Abstract
Introduction
The escalating burden of catastrophic health expenditure (CHE) poses a significant threat to individuals and households in India, where out-of-pocket expenditure (OOP) constitutes a substantial portion of healthcare financing. With rising OOP in India, a proper measurement to track and monitor CHE due to health expenditure is of utmost important. This study focuses on synthesizing findings, understanding measurement variations, and estimating the pooled incidence of CHE by health services, reported diseases, and survey types.
Method
Following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, a thorough search strategy was employed across multiple databases, between 2010 and 2023. Inclusion criteria encompassed observational or interventional studies reporting CHE incidence, while exclusion criteria screened out studies with unclear definitions, pharmacy revenue-based spending, or non-representative health facility surveys. A meta-analysis, utilizing a random-effects model, assessed the pooled CHE incidence. Sensitivity analysis and subgroup analyses were conducted to explore heterogeneity.
Results
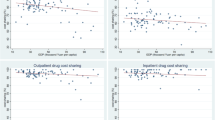
Out of 501 initially relevant articles, 36 studies met inclusion criteria. The review identified significant variations in CHE measurements, with incidence ranging from 5.1% to 69.9%. Meta-analysis indicated the estimated incidence of CHE at a 10% threshold is 0.30 [0.25–0.35], indicating a significant prevalence of financial hardship due to health expenses. The pooled incidence is estimated by considering different sub-groups. No statistical differences were found between inpatient and outpatient CHE. However, disease-specific estimates were significantly higher (52%) compared to combined diseases (21%). Notably, surveys focusing on health reported higher CHE (33%) than consumption surveys (14%).
Discussion
The study highlights the intricate challenges in measuring CHE, emphasizing variations in recall periods, components considered in out-of-pocket expenditure, and diverse methods for defining capacity to pay. Notably, the findings underscore the need for standardized definitions and measurements across studies. The lack of uniformity in reporting exacerbates the challenge of comparing and comprehensively understanding the financial burden on households.





Similar content being viewed by others
References
Bredenkamp C, Mendola M, Gragnolati M. Catastrophic and impoverishing effects of health expenditure: new evidence from the Western Balkans. Health Policy Plan. 2011;26:349–56. https://doi.org/10.1093/heapol/czq070.
Joe W. Distressed financing of household out-of-pocket health care payments in India: incidence and correlates. Health Policy Plan. 2015;30:728–41. https://doi.org/10.1093/heapol/czu050.
Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJL. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362:111–7. https://doi.org/10.1016/S0140-6736(03)13861-5.
Wagstaff A, Flores G, Hsu J, Smitz MF, Chepynoga K, Buisman LR, et al. Progress on catastrophic health spending in 133 countries: a retrospective observational study. Lancet Glob Heal. 2018;6:e169–79. https://doi.org/10.1016/S2214-109X(17)30429-1.
Nandi A, Ashok A, Laxminarayan R. The socioeconomic and institutional determinants of participation in India’s health insurance scheme for the poor. PLoS ONE. 2013. https://doi.org/10.1371/journal.pone.0066296.
Raban MZ, Dandona R, Dandona L. Variations in catastrophic health expenditure estimates from household surveys in India. Bull World Health Organ. 2013;91:726–35. https://doi.org/10.2471/BLT.12.113100.
Shukla V, Arora R. The economic cost of rising non-communicable diseases in India: a systematic literature review of methods and estimates. Appl Health Econ Health Policy. 2023. https://doi.org/10.1007/s40258-023-00822-8.
Alam K, Mahal A. Economic impacts of health shocks on households in low and middle income countries: a review of the literature. Global Health. 2014. https://doi.org/10.1186/1744-8603-10-21.
Harrer M, Cuijpers P, Furukawa TA, Ebert DD. Doing meta-analysis with R. 2021.https://doi.org/10.1201/9781003107347
Wang N. How to conduct a meta-analysis of proportions in R: a comprehensive tutorial. John Jay Coll Crim Justice. 2016. p. 1–63.
Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. https://doi.org/10.1002/sim.1186.
Pandey A, Ploubidis GB, Clarke L, Dandona L. Trends in catastrophic health expenditure in India: 1993 to 2014. Bull World Health Organ. 2018;96:18–28. https://doi.org/10.2471/BLT.17.191759.
Yadav J, Menon GR, John D. Disease-specific out-of-pocket payments, catastrophic health expenditure and impoverishment effects in India: an analysis of national health survey data. Appl Health Econ Health Policy. 2021;19:769–82. https://doi.org/10.1007/s40258-021-00641-9.
Sangar S, Dutt V, Thakur R. Economic burden, impoverishment, and co** mechanisms associated with out-of-pocket health expenditure in India: a disaggregated analysis at the state level. Int J Health Plann Manage. 2019;34:e301–13. https://doi.org/10.1002/hpm.2649.
