Abstract
The prevalence and embolic risk of atrial fibrillation (AF) increase with age. Vitamin K antagonists (VKAs) or direct-acting oral anticoagulants (DOACs) reduce the risk of stroke or embolism. The aim of this review was to summarize the paucity of information regarding the safety and efficacy of DOACs in AF patients aged 90 years or older. The maximum age of included patients is not listed in any of the available DOAC investigating trials and registries, thus it is unclear if nonagenarians were included. Additionally, we could not find any subgroup analysis addressing this issue. There is an urgent need to collect more information on the safety and efficacy of oral anticoagulants in nonagenarians, especially regarding the role of DOACs, which are increasingly prescribed to this group of patients despite the lack of data. The best solution to this problem would be a prospective, randomized trial in this group of patients, however that would require a large investment of time, effort, and funds. In the meantime, we suggest subgroup analyses addressing the effects and safety of VKAs versus DOACs in nonagenarians, in case they have been included in previously completed or ongoing trials or registries. This could be feasible and would be desirable in view of the large amount of data already accumulated. Irrespective of age, anemia in patients receiving DOACs should be carefully investigated to rule out occult blood loss. With their known interaction profile and the possibility of monitoring these drugs, VKAs should be favored over DOACs in nonagenarians until more data are available regarding the safety of DOACs.

Similar content being viewed by others
References
Schnabel RB, Yin X, Gona P, Larson MG, Beiser AS, McManus DD, et al. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: a cohort study. Lancet. 2015;386:154–62.
Dreischulte T, Barnett K, Madhok V, Guthrie B. Use of oral anticoagulants in atrial fibrillation is highly variable and only weakly associated with estimated stroke risk: cross-sectional population database study. Eur J Gen Pract. 2014;20:181–9.
Charlton B, Redberg R. The trouble with dabigatran. BMJ. 2014;349:g4681.
Deshpande A, Sampat P, Bhargavan R, Sharma M. Bleeding isolated jejunal varices without portal hypertension. ANZ J Surg. 2008;78:814–5.
Stöllberger C, Finsterer J. Concerns about the use of new oral anticoagulants for stroke prevention in elderly patients with atrial fibrillation. Drugs Aging. 2013;30:949–58.
Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007;146:857–67.
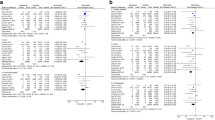
Sharma M, Cornelius VR, Patel JP, Davies JG, Molokhia M. Efficacy and harms of direct oral anticoagulants in the elderly for stroke prevention in atrial fibrillation and secondary prevention of venous thromboembolism: systematic review and meta-analysis. Circulation. 2015;132:194–204.
Sardar P, Chatterjee S, Chaudhari S, Lip GY. New oral anticoagulants in elderly adults: evidence from a meta-analysis of randomized trials. J Am Geriatr Soc. 2014;62:857–64.
Lutz W, Sanderson W, Scherbov S. The coming acceleration of global population ageing. Nature. 2008;451:716–9.
Mandalenakis Z, Von Koch L, Eriksson H, Dellborg M, Caidahl K, Welin L, et al. The risk of atrial fibrillation in the general male population: a lifetime follow-up of 50-year-old men. Europace. 2015;17:1018–22.
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–51.
Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, et al. ARISTOTLE Committees and Investigators. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365:981–92.
Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. ROCKET AF Investigators. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–91.
Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, et al. ENGAGE AF-TIMI 48 Investigators. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369:2093–104.
Steinberg BA, Holmes DN, Ezekowitz MD, Fonarow GC, Kowey PR, Mahaffey KW, et al. Rate versus rhythm control for management of atrial fibrillation in clinical practice: results from the outcomes registry for better informed treatment of atrial fibrillation (ORBIT-AF) registry. Am Heart J. 2013;165:622–9.
Beyer-Westendorf J, Förster K, Ebertz F, Gelbricht V, Schreier T, Göbelt M, et al. Drug persistence with rivaroxaban therapy in atrial fibrillation patients-results from the Dresden non-interventional oral anticoagulation registry. Europace. 2015;17:530–8.
