106–11. https://doi.org/10.1016/j.envres.2016.05.051.
Kasprzyk-Hordern B, et al. Wastewater-based epidemiology for the assessment of population exposure to chemicals: The need for integration with human biomonitoring for global One Health actions. J Hazard Mater. 2023;450:131009. https://doi.org/10.1016/j.jhazmat.2023.131009.
Picó Y, Barceló D. Identification of biomarkers in wastewater-based epidemiology: Main approaches and analytical methods. TrAC Trends Anal Chem. 2021;145:116465. https://doi.org/10.1016/j.trac.2021.116465.
Gao Z, et al. Biomarker selection strategies based on compound stability in wastewater-based epidemiology. Environ Sci Pollut Res. 2023;30(3):5516–29. https://doi.org/10.1007/s11356-022-24268-y.
Rousis NI, et al. Assessment of human exposure to selected pesticides in Norway by wastewater analysis. Sci Total Environ. 2020;723:138132. https://doi.org/10.1016/j.scitotenv.2020.138132.
Been F, et al. Mining the chemical information on urban wastewater: monitoring human exposure to phosphorus flame retardants and plasticizers. Environ Sci Technol. 2018;52(12):6996–7005. https://doi.org/10.1021/acs.est.8b01279.
Been F, et al. Liquid chromatography-tandem mass spectrometry analysis of biomarkers of exposure to phosphorus flame retardants in wastewater to monitor community-wide exposure. Anal Chem. 2017;89(18):10045–53. https://doi.org/10.1021/acs.analchem.7b02705.
Kasprzyk-Hordern B, et al. Estimation of community-wide multi-chemical exposure via water-based chemical mining: Key research gaps drawn from a comprehensive multi-biomarker multi-city dataset. Environ Int. 2021;147:106331. https://doi.org/10.1016/j.envint.2020.106331.
Cai L, et al. Wastewater-based epidemiology for comprehensive communitywide exposome surveillance: A gradient of metals exposure. medRxiv. 2023. https://doi.org/10.1101/2023.09.26.23295844. Findings from this study suggests the use of WBE to assess community-level exposure to heavy metals is feasible, proposing a novel analytical method and identifying differential exposure across selected sewersheds, pointing towards a precision-based approach for addressing matters of environmental injustice.
Stingone, J.A., et al., Community-level exposomics: a population-centered approach to address public health concerns. Exposome. 2023;3(1). https://doi.org/10.1093/exposome/osad009.
Driver EM, et al. Assessing population-level stress through glucocorticoid hormone monitoring in wastewater. Sci Total Environ. 2022;838:155961. https://doi.org/10.1016/j.scitotenv.2022.155961.
Choi PM, et al. Social, demographic, and economic correlates of food and chemical consumption measured by wastewater-based epidemiology. Proc Natl Acad Sci. 2019;116(43):21864–73. https://doi.org/10.1073/pnas.1910242116.
Lancaster E, et al. Socioeconomic status correlations with confirmed COVID-19 cases and SARS-CoV-2 wastewater concentrations in small-medium sized communities. Environ Res. 2022;215(Pt 2):114290. https://doi.org/10.1016/j.envres.2022.114290.
Saingam P, et al. Integrating socio-economic vulnerability factors improves neighborhood-scale wastewater-based epidemiology for public health applications. Water Res. 2024;254:121415. https://doi.org/10.1016/j.watres.2024.121415.
Lorenzo M, Picó Y. Wastewater-based epidemiology: current status and future prospects. Curr Opin Environ Sci Health. 2019;9:77–84. https://doi.org/10.1016/j.coesh.2019.05.007.
Ferrando-Climent L, et al. Identification of markers of cancer in urban sewage through the use of a suspect screening approach. J Pharm Biomed Anal. 2016;129:571–80. https://doi.org/10.1016/j.jpba.2016.08.001.
Carrascal M, et al. Discovery of large molecules as new biomarkers in wastewater using environmental proteomics and suitable polymer probes. Sci Total Environ. 2020;747:141145. https://doi.org/10.1016/j.scitotenv.2020.141145.
Perez-Lopez C, et al. Non-target protein analysis of samples from wastewater treatment plants using the regions of interest-multivariate curve resolution (ROIMCR) chemometrics method. J Environ Chem Eng. 2021;9(4):105752. https://doi.org/10.1016/j.jece.2021.105752.
Spurbeck RR, Minard-Smith A, Catlin L. Feasibility of neighborhood and building scale wastewater-based genomic epidemiology for pathogen surveillance. Sci Total Environ. 2021;789:147829. https://doi.org/10.1016/j.scitotenv.2021.147829.
Bowes DA, et al. Structured ethical review for wastewater-based testing in support of public health. Environ Sci Technol. 2023;57(35):12969–80. https://doi.org/10.1021/acs.est.3c04529.
Tang S, et al. Urinary concentrations of bisphenols in the Australian population and their association with the per capita mass loads in wastewater. Environ Sci Technol. 2020;54(16):10141–8. https://doi.org/10.1021/acs.est.0c00921.
Funding
Open access funding provided by the Carolinas Consortium. DAB is currently funded by the NIH Common Fund through the Office of the Director, National Institutes of Health (OD) and under Award Number U54CA272171. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
DAB – conceptualization, methodology, literature review and analysis, writing-original draft, writing-editing and revision, critical evaluation of the reported work.
Corresponding author
Ethics declarations
Financial Interests
The author has no relevant financial or non-financial interests to disclose.
Competing Interests
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bowes, D.A. Towards a Precision Model for Environmental Public Health: Wastewater-based Epidemiology to Assess Population-level Exposures and Related Diseases. Curr Epidemiol Rep (2024). https://doi.org/10.1007/s40471-024-00350-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s40471-024-00350-6