Abstract
Helicobacter pylori is the main etiopathogenetic factor of chronic gastritis, peptic ulcer disease and gastric cancer. The world’s population is shifting towards older people, who have the highest prevalence of H. pylori. Aging-related peculiarities could have an impact on the treatment of H. pylori and there is still a lack of research data in the older population. The aim of this review was to summarize the findings of the most recent information, publications and studies on the issues relating to H. pylori infection in older patients. H. pylori eradication offers gastrointestinal and extra gastrointestinal benefits in older patients. Based on the main guidelines, H. pylori should be eradicated independent of the patient’s age, only reconsidering cases with terminal illness and low life expectancy. Proton pump inhibitors are generally safe and well tolerated. Some antibiotics require dose adjustment only in advanced renal insufficiency and the risk of hepatotoxicity is very low. Special precautions should be taken in patients with polypharmacy and those taking aspirin or non-steroidal anti-inflammatory drugs. In older patients, H. pylori eradication treatment frequently causes only mild and short-term adverse events; however, treatment compliance is usually still very good. H. pylori treatment in older patients does not increase the risk of Clostridium difficile infection. Optimal eradication effectiveness (> 90%) is mostly achieved with bismuth- and non-bismuth-based quadruple therapies. Susceptibility-guided treatment of H. pylori can contribute to increasing the effectiveness of eradication regimens in older adults. To achieve optimal H. pylori eradication effectiveness in older patients, the same guidelines, which are applied to adults, also apply to this population: avoiding repetitive treatment prescriptions, choosing quadruple therapies, prescribing longer treatment duration and administering high-dose proton pump inhibitors twice daily.

Similar content being viewed by others
References
Mitchell E, Walker R. Global ageing: successes, challenges and opportunities. Br J Hosp Med. 2020;81(2):1–9.
World Health Organization (WHO). Ageing and Health. 2022 [cited 2023 Sep 3]. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health. Accessed on 3 Sept 2023.
United Nations (UN). Older persons. 2023 [cited 2023 Sep 3]. https://emergency.unhcr.org/protection/persons-risk/older-persons. Accessed on 3 Sept 2023.
Singh S, Bajorek B. Defining, “Elderly” in Clinical Practice Guidelines for Pharmacotherapy. Pharm Pract (Granada). 2014;12(4):489.
Sieber CC. The elderly patient—who is that? Internist (Berl). 2007;48(11):1190,1192-11901194.
Kobayashi S, Joshita S, Yamamoto C, Yanagisawa T, Miyazawa T, Miyazawa M, et al. Efficacy and safety of eradication therapy for elderly patients with Helicobacter pylori infection. Medicine (Baltimore). 2019;98(30): e16619.
Liu T. Super-aging and Social Security for the Most Elderly in China. Z Gerontol Geriatr. 2018;51(1):105–12.
Narayanan M, Reddy KM, Marsicano E. Peptic ulcer disease and Helicobacter pylori infection. Mo Med. 2018;115(3):219–24.
Senchukova MA, Tomchuk O, Shurygina EI. Helicobacter pylori in gastric cancer: features of infection and their correlations with long-term results of treatment. World J Gastroenterol. 2021;27(37):6290–305.
Norwood DA, Montalvan-Sanchez E, Dominguez RL, Morgan DR. Gastric cancer: emerging trends in prevention, diagnosis, and treatment. Gastroenterol Clin N Am. 2022;51(3):501–18.
Malfertheiner P, Megraud F, Rokkas T, Gisbert JP, Liou J-M, Schulz C, et al. Management of Helicobacter pylori infection: the Maastricht VI/Florence consensus report. Gut. 2022;71:1724–62.
Jamkhande PG, Gattani SG, Farhat SA. Helicobacter pylori and cardiovascular complications: a mechanism based review on role of Helicobacter pylori in cardiovascular diseases. Integr Med Res. 2016;5(4):244–9.
Kountouras J, Boziki M, Polyzos SA, Katsinelos P, Gavalas E, Zeglinas C, et al. The emerging role of Helicobacter pylori-induced metabolic gastrointestinal dysmotility and neurodegeneration. Curr Mol Med. 2017;17(6):389–404.
