Abstract
Purpose
Lymphedema after cancer treatment is a progressive, debilitating condition that is becoming increasingly common as mortality rates decline. The purpose of this review is to summarize the evolution of treatment of lymphedema focusing on surgical management and outcomes.
Recent Findings
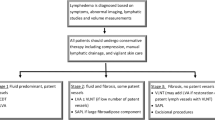
With the development of supermicrosurgical techniques and advanced imaging technology, surgical treatment of lymphedema has evolved past reductive measures and sought to address the underlying pathophysiology. Particularly in breast cancer-related lymphedema, our group follows a novel algorithm to address both the autologous breast reconstruction with physiologic treatment of the affected extremity.
Summary
Patients and physicians alike should be educated about the risk factors for develo** lymphedema after cancer treatment, prompt and proper diagnosis, as well as conservative and surgical treatment options. While the optimal treatment algorithm remains to be elucidated, a multi-modality treatment approach has demonstrated promising outcomes in symptom improvement, volume reduction, and quality of life.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: ∙ Of importance ∙∙ Of major importance
Rockson SG, Rivera KK. Estimating the population burden of lymphedema. Ann N Y Acad Sci. 2008;1131:147–54.
Schook CC, Mulliken JB, Fishman SJ, Grant FD, Zurakowski D, Greene AK. Primary lymphedema: clinical features and management in 138 pediatric patients. Plast Reconstr Surg. 2011;127(6):2419–31.
Mendola A, Schlögel MJ, Ghalamkarpour A, Irrthum A, Nguyen HL, Fastré E, et al. Mutations in the VEGFR3 signaling pathway explain 36% of familial lymphedema. Mol Syndromol. 2013;4(6):257–66.
Cormier JN, Askew RL, Mungovan KS, **ng Y, Ross MI, Armer JM. Lymphedema beyond breast cancer: a systematic review and meta-analysis of cancer-related secondary lymphedema. Cancer. 2010;116(22):5138–49.
∙ Voss RK, Cromwell KD, Chiang YJ, Armer JM, Ross MI, Lee JE, et al. The long-term risk of upper-extremity lymphedema is two-fold higher in breast cancer patients than in melanoma patients. Journal of surgical oncology. 2015;112(8):834–40. This manuscript establsihes rate of lymphedema in two commonly treated cancers.
Armer JM, Ballman KV, McCall L, Ostby PL, Zagar E, Kuerer HM, et al. Factors associated with lymphedema in women with node-positive breast cancer treated with neoadjuvant chemotherapy and axillary dissection. JAMA Surg. 2019;154(9):800–9.
Shaitelman SF, Chiang YJ, Griffin KD, DeSnyder SM, Smith BD, Schaverien MV, et al. Radiation therapy targets and the risk of breast cancer-related lymphedema: a systematic review and network meta-analysis. Breast Cancer Res Treat. 2017;162(2):201–15.
DiSipio T, Rye S, Newman B, Hayes S. Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol. 2013;14(6):500–15.
Mihara M, Hara H, Hayashi Y, Narushima M, Yamamoto T, Todokoro T, et al. Pathological steps of cancer-related lymphedema: histological changes in the collecting lymphatic vessels after lymphadenectomy. PLoS ONE. 2012;7(7):e41126.
Zampell JC, Yan A, Elhadad S, Avraham T, Weitman E, Mehrara BJ. CD4(+) cells regulate fibrosis and lymphangiogenesis in response to lymphatic fluid stasis. PLoS ONE. 2012;7(11):e49940.
Zhang L, Fan A, Yan J, He Y, Zhang H, Zhang H, et al. Combining manual lymph drainage with physical exercise after modified radical mastectomy effectively prevents upper limb lymphedema. Lymphatic Res Biol. 2016;14(2):104–8.
Schaverien MV, Moeller JA, Cleveland SD. Nonoperative treatment of lymphedema. Semin Plast Surg. 2018;32(1):17–21.