Nanda M, Sharma R. A comprehensive examination of the economic impact of out-of-pocket health expenditures in India. Health Policy Plan. 2023;38:926–38. https://doi.org/10.1093/heapol/czad050.
Mohanty SK, Dwivedi LK. Addressing data and methodological limitations in estimating catastrophic health spending and impoverishment in India, 2004–18. Int J Equity Health. 2021;20:1–18. https://doi.org/10.1186/s12939-021-01421-6.
Lee THJ, Saran I, Rao KD. Ageing in India: financial hardship from health expenditures. Int J Health Plan Manag. 2018;33:414–25. https://doi.org/10.1002/hpm.2478.
Tripathy JP, Jagnoor J, Prasad BM, Ivers R. Cost of injury care in India: cross-sectional analysis of National Sample Survey 2014. Inj Prev. 2018;24:116–22. https://doi.org/10.1136/injuryprev-2017-042318.
Mahal A, Karan A, Engelgau M. The economic implications of non-communicable disease for India. 2010.
Engelgau MM, Karan A, Mahal A. The economic impact of non-communicable diseases on households in India. Glob Health. 2012;8:9–12. https://doi.org/10.1186/1744-8603-8-9.
Yadav J, John D, Allarakha S, Menon GR. Rising healthcare expenditure on tuberculosis: can India achieve the End TB goal? Trop Med Int Health. 2021;26:1256–75. https://doi.org/10.1111/tmi.13648.
Mohanty SK, Sahoo U, Rashmi R. Old-age dependency and catastrophic health expenditure: evidence from Longitudinal Ageing Study in India. Int J Health Plan Manag. 2022;37:3148–71. https://doi.org/10.1002/hpm.3546.
Rajasulochana SR, Kar SS. Economic burden associated with stroke in India: insights from national sample survey 2017–18. Expert Rev Pharmacoecon Outcomes Res. 2021;00:1–9. https://doi.org/10.1080/14737167.2021.1941883.
Karan A, Farooqui HH, Hussain S, Hussain MA, Selvaraj S, Mathur MR. Multimorbidity, healthcare use and catastrophic health expenditure by households in India: a cross-section analysis of self-reported morbidity from national sample survey data 2017–18. BMC Health Serv Res. 2022;22:1–12. https://doi.org/10.1186/s12913-022-08509-x.
Verma VR, Kumar P, Dash U. Assessing the household economic burden of non-communicable diseases in India: evidence from repeated cross-sectional surveys. BMC Public Health. 2021;21:1–22. https://doi.org/10.1186/s12889-021-10828-3.
Sriram S, Albadrani M. A study of catastrophic health expenditures in India—evidence from nationally representative survey data: 2014–2018. F1000Research 2022;11:2014–8. https://doi.org/10.12688/f1000research.75808.1.
Madan J, Lönnroth K, Laokri S, Squire SB. What can dissaving tell us about catastrophic costs? Linear and logistic regression analysis of the relationship between patient costs and financial co** strategies adopted by tuberculosis patients in Bangladesh, Tanzania and Bangalore, India. BMC Health Serv Res. 2015;15:1–8. https://doi.org/10.1186/s12913-015-1138-z.
Behera S, Pradhan J. Uneven economic burden of noncommunicable diseases among Indian households: a comparative analysis. PLoS ONE. 2021;16:1–17. https://doi.org/10.1371/journal.pone.0260628.
Muniyandi M, Thomas BE, Karikalan N, Kannan T, Rajendran K, Saravanan B, et al. Association of tuberculosis with household catastrophic expenditure in South India. JAMA Netw Open. 2020;3:1–11. https://doi.org/10.1001/jamanetworkopen.2019.20973.
Kastor A, Mohanty SK. Disease-specific out-of-pocket and catastrophic health expenditure on hospitalization in India: do Indian households face distress health financing? PLoS ONE. 2018;13:1–18. https://doi.org/10.1371/journal.pone.0196106.
Maurya PK, Murali S, Jayaseelan V, Thulasingam M, Pandjatcharam J. Economic burden of cancer treatment in a region in South India: a cross sectional analytical study. Asian Pacific J Cancer Prev. 2021;22:3755–62. https://doi.org/10.31557/APJCP.2021.22.12.3755.
Yadav J, Menon G, Agarwal A, John D. Burden of injuries and its associated hospitalization expenditure in India. Int J Inj Contr Saf Promot. 2021;28:153–61. https://doi.org/10.1080/17457300.2021.1879163.
Mohanty SK, Agrawal NK, Mahapatra B, Choudhury D, Tuladhar S, Holmgren EV. Multidimensional poverty and catastrophic health spending in the mountainous regions of Myanmar, Nepal and India. Int J Equity Health. 2017;16:1–13. https://doi.org/10.1186/s12939-016-0514-6.