Tsay F-W, Hsu P-I. H. pylori infection and extra-gastroduodenal diseases. J Biomed Sci. 2018;25(1):65.
Li Y, Choi H, Leung K, Jiang F, Graham DY, Leung WK. Global prevalence of Helicobacter pylori infection between 1980 and 2022: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2023;8(6):553–64.
Hooi JKY, Lai WY, Ng WK, Suen MMY, Underwood FE, Tanyingoh D, et al. Global prevalence of Helicobacter pylori infection: systematic review and meta-analysis. Gastroenterology. 2017;153(2):420–9.
Jonaityte IR, Ciupkeviciene E, Jonaitis P, Kupcinskas J, Petkeviciene J, Jonaitis L. Changes in the seroprevalence of Helicobacter pylori among the Lithuanian medical students over the last 25 years and its relation to dyspeptic symptoms. Medicina. 2021;57(3):254.
Pilotto A, Franceschi M. Helicobacter pylori infection in older people. World J Gastroenterol. 2014;20(21):6364–73.
Peng C, Hu Y, Ge Z-M, Zou Q-M, Lyu N-H. Diagnosis and treatment of Helicobacter pylori infections in children and elderly populations. Chronic Dis Transl Med. 2019;5(4):243–51.
den Hoed CM, Vila AJ, Holster IL, Perez-Perez GI, Blaser MJ, de Jongste JC, et al. Helicobacter pylori and the birth cohort effect: evidence for stabilized colonization rates in childhood. Helicobacter. 2011;16(5):405–9.
Kienesberger S, Perez-Perez GI, Olivares AZ, Bardhan P, Sarker SA, Hasan KZ, et al. When is Helicobacter pylori acquired in populations in develo** countries? A birth-cohort study in Bangladeshi children. Gut Microbes. 2018;9(3):252–63.
Gisbert JP. The recurrence of Helicobacter pylori infection: incidence and variables influencing it. A critical review. Am J Gastroenterol. 2005;100(9):2083–209.
Hu Y, Wan J-H, Li X-Y, Zhu Y, Graham DY, Lu N-H. Systematic review with meta-analysis: the global recurrence rate of Helicobacter pylori. Aliment Pharmacol Ther. 2017;46(9):773–9.
**e Y, Song C, Cheng H, Xu C, Zhang Z, Wang J, et al. Long-term follow-up of Helicobacter pylori reinfection and its risk factors after initial eradication: a large-scale multicentre, prospective open cohort, observational study. Emerg Microbes Infect. 2020;9(1):548–57.
Joo Y-E, Park H-K, Myung D-S, Baik G-H, Shin J-E, Seo G-S, et al. Prevalence and Risk factors of atrophic gastritis and intestinal Metaplasia: a Nationwide Multicenter Prospective Study in Korea. Gut Liver. 2013;7(3):303–10.
Cizginer S, Ordulu Z, Kadayifci A. Approach to Helicobacter pylori infection in geriatric population. World J Gastrointest Pharmacol Ther. 2014;5(3):139–47.
Huang Q, Jia X, Chu Y, Zhang X, Ye H. Helicobacter pylori infection in geriatric patients: current situation and treatment regimens. Front Med. 2021;8: 713908.
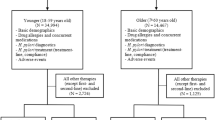
Jonaitis P, Nyssen OP, Saracino IM, Fiorini G, Vaira D, Pérez-Aísa Á, et al. Comparison of the management of helicobacter pylori infection between the older and younger European Populations. Sci Rep. 2023;13(1):17235.
Ganda Mall J-P, Östlund-Lagerström L, Lindqvist CM, Algilani S, Rasoal D, Repsilber D, et al. Are self-reported gastrointestinal symptoms among older adults associated with increased intestinal permeability and psychological distress? BMC Geriatr. 2018;18(1):75.
Pilotto A, Maggi S, Noale M, Franceschi M, Parisi G, Crepaldi G. Association of upper gastrointestinal symptoms with functional and clinical charateristics in elderly. World J Gastroenterol. 2011;17(25):3020–6.