Huisman MV, Rothman KJ, Paquette M, Teutsch C, Diener HC, Dubner SJ, et al. GLORIA-AF Investigators. Antithrombotic treatment patterns in patients with newly diagnosed nonvalvular atrial fibrillation: the GLORIA-AF Registry, Phase II. Am J Med. 2015;128(1306–13):e1.
Kakkar AK, Mueller I, Bassand JP, Fitzmaurice DA, Goldhaber SZ, Goto S, et al. GARFIELD Registry Investigators. Risk profiles and antithrombotic treatment of patients newly diagnosed with atrial fibrillation at risk of stroke: perspectives from the international, observational, prospective GARFIELD registry. PLoS One. 2013;8:e63479.
Hsu JC, Chan PS, Tang F, Maddox TM, Marcus GM. Differences in anticoagulant therapy prescription in patients with paroxysmal versus persistent atrial fibrillation. Am J Med. 2015;128:654.e1–654.e10.
Lip GY, Laroche C, Ioachim PM, Rasmussen LH, Vitali-Serdoz L, Petrescu L, et al. Prognosis and treatment of atrial fibrillation patients by European cardiologists: one year follow-up of the EURObservational Research Programme-Atrial Fibrillation General Registry Pilot Phase (EORP-AF Pilot registry). Eur Heart J. 2014;35:3365–76.
Eikelboom JW, Wallentin L, Connolly SJ, Ezekowitz M, Healey JS, Oldgren J, et al. Risk of bleeding with 2 doses of dabigatran compared with warfarin in older and younger patients with atrial fibrillation: an analysis of the randomized evaluation of long-term anticoagulant therapy (RE-LY) trial. Circulation. 2011;123:2363–72.
Halvorsen S, Atar D, Yang H, De Caterina R, Erol C, Garcia D, et al. Efficacy and safety of apixaban compared with warfarin according to age for stroke prevention in atrial fibrillation: observations from the ARISTOTLE trial. Eur Heart J. 2014;35:1864–72.
Xu Y, Holbrook AM, Simpson CS, Dowlatshahi D, Johnson AP. Prescribing patterns of novel oral anticoagulants following regulatory approval for atrial fibrillation in Ontario, Canada: a population-based descriptive analysis. CMAJ Open. 2013;1:E115–9.
Olesen JB, Sørensen R, Hansen ML, Lamberts M, Weeke P, Mikkelsen AP, et al. Non-vitamin K antagonist oral anticoagulation agents in anticoagulant naïve atrial fibrillation patients: Danish nationwide descriptive data 2011-2013. Europace. 2015;17:187–93.
Metcalfe S, Moodie P. National prescribing data for dabigatran. N Z Med J. 2012;125:97–105.
Kirley K, Qato DM, Kornfield R, Stafford RS, Alexander GC. National trends in oral anticoagulant use in the United States, 2007 to 2011. Circ Cardiovasc Qual Outcomes. 2012;5:615–21.
Harper P, Young L, Merriman E. Bleeding risk with dabigatran in the frail elderly. N Engl J Med. 2012;366:864–6.
Chang DN, Dager WE, Chin AI. Removal of dabigatran by hemodialysis. Am J Kidney Dis. 2013;61:487–9.
Kernan L, Ito S, Shirazi F, et al. Fatal gastrointestinal hemorrhage after a single dose of dabigatran. Clin Toxicol (Phila). 2012;50:571–3.
Fontaine GV, Mathews KD, Woller SC, Stevens SM, Lloyd JF, Evans RS. Major bleeding with dabigatran and rivaroxaban in patients with atrial fibrillation: a real-world setting. Clin Appl Thromb Hemost. 2014;20:665–72.
Lo JC, Gerona RR. A case of rivaroxaban associated intracranial hemorrhage. West J Emerg Med. 2014;15:375–7.
