Abstract
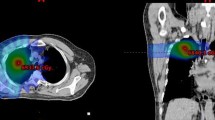
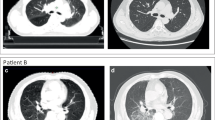
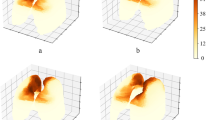
This study aimed to develop a predictive model using clinical, dosimetric, and radiomic features for radiation-induced pneumonitis (RP) after lung stereotactic body radiation therapy (SBRT). We retrospectively analyzed the clinical data of 153 patients who underwent SBRT for lung nodules between 2010 and 2019. A total of 3,350 radiomic computed tomography (CT) features of radiotherapy simulation (shape, intensity, texture, and log filters) were extracted. Among them, 30 factors were selected through Pearson’s correlation analysis and subjected to analysis. A proposed lung toxicity prediction model was developed using a deep neural network algorithm. The programming language used was Python. The data were divided into a training set (70% of data) and a test/validation set (30% of data). We adjusted the original data by oversampling to correct the uneven sample distribution to balance the data set. The Talos library was used in this study for hyperparameter determination and the model with the highest accuracy was selected. The Talos library provided the RP prediction model with the highest accuracy of 94.8%. The area under the curve of the receiver operating characteristics curve was 0.90, which was relatively fair. It showed relatively high accuracy in the RP prediction model based on the clinical, dosimetric, and radiomic factors of patients who received SBRT for lung nodules. A further study using more cases from other medical centers is being planned for external validation.






Similar content being viewed by others
References
S.W. Lee, E.K. Choi, H.J. Park, S.D. Ahn, J.H. Kim, K.J. Kim, S.M. Yoon, Y.S. Kim, B.Y. Yi, Stereotactic body frame based fractionated radiosurgery on consecutive days for primary or metastatic tumors in the lung. Lung Cancer (Amst Netherlands) 40, 309 (2003). https://doi.org/10.1016/s0169-5002(03)00040-0
G.M. Videtic, C.A. Reddy, L. Sorenson, A prospective study of quality of life including fatigue and pulmonary function after stereotactic body radiotherapy for medically inoperable early-stage lung cancer. Support Care Cancer 21, 211 (2013). https://doi.org/10.1007/s00520-012-1513-9
H. Onishi, H. Shirato, Y. Nagata, M. Hiraoka, M. Fu**o, K. Gomi, K. Karasawa, K. Hayakawa, Y. Niibe, Y. Takai, T. Kimura, A. Takeda, A. Ouchi, M. Hareyama, M. Kokubo, T. Kozuka, T. Arimoto, R. Hara, J. Itami, T. Araki, Stereotactic body radiotherapy (SBRT) for operable stage I non-small-cell lung cancer: can SBRT be comparable to surgery? Int. J. Radiat. Oncol. Biol. Phys. 81, 1352 (2011). https://doi.org/10.1016/j.ijrobp.2009.07.1751
N.E. Verstegen, J.W. Oosterhuis, D.A. Palma, G. Rodrigues, F.J. Lagerwaard, A. van der Elst, R. Mollema, W.F. van Tets, A. Warner, J.J. Joosten, M.I. Amir, C.J. Haasbeek, E.F. Smit, B.J. Slotman, S. Senan, Stage I-II non-small-cell lung cancer treated using either stereotactic ablative radiotherapy (SABR) or lobectomy by video-assisted thoracoscopic surgery (VATS): outcomes of a propensity score-matched analysis. Ann. Oncol. 24, 1543 (2013). https://doi.org/10.1093/annonc/mdt026
G.M. Videtic, C. Hu, A.K. Singh, J.Y. Chang, W. Parker, K.R. Olivier, S.E. Schild, R. Komaki, J.J. Urbanic, R.D. Timmerman, H. Choy, A randomized phase 2 study comparing 2 stereotactic body radiation therapy schedules for medically inoperable patients with stage I peripheral non-small cell lung cancer: NRG oncology RTOG 0915 (NCCTG N0927). Int. J. Radiat. Oncol. Biol. Phys. 93, 757 (2015). https://doi.org/10.1016/j.ijrobp.2015.07.2260
M. Guckenberger, T. Krieger, A. Richter, K. Baier, J. Wilbert, R.A. Sweeney, M. Flentje, Potential of image-guidance, gating and real-time tracking to improve accuracy in pulmonary stereotactic body radiotherapy. Radiother. Oncol. 91, 288 (2009). https://doi.org/10.1016/j.radonc.2008.08.010
R.A. Sweeney, B. Seubert, S. Stark, V. Homann, G. Müller, M. Flentje, M. Guckenberger, Accuracy and inter-observer variability of 3D versus 4D cone-beam CT based image-guidance in SBRT for lung tumors. Radiat. Oncol. 7, 81 (2012). https://doi.org/10.1186/1748-717x-7-81