Amarya S, Singh K, Sabharwal M. Ageing Process and Physiological Changes. In: D’Onofrio G, Greco A, Sancarlo D, editors. Gerontology. Rijeka: IntechOpen; 2018. Available at: https://doi.org/10.5772/intechopen.76249
Alvis BD, Hughes CG. Physiology Considerations in Geriatric Patients. Anesthesiol Clin. 2015;33(3):447–56.
Shruthi R, Jyothi R, Pundarikaksha HP, Nagesh GN, Tushar TJ. A study of medication compliance in geriatric patients with chronic illnesses at a tertiary care hospital. J Clin Diagnostic Res JCDR. 2016;10(12):FC40–3.
Soenen S, Rayner CK, Jones KL, Horowitz M. The ageing gastrointestinal tract. Curr Opin Clin Nutr Metab Care. 2016;19(1):12–8.
Bhutto A, Morley JE. The clinical significance of gastrointestinal changes with aging. Curr Opin Clin Nutr Metab Care. 2008;11(5):651–60.
Sugano K, Tack J, Kuipers EJ, Graham DY, El-Omar EM, Miura S, et al. Kyoto Global Consensus Report on Helicobacter pylori Gastritis. Gut. 2015;64(9):1353–67.
Chey WD, Leontiadis GI, Howden CW, Moss SF. ACG Clinical Guideline: treatment of Helicobacter pylori Infection. Am J Gastroenterol. 2017;112(2):212–39.
Chitapanarux T, Kongkarnka S, Wannasai K, Sripan P. Prevalence and factors associated with atrophic gastritis and intestinal metaplasia: a multivariate, hospital-based, statistical analysis. Cancer Epidemiol. 2023;82: 102309.
Eriksson NK, Kärkkäinen PA, Färkkilä MA, Arkkila PET. Prevalence and distribution of gastric intestinal metaplasia and its subtypes. Dig Liver Dis. 2008;40(5):355–60.
Liu WZ, **e Y, Lu H, Cheng H, Zeng ZR, Zhou LY, et al. Fifth Chinese National Consensus Report on the management of Helicobacter pylori infection. Helicobacter. 2018;23(2): e12475.
Leung WK, Wong IOL, Cheung KS, Yeung KF, Chan EW, Wong AYS, et al. Effects of Helicobacter pylori treatment on incidence of gastric cancer in older individuals. Gastroenterology. 2018;155(1):67–75.
Take S, Mizuno M, Ishiki K, Kusumoto C, Imada T, Hamada F, et al. Risk of gastric cancer in the second decade of follow-up after helicobacter pylori eradication. J Gastroenterol. 2020;55(3):281–8.
Wu S-R, Liu Y-H, Shi Y-Q. Is intestinal metaplasia the point of no return in the progression of gastric carcinogenesis? Chin Med J (Engl). 2021;134(24):2965–7.
Hwang Y-J, Kim N, Lee HS, Lee JB, Choi YJ, Yoon H, et al. Reversibility of atrophic gastritis and intestinal metaplasia after Helicobacter pylori eradication—a prospective study for up to 10 years. Aliment Pharmacol Ther. 2018;47(3):380–90.
Yan L, Chen Y, Chen F, Tao T, Hu Z, Wang J, et al. Effect of Helicobacter pylori eradication on gastric cancer prevention: updated report from a randomized controlled trial with 26.5 years of follow-up. Gastroenterology. 2022;163(1):154-162.e3.
Khan MY, Aslam A, Mihali AB, Shabbir Rawala M, Dirweesh A, Khan S, et al. Effectiveness of Helicobacter pylori eradication in preventing metachronous gastric cancer and preneoplastic lesions. A systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2020;32(6):686–94.
Chen H-N, Wang Z, Li X, Zhou Z-G. Helicobacter pylori eradication cannot reduce the risk of gastric cancer in patients with intestinal metaplasia and dysplasia: evidence from a meta-analysis. Gastric Cancer. 2016;19(1):166–75.
Ng JC, Yeomans ND. Helicobacter pylori infection and the risk of upper gastrointestinal bleeding in low dose aspirin users: systematic review and meta-analysis. Med J Aust. 2018;209(7):306–11.