Suami H, Chang DW. Overview of surgical treatments for breast cancer-related lymphedema. Plast Reconstr Surg. 2010;126(6):1853–63.
Schaverien MV, Coroneos CJ. Surgical treatment of lymphedema. Plast Reconstr Surg. 2019;144(3):738–58.
∙∙ Chang EI, Schaverien MV, Hanson SE, Chu CK, Hanasono MM. Evolution in surgical management of breast cancer-related lymphedema: the MD Anderson Cancer Center Experience. Plast Reconstr Surg Glob Open. 2020;8(3). **This manuscript provides detiled description of the authors' preferred combined approach to breast cancer related lymphedema including outcomes at our institution.
Akita S, Mitsukawa N, Kuriyama M, Hasegawa M, Kubota Y, Tokumoto H, et al. Suitable therapy options for sub-clinical and early-stage lymphoedema patients. J Plast Reconstr Aesthet Surg. 2014;67(4):520–5.
Coroneos CJ, Wong FC, DeSnyder SM, Shaitelman SF, Schaverien MV. Correlation of L-Dex bioimpedance spectroscopy with limb volume and lymphatic function in lymphedema. Lymphatic Res Biol. 2019;17(3):301–7.
Neligan PC, Kung TA, Maki JH. MR lymphangiography in the treatment of lymphedema. J Surg Oncol. 2017;115(1):18–22.
Suami H, Chang DW, Yamada K, Kimata Y. Use of indocyanine green fluorescent lymphography for evaluating dynamic lymphatic status. Plast Reconstr Surg. 2011;127(3):74e-e76.
The Diagnosis and Treatment of Peripheral Lymphedema. 2016 Consensus Document of the International Society of Lymphology. Lymphology. 2016;49(4):170–84.
Chang DW, Suami H, Skoracki R. A prospective analysis of 100 consecutive lymphovenous bypass cases for treatment of extremity lymphedema. Plast Reconstr Surg. 2013;132(5):1305–14.
Yamamoto T, Narushima M, Doi K, Oshima A, Ogata F, Mihara M, et al. Characteristic indocyanine green lymphography findings in lower extremity lymphedema: the generation of a novel lymphedema severity staging system using dermal backflow patterns. Plast Reconstr Surg. 2011;127(5):1979–86.
Nguyen AT, Chang EI, Suami H, Chang DW. An algorithmic approach to simultaneous vascularized lymph node transfer with microvascular breast reconstruction. Ann Surg Oncol. 2015;22(9):2919–24.
Chang EI, Ibrahim A, Liu J, Robe C, Suami H, Hanasono MM, et al. Optimizing quality of life for patients with breast cancer-related lymphedema: a prospective study combining diep flap breast reconstruction and lymphedema surgery. Plast Reconstr Surg. 2020;145(4):676e-e685.
Bae JS, Yoo RE, Choi SH, Park SO, Chang H, Suh M, et al. Evaluation of lymphedema in upper extremities by MR lymphangiography: comparison with lymphoscintigraphy. Magn Reson Imaging. 2018;49:63–70.
Dayan JH, Dayan E, Smith ML. Reverse lymphatic map**: a new technique for maximizing safety in vascularized lymph node transfer. Plast Reconstr Surg. 2015;135(1):277–85.
∙ Koshima I, Inagawa K, Urushibara K, Moriguchi T. Supermicrosurgical lymphaticovenular anastomosis for the treatment of lymphedema in the upper extremities. J Reconstr Microsurg. 2000;16(6):437–42. *Seminal paper describing supermicrosurgery for LVA/LVB in early patients.
∙∙ Garza RM, Chang DW. Lymphovenous bypass for the treatment of lymphedema. J Surg Oncol. 2018;118(5):743–9. ** This paper reviews outcomes in LVA/LVB and includes the senior authors description of imaging, planning and technique
Campisi C, Boccardo F, Zilli A, Maccio A, Napoli F. Long-term results after lymphatic-venous anastomoses for the treatment of obstructive lymphedema. Microsurgery. 2001;21(4):135–9.