E.M. Harder, H.S. Park, Z.J. Chen, R.H. Decker, Pulmonary dose-volume predictors of radiation pneumonitis following stereotactic body radiation therapy. Pract. Radiat. Oncol. 6, e353 (2016). https://doi.org/10.1016/j.prro.2016.01.015
G. Valdes, T.D. Solberg, M. Heskel, L. Ungar, C.B. Simone 2nd., Using machine learning to predict radiation pneumonitis in patients with stage I non-small cell lung cancer treated with stereotactic body radiation therapy. Phys. Med. Biol. 61, 6105 (2016). https://doi.org/10.1088/0031-9155/61/16/6105
M. Yakar, D. Etiz, M. Metintas, G. Ak, O. Celik, Prediction of radiation pneumonitis with machine learning in stage III lung cancer: a pilot study. Technol. Cancer Res. Treat. 20, 15330338211016372 (2021). https://doi.org/10.1177/15330338211016373
A.J. Hope, P.E. Lindsay, I. El Naqa, J.R. Alaly, M. Vicic, J.D. Bradley, J.O. Deasy, Modeling radiation pneumonitis risk with clinical, dosimetric, and spatial parameters. Int. J. Radiat. Oncol. Biol. Phys. 65, 112 (2006). https://doi.org/10.1016/j.ijrobp.2005.11.046
R.J. Klement, M. Allgäuer, S. Appold, K. Dieckmann, I. Ernst, U. Ganswindt, R. Holy, U. Nestle, M. Nevinny-Stickel, S. Semrau, F. Sterzing, A. Wittig, N. Andratschke, M. Guckenberger, Support vector machine-based prediction of local tumor control after stereotactic body radiation therapy for early-stage non-small cell lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 88, 732 (2014). https://doi.org/10.1016/j.ijrobp.2013.11.216
T. Adachi, M. Nakamura, T. Shintani, T. Mitsuyoshi, R. Kakino, T. Ogata, T. Ono, H. Tanabe, M. Kokubo, T. Sakamoto, Y. Matsuo, T. Mizowaki, Multi-institutional dose-segmented dosiomic analysis for predicting radiation pneumonitis after lung stereotactic body radiation therapy. Med. Phys. 48, 1781 (2021). https://doi.org/10.1002/mp.14769
S.P. Krafft, A. Rao, F. Stingo, T.M. Briere, L.E. Court, Z. Liao, M.K. Martel, The utility of quantitative CT radiomics features for improved prediction of radiation pneumonitis. Med. Phys. 45, 5317 (2018). https://doi.org/10.1002/mp.13150
H. Kim, C.M. Park, J.M. Goo, J.E. Wildberger, H.U. Kauczor, Quantitative computed tomography imaging biomarkers in the diagnosis and management of lung cancer. Invest. Radiol. 50, 571 (2015). https://doi.org/10.1097/rli.0000000000000152
D. De Ruysscher, H. Sharifi, G. Defraene, S.L. Kerns, M. Christiaens, K. De Ruyck, S. Peeters, J. Vansteenkiste, R. Jeraj, F. Van Den Heuvel, W. van Elmpt, Quantification of radiation-induced lung damage with CT scans: the possible benefit for radiogenomics. Acta Oncol. 52, 1405 (2013). https://doi.org/10.3109/0284186x.2013.813074
D.A. Palma, J. van Sörnsen, W.F. de Koste, A. Verbakel, S.S. Vincent, Lung density changes after stereotactic radiotherapy: a quantitative analysis in 50 patients. Int. J. Radiat. Oncol. Biol. Phys. 81, 974 (2011). https://doi.org/10.1016/j.ijrobp.2010.07.025
I. Kyas, H. Hof, J. Debus, W. Schlegel, C.P. Karger, Prediction of radiation-induced changes in the lung after stereotactic body radiation therapy of non-small-cell lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 67, 768 (2007). https://doi.org/10.1016/j.ijrobp.2006.08.066
G. Defraene, W. van Elmpt, W. Crijns, P. Slagmolen, D. De Ruysscher, CT characteristics allow identification of patient-specific susceptibility for radiation-induced lung damage. Radiother. Oncol. 117, 29 (2015). https://doi.org/10.1016/j.radonc.2015.07.033
E. Huynh, T.P. Coroller, V. Narayan, V. Agrawal, Y. Hou, J. Romano, I. Franco, R.H. Mak, H.J. Aerts, CT-based radiomic analysis of stereotactic body radiation therapy patients with lung cancer. Radiother. Oncol. 120, 258 (2016). https://doi.org/10.1016/j.radonc.2016.05.024
B. Liang, Y. Tian, X. Chen, H. Yan, L. Yan, T. Zhang, Z. Zhou, L. Wang, J. Dai, Prediction of radiation pneumonitis with dose distribution: a convolutional neural network (CNN) based model. Front. Oncol. 9, 1500 (2019). https://doi.org/10.3389/fonc.2019.01500