Hawkey C, Avery A, Coupland CAC, Crooks C, Dumbleton J, Hobbs FDR, et al. Helicobacter pylori eradication for primary prevention of peptic ulcer bleeding in older patients prescribed aspirin in primary care (HEAT): a randomised, double-blind, placebo-controlled trial. Lancet (London, England). 2022;400(10363):1597–606.
Hellström PM, Benno P, Malfertheiner P. Gastrointestinal bleeding in patients with helicobacter pylori and dual platelet inhibition after myocardial infarction. Lancet Gastroenterol Hepatol. 2021;6(9):684–5.
Waluga M, Kukla M, Żorniak M, Bacik A, Kotulski R. From the stomach to other organs: Helicobacter pylori and the liver. World J Hepatol. 2015;7(18):2136–46.
Yu Y-Y, Tong Y-L, Wu L-Y, Yu X-Y. Helicobacter pylori infection eradication for nonalcoholic fatty liver disease: a randomized controlled trial. Sci Rep. 2022;12(1):19530.
Lolekha P, Sriphanom T, Vilaichone R-K. Helicobacter pylori eradication improves motor fluctuations in advanced Parkinson’s disease patients: a prospective cohort study (HP-PD trial). PLoS ONE. 2021;16(5): e0251042.
Bugdaci MS, Zuhur SS, Sokmen M, Toksoy B, Bayraktar B, Altuntas Y. The role of Helicobacter pylori in patients with hypothyroidism in whom could not be achieved normal thyrotropin levels despite treatment with high doses of thyroxine. Helicobacter. 2011;16(2):124–30.
Centanni M, Gargano L, Canettieri G, Viceconti N, Franchi A, Delle Fave G, et al. Thyroxine in Goiter, Helicobacter pylori infection, and chronic gastritis. N Engl J Med. 2006;354(17):1787–95.
Rahmani Y, Mohammadi S, Babanejad M, Rai A, Zalei B, Shahmohammadi A. Association of Helicobacter pylori with presence of myocardial infarction in Iran: a systematic review and meta-analysis. Ethiop J Health Sci. 2017;27(4):433–40.
Azarkar Z, Jafarnejad M, Sharifzadeh G. The relationship between Helicobacter pylori infection and myocardial infarction. Casp J Intern Med. 2011;2(2):222–5.
Sharma V, Aggarwal A. Helicobacter pylori: does it add to risk of coronary artery disease. World J Cardiol. 2015;7(1):19–25.
Weinstein JR, Anderson S. The aging kidney: physiological changes. Adv Chronic Kidney Dis. 2010;17(4):302–7.
Kovesdy CP. Epidemiology of Chronic Kidney Disease: an Update 2022. Kidney Int Suppl. 2022;12(1):7–11.
Kinoshita Y, Ishimura N, Ishihara S. Advantages and disadvantages of long-term proton pump inhibitor use. J Neurogastroenterol Motil. 2018;24(2):182–96.
Yibirin M, De Oliveira D, Valera R, Plitt AE, Lutgen S. Adverse effects associated with proton pump inhibitor use. Cureus. 2021;13(1): e12759.
Masclee GMC, Sturkenboom MCJM, Kuipers EJ. A benefit-risk assessment of the use of proton pump inhibitors in the elderly. Drugs Aging. 2014;31(4):263–82.
Maes ML, Fixen DR, Linnebur SA. Adverse effects of proton-pump inhibitor use in older adults: a review of the evidence. Ther Adv Drug Saf. 2017;8(9):273–97.
Vanderhoff BT, Tahboub RM. Proton pump inhibitors: an update. Am Fam Physician. 2002;66(2):273–80.
Nabeta H, Shinozaki S, Abe Y, Koyanagi R, Nakamichi T, Kobayashi Y, et al. A potassium-competitive acid blocker-based regimen as second-line therapy improves Helicobacter pylori eradication. Digestion. 2020;101(3):332–8.
Kiyotoki S, Nishikawa J, Sakaida I. Efficacy of vonoprazan for Helicobacter pylori eradication. Intern Med. 2020;59(2):153–61.
Simadibrata DM, Syam AF, Lee YY. A comparison of efficacy and safety of potassium-competitive acid blocker and proton pump inhibitor in gastric acid-related diseases: a systematic review and meta-analysis. J Gastroenterol Hepatol. 2022;37(12):2217–28.