Pronin VAA, Zolotarevsky V, Rozanov Y, Savchenko T, Akimon A. Lymphovenous anastomosis for the prevention of post-mastectomy edema of the arm. Sov Med. 1989;4:32–5.
Boccardo FM, Casabona F, Friedman D, Puglisi M, De Cian F, Ansaldi F, et al. Surgical prevention of arm lymphedema after breast cancer treatment. Ann Surg Oncol. 2011;18(9):2500–5.
Jorgensen MG, Toyserkani NM, Sorensen JA. The effect of prophylactic lymphovenous anastomosis and shunts for preventing cancer-related lymphedema: a systematic review and meta-analysis. Microsurgery. 2018;38(5):576–85.
Boccardo F, Casabona F, De Cian F, Friedman D, Murelli F, Puglisi M, et al. Lymphatic microsurgical preventing healing approach (LYMPHA) for primary surgical prevention of breast cancer-related lymphedema: over 4 years follow-up. Microsurgery. 2014;34(6):421–4.
Feldman S, Bansil H, Ascherman J, Grant R, Borden B, Henderson P, et al. Single institution experience with Lymphatic Microsurgical Preventive Healing Approach (LYMPHA) for the primary prevention of lymphedema. Ann Surg Oncol. 2015;22(10):3296–301.
Agarwal S, Garza RM, Chang DW. Lymphatic Microsurgical Preventive Healing Approach (LYMPHA) for the prevention of secondary lymphedema. Breast J. 2020;26(4):721–4.
Ciudad P, Agko M, Perez Coca JJ, Manrique OJ, Chang WL, Nicoli F, et al. Comparison of long-term clinical outcomes among different vascularized lymph node transfers: 6-year experience of a single center’s approach to the treatment of lymphedema. J Surg Oncol. 2017;116(6):671–82.
Suami H, Scaglioni MF, Dixon KA, Tailor RC. Interaction between vascularized lymph node transfer and recipient lymphatics after lymph node dissection-a pilot study in a canine model. J Surg Res. 2016;204(2):418–27.
Cheng MH, Chen SC, Henry SL, Tan BK, Lin MC, Huang JJ. Vascularized groin lymph node flap transfer for postmastectomy upper limb lymphedema: flap anatomy, recipient sites, and outcomes. Plast Reconstr Surg. 2013;131(6):1286–98.
Cheng MH, Huang JJ, Nguyen DH, Saint-Cyr M, Zenn MR, Tan BK, et al. A novel approach to the treatment of lower extremity lymphedema by transferring a vascularized submental lymph node flap to the ankle. Gynecol Oncol. 2012;126(1):93–8.
Maldonado AA, Chen R, Chang DW. The use of supraclavicular free flap with vascularized lymph node transfer for treatment of lymphedema: a prospective study of 100 consecutive cases. J Surg Oncol. 2017;115(1):68–71.
Steinbacher J, Tinhofer IE, Meng S, Reissig LF, Placheta E, Roka-Palkovits J, et al. The surgical anatomy of the supraclavicular lymph node flap: a basis for the free vascularized lymph node transfer. J Surg Oncol. 2017;115(1):60–2.
Barreiro GC, Baptista RR, Kasai KE, dos Anjos DM, Busnardo Fde F, Modolin M, et al. Lymph fasciocutaneous lateral thoracic artery flap: anatomical study and clinical use. J Reconstr Microsurg. 2014;30(6):389–96.
Smith ML, Molina BJ, Dayan E, Saint-Victor DS, Kim JN, Kahn ES, et al. Heterotopic vascularized lymph node transfer to the medial calf without a skin paddle for restoration of lymphatic function: proof of concept. J Surg Oncol. 2017;115(1):90–5.