King AE, Szarlej DK, Rincon F. Dabigatran-associated intracranial hemorrhage: literature review and institutional experience. Neurohospitalist. 2015;5:234–44.
Baumann D, Haap M, Tsaousidis C, Krämer B, Schreieck J, Jaschonek K, et al. Vaginal bleeding as symptom of a medical emergency: pitfalls of therapy with new oral anticoagulants—case 5/2014. Dtsch Med Wochenschr. 2014;139:1539.
Kramarow E, Chen LH, Hedegaard H, Warner M. Deaths from unintentional injury among adults aged 65 and over: United States, 2000-2013. NCHS Data Brief. 2015;199:199.
Chang HY, Zhou M, Tang W, Alexander GC, Singh S. Risk of gastrointestinal bleeding associated with oral anticoagulants: population based retrospective cohort study. BMJ. 2015;350:h1585.
Goodman SG, Wojdyla DM, Piccini JP, et al. Factors associated with major bleeding events: insights from the ROCKET AF trial (rivaroxaban once-daily oral direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation). J Am Coll Cardiol. 2014;63:891–900.
Abraham NS, Singh S, Alexander GC, Heien H, Haas LR, Crown W, et al. Comparative risk of gastrointestinal bleeding with dabigatran, rivaroxaban, and warfarin: population based cohort study. BMJ. 2015;350:h1857.
Blech S, Ebner T, Ludwig-Schwellinger E, Stangier J, Roth W. The metabolism and disposition of the oral direct thrombin inhibitor, dabigatran, in humans. Drug Metab Dispos. 2008;36(2):386–99.
Weinz C, Schwarz T, Kubitza D, Mueck W, Lang D. Metabolism and excretion of rivaroxaban, an oral, direct factor Xa inhibitor, in rats, dogs, and humans. Drug Metab Dispos. 2009;37:1056–64.
Raghavan N, Frost CE, Yu Z, He K, Zhang H, Humphreys WG, et al. Apixaban metabolism and pharmacokinetics after oral administration to humans. Drug Metab Dispos. 2009;37:74–81.
Bathala MS, Masumoto H, Oguma T, He L, Lowrie C, Mendell J. Pharmacokinetics, biotransformation, and mass balance of edoxaban, a selective, direct factor Xa inhibitor, in humans. Drug Metab Dispos. 2012;40:2250–5.
Stöllberger C, Finsterer J. Relevance of P-glycoprotein in stroke prevention with dabigatran, rivaroxaban, and apixaban. Herz. 2015;40(Suppl 2):140–5.
Takahashi N, Inui N, Morita H, et al. Effect of thyroid hormone on the activity of CYP3A enzyme in humans. J Clin Pharmacol. 2010;50:88–93.
Böhm M, Ezekowitz MD, Connolly SJ, Eikelboom JW, Hohnloser SH, Reilly PA, et al. Changes in renal function in patients with atrial fibrillation: an analysis from the RE-LY trial. J Am Coll Cardiol. 2015;65:2481–93.
Manzano-Fernández S, Andreu-Cayuelas JM, Marín F, Orenes-Piñero E, Gallego P, Valdés M, et al. Comparison of estimated glomerular filtration rate equations for dosing new oral anticoagulants in patients with atrial fibrillation. Rev Esp Cardiol (Engl Ed). 2015;68:497–504.
Ruff CT, Giugliano RP, Braunwald E, Antman EM. New oral anticoagulants in patients with atrial fibrillation—authors’ reply. Lancet. 2014;384:25–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this manuscript.
Conflict of interest
Claudia Stöllberger, Roman Brooks, Josef Finsterer, Thomas Pachofszky declare that they have no conflicts of interest that might be relevant to the contents of this manuscript.
Rights and permissions
About this article
Cite this article
Stöllberger, C., Brooks, R., Finsterer, J. et al. Use of Direct-Acting Oral Anticoagulants in Nonagenarians: A Call for More Data. Drugs Aging 33, 315–320 (2016). https://doi.org/10.1007/s40266-016-0363-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-016-0363-4