UpToDate. Drug Information. 2023 [cited 2023 Sep 3]. https://www.uptodate.com/contents/search. Accessed on 3 Sept 2023.
Drug Information. 2023 [cited 2023 Sep 3]. www.drugs.com. Accessed on 3 September, 2023.
Tsai C-E, Liang C-M, Lee C-H, Kuo Y-H, Wu K-L, Chiu Y-C, et al. First-line Helicobacter pylori eradication among patients with chronic liver diseases in Taiwan. Kaohsiung J Med Sci. 2016;32(8):397–402.
Jung SW, Lee SW, Hyun JJ, Kim DI, Koo JS, Yim HJ, et al. Efficacy of Helicobacter pylori eradication therapy in chronic liver disease. Dig Liver Dis. 2009;41(2):134–40.
Sharma NR, Wagle A, Bist M, Panthi B, Pokhrel Dahal R, Rokaya R, et al. Clarithromycin-induced Acute Liver injury in a Patient with Positive Helicobacter pylori: a Case Report and Review of the Literature. Vol. 85, Annals of medicine and surgery (2012). England; 2023. p. 4629–32.
Cheng D-D, He C, Ai H-H, Huang Y, Lu N-H. The possible role of Helicobacter pylori infection in non-alcoholic fatty liver disease. Front Microbiol. 2017;8:743.
Nyssen OP, Perez-Aisa A, Tepes B, Castro-Fernandez M, Kupcinskas J, Jonaitis L, et al. Adverse event profile during the treatment of helicobacter pylori: a real-world experience of 22,000 patients from the European registry on H. pylori management (Hp-EuReg). Am J Gastroenterol. 2021;116(6):1220–9.
Pulia MS, Keller SC, Crnich CJ, Jump RLP, Yoshikawa TT. Antibiotic stewardship for older adults in ambulatory care settings: addressing an unmet challenge. J Am Geriatr Soc. 2020;68(2):244–9.
Faulkner CM, Cox HL, Williamson JC. Unique aspects of antimicrobial use in older adults. Clin Infect Dis. 2005;40(7):997–1004.
Mégraud F, Graham DY, Howden CW, Trevino E, Weissfeld A, Hunt B, et al. Rates of antimicrobial resistance in helicobacter pylori isolates from clinical trial patients across the US and Europe. Am J Gastroenterol. 2023;118(2):269–75.
Denkinger CM, Grant AD, Denkinger M, Gautam S, D’Agata EMC. Increased multi-drug resistance among the elderly on admission to the hospital—a 12-year surveillance study. Arch Gerontol Geriatr. 2013;56(1):227–30.
Yoshikawa TT. Antimicrobial resistance and aging: beginning of the end of the antibiotic era? J Am Geriatr Soc. 2002;50(7 Suppl):S226–9.
Gao C, Fan Y-H. Effect and safety of helicobacter pylori eradication treatment based on molecular pathologic antibiotic resistance in chinese elderly people. Infect Drug Resist. 2022;15:3277–86.
Durazzo M, Ferro A, Fagoonee S, Staiano MT, Saracco GM, Pellicano R. Helicobacter pylori eradication with a clarithromycin-based triple therapy in elderly patients. Panminerva Med. 2021;63(3):332–5.
Ma T-L, Tai W-C, Loke S-S, Yao C-C, Liang C-M, Chuah S-K. Efficacy and safety of 7-day non-Bismuth concomitant quadruple therapy for first-line Helicobacter pylori eradication in the elderly. Drugs Aging. 2023;40(1):71–9.
Dore MP, Maragkoudakis E, Pironti A, Tadeu V, Tedde R, Realdi G, et al. Twice-a-day quadruple therapy for eradication of Helicobacter pylori in the elderly. Helicobacter. 2006;11(1):52–5.
Zullo A, Gatta L, De Francesco V, Hassan C, Ricci C, Bernabucci V, et al. High rate of Helicobacter pylori eradication with sequential therapy in elderly patients with peptic ulcer: a prospective controlled study. Aliment Pharmacol Ther. 2005;21(12):1419–24.
Wedemeyer R-S, Blume H. Pharmacokinetic drug interaction profiles of proton pump inhibitors: an update. Drug Saf. 2014;37(4):201–11.