Chu CK, Schaverien MV, Chang EI, Hanson SE, Hanasono MM, Selber JC. Intra-abdominal lymph nodes: a privileged donor site for vascularized lymph node transfer. Plast Reconstr Surg Glob Open. 2020;8(3).
Nguyen AT, Suami H, Hanasono MM, Womack VA, Wong FC, Chang EI. Long-term outcomes of the minimally invasive free vascularized omental lymphatic flap for the treatment of lymphedema. J Surg Oncol. 2017;115(1):84–9.
Coriddi M, Wee C, Meyerson J, Eiferman D, Skoracki R. Vascularized jejunal mesenteric lymph node transfer: a novel surgical treatment for extremity lymphedema. J Am Coll Surg. 2017;225(5):650–7.
Schaverien MV, Hofstetter WL, Selber JC. Vascularized jejunal mesenteric lymph node transfer for lymphedema: a novel approach. Plast Reconstr Surg. 2018;141(3):468e-e469.
∙ Scaglioni MF, Arvanitakis M, Chen YC, Giovanoli P, Chia-Shen Yang J, Chang EI. Comprehensive review of vascularized lymph node transfers for lymphedema: outcomes and complications. Microsurgery. 2018;38(2):222–9. *This manuscript reviews all currently described donor sites for vascularized lymph node transfers and summarizes the available literature on outcomes of each.
Kenworthy EO, Nelson JA, Verma R, Mbabuike J, Mehrara BJ, Dayan JH. Double vascularized omentum lymphatic transplant (VOLT) for the treatment of lymphedema. J Surg Oncol. 2018;117(7):1413–9.
Hanson SE, Chang EI, Schaverien MV, Chu C, Selber JC, Hanasono MM. Controversies in surgical management of lymphedema. Plast Reconstr Surg Glob Open. 2020;8(3):e2675.
Basta MN, Gao LL, Wu LC. Operative treatment of peripheral lymphedema: a systematic meta-analysis of the efficacy and safety of lymphovenous microsurgery and tissue transplantation. Plast Reconstr Surg. 2014;133(4):905–13.
∙ Carl HM, Walia G, Bello R, Clarke-Pearson E, Hassanein AH, Cho B, et al. Systematic review of the surgical treatment of extremity lymphedema. J Reconstr Microsurg. 2017;33(6):412–25. This is the most recent polled analysis of surgical treatment options but illustrates the need for standardized outcomes and long term data collection.
Cheng MH, Loh CYY, Lin CY. Outcomes of vascularized lymph node transfer and lymphovenous anastomosis for treatment of primary lymphedema. Plast Reconstr Surg Glob Open. 2018;6(12):e2056.
Winters H, Tielemans HJP, Verhulst AC, Paulus VAA, Slater NJ, Ulrich DJO. The long-term patency of lymphaticovenular anastomosis in breast cancer-related lymphedema. Ann Plast Surg. 2019;82(2):196–200.
Forte AJ, Cinotto G, Boczar D, Huayllani MT, Lu X, Manrique OJ, et al. Lymph node transfer combined with deep inferior epigastric perforators and transverse rectus abdominis myocutaneous procedures: a systematic review. Gland Surg. 2020;9(2):521–7.
Tourani SS, Taylor GI, Ashton MW. Long-term patency of lymphovenous anastomoses: a systematic review. Plast Reconstr Surg. 2016;138(2):492–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no commercial associations or financial disclosures that might pose or create a conflict of interest with information presented in this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical collection on Plastic Surgery.
Rights and permissions
About this article
Cite this article
Hanson, S.E., Chu, C.K. & Chang, E.I. Surgical Treatment Options of Breast Cancer-Related Lymphedema. Curr Surg Rep 9, 6 (2021). https://doi.org/10.1007/s40137-021-00286-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s40137-021-00286-6