Dwivedi R, Pradhan J, Athe R. Measuring catastrophe in paying for healthcare: a comparative methodological approach by using National Sample Survey. India Int J Health Plan Manag. 2021;36:1887–915. https://doi.org/10.1002/hpm.3272.
Kumar K, Singh A, Kumar S, Ram F, Singh A, Ram U, et al. Socio-economic differentials in impoverishment effects of out-of-pocket health expenditure in China and India: evidence from WHO SAGE. PLoS ONE. 2015;10:1–19. https://doi.org/10.1371/journal.pone.0135051.
Hei**k R, Xu K, Saksana P, Evans D. Validity and Comparability of out-of- pocket health expenditure from household surveys: a review of the literature and current survey instruments. WHO Discuss Pap 2011. p. 1–30.
Mohanty SK, Kim R, Khan PK, Subramanian SV. Geographic variation in household and catastrophic health spending in India: assessing the relative importance of villages, districts, and states, 2011–2012. Milbank Q. 2018;96:167–206. https://doi.org/10.1111/1468-0009.12315.
Pandey KR, Meltzer DO. Financial burden and impoverishment due to cardiovascular medications in low and middle income countries: an illustration from India. PLoS ONE. 2016;11:1–19. https://doi.org/10.1371/journal.pone.0155293.
Yadav J, Allarakha S, Menon GR, John D, Nair S. Socioeconomic impact of hospitalization expenditure for treatment of noncommunicable diseases in India: a repeated cross-sectional analysis of national sample survey data, 2004 to 2018. Value Heal Reg Issues. 2021;24:199–213. https://doi.org/10.1016/j.vhri.2020.12.010.
Karan A, Selvaraj S, Mahal A. Moving to universal coverage? Trends in the burden of out-of-pocket payments for health care across social groups in India, 1999–2000 to 2011–12. PLoS ONE. 2014;9:1999–2000. https://doi.org/10.1371/journal.pone.0105162.
Gupta I, Joe W. Refining estimates of catastrophic healthcare expenditure: an application in the Indian context. Int J Health Care Finance Econ. 2013;13:157–72. https://doi.org/10.1007/s10754-013-9125-6.
Xu K, Ravndal F, Evans DB, Carrin G. Assessing the reliability of household expenditure data: results of the World Health Survey. Health Policy (New York). 2009;91:297–305. https://doi.org/10.1016/j.healthpol.2009.01.002.
Eze P, Lawani LO, Agu UJ, Acharya Y. Catastrophic health expenditure in sub-Saharan Africa: systematic review and meta-analysis. Bull World Health Organ. 2022;100:337-351J. https://doi.org/10.2471/BLT.21.287673.
Clarke PM, Fiebig DG, Gerdtham UG. Optimal recall length in survey design. J Health Econ. 2008;27:1275–84. https://doi.org/10.1016/j.jhealeco.2008.05.012.
Lu C, Chin B, Li G, Murray CJL. Limitations of methods for measuring out-of-pocket and catastrophic private health expenditures. Bull World Health Organ. 2009;87:238–44. https://doi.org/10.2471/BLT.08.054379.
Kalita A, Carton-Rossen N, Joseph L, Chhetri D, Patel V. The barriers to universal health coverage in India and the strategies to address them: a key informant study. Ann Glob Heal. 2023;89:69. https://doi.org/10.5334/aogh.4120.
Acknowledgements
The team mentioned in the Methods section consists of three independent reviewers, Umenthla Srikanth Reddy, Adrita Banerjee, and Tapasya Raj, who extracted papers and data from the selected papers. The authors acknowledge the contribution of Adrita Banerjee, Tapasya Raj and Shreya Singh in editing the manuscript and providing valuable feedback. The author also acknowledges the journal editor for meticulously reviewing the manuscript, as well as the anonymous reviewers for their valuable suggestions and feedback.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding has been received for the study; the paper is a part of PhD thesis.
Conflict of interest
The author declares no competing interests.
Ethics statement
Ethical approval for this type of study is not required by our institute.
Consent for publication
Not applicable.
Consent to participate
Not applicable.
Reflexivity statement
The author is a PhD student, this work is a part of his thesis. The author has an understanding and experience of health financing in India.
Availability of data and materials
Available upon request.
Code availability
Available upon request.
Author contributions
USR has conceptualised and designed the work. USR has collected the data and did analysis. Interpretation of the results were done by USR under the guidance of Prof. K.S. James (PhD supervisor). All the results were discussed with USR’s supervisor. The paper was drafted by USR. The critical revision was done by USR.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Reddy, U.S. Measurement of Catastrophic Health Expenditure in India: A Systematic Review and Meta-Analysis. Appl Health Econ Health Policy 22, 471–483 (2024). https://doi.org/10.1007/s40258-024-00885-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-024-00885-1