Li W, Zeng S, Yu L-S, Zhou Q. Pharmacokinetic drug interaction profile of omeprazole with adverse consequences and clinical risk management. Ther Clin Risk Manag. 2013;9:259–71.
Cadiou G, Adam M, Caussin M, Landrin I, Mariette N, Capet C, et al. Antiplatelet drugs in the elderly: prescriptions often inappropriate and reduced tolerance by associated diseases and drugs. Fundam Clin Pharmacol. 2012;26(2):307–13.
Jonaitis P, Jonaitis L, Kupcinskas J. Role of genetic polymorphisms of cytochrome P450 2C19 in pantoprazole metabolism and pantoprazole-based Helicobacter pylori eradication regimens. Curr Drug Metab. 2020;21(11): 830–837.
Harmsze AM, de Boer A, Boot H, Deneer VHM, Heringa M, Mol PGM, et al. Interaction Between Clopidogrel and Proton Pump Inhibitors. Ned Tjdschrift voor Geneeskd. 2011;155(28):A2442.
Choi YJ, Kim N, Jang I-J, Cho J-Y, Nam RH, Park JH, et al. Pantoprazole does not reduce the antiplatelet effect of clopidogrel: a randomized controlled trial in Korea. Gut Liver. 2017;11(4):504–11.
Scott SA, Owusu Obeng A, Hulot J-S. Antiplatelet drug interactions with proton pump inhibitors. Expert Opin Drug Metab Toxicol. 2014;10(2):175–89.
Hines LE, Murphy JE. Potentially Harmful Drug-drug Interactions in the Elderly: a Review. Am J Geriatr Pharmacother. 2011;9(6):364–77.
Soraci L, Cherubini A, Paoletti L, Filippelli G, Luciani F, Laganà P, et al. Safety and tolerability of antimicrobial agents in the older patient. Drugs Aging. 2023;40(6):499–526.
Lee SP, Sung I-K, Kim JH, Lee S-Y, Park HS, Shim CS. Risk factors for the presence of symptoms in peptic ulcer disease. Clin Endosc. 2017;50(6):578–84.
Shiotani A, Manabe N, Kamada T, Fujimura Y, Sakakibara T, Haruma K. Risk and preventive factors of low-dose aspirin-induced gastroduodenal injuries: a comprehensive review. J Gastroenterol Hepatol. 2012;27(Suppl 3):8–12.
Wongrakpanich S, Wongrakpanich A, Melhado K, Rangaswami J. A comprehensive review of non-steroidal anti-inflammatory drug use in the elderly. Aging Dis. 2018;9(1):143–50.
O’Brien CW, Juraschek SP, Wee CC. Prevalence of aspirin use for primary prevention of cardiovascular disease in the United States: results from the 2017 National Health Interview Survey. Ann Intern Med. 2019;171(8):596–8.
Pilotto A, Franceschi M, Maggi S, Addante F, Sancarlo D. Optimal management of peptic ulcer disease in the elderly. Drugs Aging. 2010;27(7):545–58.
Joo MK. Helicobacter pylori eradication in drug-related peptic ulcer. Korean J Gastroenterol. 2020;76(5):227–31.
Jump RL. Clostridium difficile infection in older adults. Aging health. 2013;9(4):403–14.
Mullish BH, Williams HR. Clostridium difficile infection and antibiotic-associated diarrhoea. Clin Med. 2018;18(3):237–41.
Tawam D, Baladi M, Jungsuwadee P, Earl G, Han J. The positive association between proton pump inhibitors and Clostridium difficile infection. Inov Pharm. 2021;12(1):1–7.
Inghammar M, Svanström H, Voldstedlund M, Melbye M, Hviid A, Mølbak K, et al. Proton-pump inhibitor use and the risk of community-associated Clostridium difficile Infection. Clin Infect Dis. 2021;72(12):e1084–9.
Kumar S, Metz DC, Kaplan DE, Goldberg DS. Treatment of Helicobacter pylori is not associated with future clostridium difficile infection. Am J Gastroenterol. 2020;115(5):716–22.
Trifan A, Girleanu I, Cojocariu C, Sfarti C, Singeap AM, Dorobat C, et al. Pseudomembranous colitis associated with a triple therapy for Helicobacter pylori eradication. World J Gastroenterol. 2013;19(42):7476–9.
Castro-Fernández M, Marqués-Ruiz A, Cámara-Baena S, Grande-Santamaría L. Clostridium difficile infection associated with bismuth-based quadruple therapy (Pylera®) for Helicobacter pylori eradication. Gastroenterol y Hepatol (English ed). 2019;42(7):459–60. https://www.elsevier.es/en-revista-gastroenterologia-hepatologia-english-edition--382-articulo-clostridium-difficile-infection-associated-with-S2444382419301671. Accessed on 8 Sept 2023.
Nishida T, Tsujii Y, Okamoto A, Tomita R, Higaki Y, Osugi N, et al. A triple-drug blister-packaged drug with vonoprazan improves first-line eradication of Helicobacter pylori in elderly patients: a retrospective propensity score-matched cohort study. Digestion. 2020;101(5):608–14.
Chey WD, Mégraud F, Laine L, López LJ, Hunt BJ, Howden CW. Vonoprazan triple and dual therapy for Helicobacter pylori infection in the united states and europe: randomized clinical trial. Gastroenterology. 2022;163(3):608–19.
Yang Q, He C, Hu Y, Hong J, Zhu Z, **e Y, et al. 14-day pantoprazole- and amoxicillin-containing high-dose dual therapy for Helicobacter pylori eradication in elderly patients: a prospective, randomized controlled trial. Front Pharmacol. 2023;14:1096103.
Gao W, Ye H, Deng X, Wang C, Xu Y, Li Y, et al. Rabeprazole-amoxicillin dual therapy as first-line treatment for H. pylori eradication in special patients: a retrospective, real-life study. Helicobacter. 2020;25(5): e12717.
Mestrovic A, Perkovic N, Tonkic A, Sundov Z, Kumric M, Bozic J. Personalized approach in eradication of Helicobacter pylori infection. Antibiot (Basel, Switzerland). 2022;12(1):7.
Smith SM, O’Morain C, McNamara D. Antimicrobial susceptibility testing for Helicobacter pylori in times of increasing antibiotic resistance. World J Gastroenterol. 2014;20(29):9912–21.
Nyssen OP, Espada M, Gisbert JP. Empirical vs. susceptibility-guided treatment of Helicobacter pylori infection: a systematic review and meta-analysis. Front Microbiol. 2022;13:913436.
Kuo C-H, Lu C-Y, Shih H-Y, Liu C-J, Wu M-C, Hu H-M, et al. CYP2C19 polymorphism influences Helicobacter pylori eradication. World J Gastroenterol. 2014;20(43):16029–36.
Morino Y, Sugimoto M, Nagata N, Niikiura R, Iwata E, Hamada M, et al. Influence of cytochrome P450 2C19 genotype on Helicobacter pylori proton pump inhibitor-amoxicillin-clarithromycin eradication therapy: a meta-analysis. Front Pharmacol. 2021;12: 759249.
Mestre A, Sathiya Narayanan R, Rivas D, John J, Abdulqader MA, Khanna T, et al. Role of probiotics in the management of Helicobacter pylori. Cureus. 2022;14(6): e26463.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No specific funding was used to conduct this review.
Conflicts of Interest
Javier P. Gisbert has served as speaker, consultant, and advisory member for, or has received research funding from, Mayoly, Allergan, Diasorin, Gebro Pharma, and Richen. Paulius Jonaitis, Juozas Kupcinskas and Laimas Jonaitis have declared no conflicts of interest.
Data Availability Statement
Not applicable.
Authors’ Contributions
Conceptualization: JPG and LJ. Writing—original draft preparation: PJ and LJ. Writing—review and editing: JK, JPG, LJ. Visualization: PJ. Supervision: JK, JPG, LJ. All authors have read and approved the final version of the manuscript.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jonaitis, P., Kupcinskas, J., Gisbert, J.P. et al. Helicobacter pylori Eradication Treatment in Older Patients. Drugs Aging 41, 141–151 (2024). https://doi.org/10.1007/s40266-023-01090-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-023-01090-w