X. Zhen, J. Chen, Z. Zhong, B. Hrycushko, L. Zhou, S. Jiang, K. Albuquerque, X. Gu, Deep convolutional neural network with transfer learning for rectum toxicity prediction in cervical cancer radiotherapy: a feasibility study. Phys. Med. Biol. 62, 8246 (2017). https://doi.org/10.1088/1361-6560/aa8d09
B. Ibragimov, D. Toesca, D. Chang, Y. Yuan, A. Koong, L. **ng, Development of deep neural network for individualized hepatobiliary toxicity prediction after liver SBRT. Med. Phys. 45, 4763 (2018). https://doi.org/10.1002/mp.13122
M. D. Anderson, Cancer center head and neck quantitative imaging working group, investigation of radiomic signatures for local recurrence using primary tumor texture analysis in oropharyngeal head and neck cancer patients, Sci. Rep. 8, 1524 (2018). https://doi.org/10.1038/s41598-017-14687-0
S.P. Shayesteh, A. Alikhassi, F. Farhan, R. Ghalehtaki, M. Soltanabadi, P. Haddad, A. Bitarafan-Rajabi, Prediction of response to neoadjuvant chemoradiotherapy by mri-based machine learning texture analysis in rectal cancer patients. J Gastrointest Cancer 51, 601 (2020). https://doi.org/10.1007/s12029-019-00291-0
L. Lu, S. H. Sun, H. Yang, L. E, P. Guo, L. H. Schwartz, B. Zhao, Radiomics prediction of EGFR status in lung cancer-our experience in using multiple feature extractors and the cancer imaging archive data, tomography 6, 223 (2020). https://doi.org/10.18383/j.tom.2020.00017
F. Chollet, Keras: the python deep learning library, astrophysics source code library, ascl: 1806.022 (2018)
2022 GitHub Inc., Hyperparameter Optimization for TensorFlow, Keras and PyTorch, http://github.com/autonomio/talos, Accessed 21 January 2022.
S. Yamaguchi, T. Ohguri, S. Ide, T. Aoki, H. Imada, K. Yahara, H. Narisada, Y. Korogi, Stereotactic body radiotherapy for lung tumors in patients with subclinical interstitial lung disease: the potential risk of extensive radiation pneumonitis, Lung cancer (Amst, Netherlands) 82, 260 (2013). https://doi.org/10.1016/j.lungcan.2013.08.024
N. Ueki, Y. Matsuo, Y. Togashi, T. Kubo, K. Shibuya, Y. Iizuka, T. Mizowaki, K. Togashi, M. Mishima, M. Hiraoka, Impact of pretreatment interstitial lung disease on radiation pneumonitis and survival after stereotactic body radiation therapy for lung cancer. J. Thora. Oncol. 10, 116 (2015). https://doi.org/10.1097/jto.0000000000000359
T. Yoshitake, Y. Shioyama, K. Asai, K. Nakamura, T. Sasaki, S. Ohga, T. Kamitani, T. Yamaguchi, K. Ohshima, K. Matsumoto, S. Kawanami, H. Honda, Impact of interstitial changes on radiation pneumonitis after stereotactic body radiation therapy for lung cancer. Anticancer Res. 35, 4909 (2015)
T.A. Hirose, H. Arimura, K. Ninomiya, T. Yoshitake, J.I. Fukunaga, Y. Shioyama, Radiomic prediction of radiation pneumonitis on pretreatment planning computed tomography images prior to lung cancer stereotactic body radiation therapy. Sci Rep 10, 20424 (2020). https://doi.org/10.1038/s41598-020-77552-7
H. Yamashita, S. Kobayashi-Shibata, A. Terahara, K. Okuma, A. Haga, R. Wakui, K. Ohtomo, K. Nakagawa, Prescreening based on the presence of CT-scan abnormalities and biomarkers (KL-6 and SP-D) may reduce severe radiation pneumonitis after stereotactic radiotherapy. Radiat Oncol 5, 32 (2010). https://doi.org/10.1186/1748-717x-5-32
N. Nakajima, Y. Sugawara, M. Kataoka, Y. Hamamoto, T. Ochi, S. Sakai, T. Takahashi, M. Kajihara, N. Teramoto, M. Yamashita, T. Mochizuki, Differentiation of tumor recurrence from radiation-induced pulmonary fibrosis after stereotactic ablative radiotherapy for lung cancer: characterization of 18F-FDG PET/CT findings. Ann Nucl Med 27, 261 (2013). https://doi.org/10.1007/s12149-012-0682-4
A. Cunliffe, S.G. Armato 3rd., R. Castillo, N. Pham, T. Guerrero, H.A. Al-Hallaq, Lung texture in serial thoracic computed tomography scans: correlation of radiomics-based features with radiation therapy dose and radiation pneumonitis development. Int. J. Radiat. Oncol. Biol. Phys. 91, 1048 (2015). https://doi.org/10.1016/j.ijrobp.2014.11.030
A. Pella, R. Cambria, M. Riboldi, B.A. Jereczek-Fossa, C. Fodor, D. Zerini, A.E. Torshabi, F. Cattani, C. Garibaldi, G. Pedroli, G. Baroni, R. Orecchia, Use of machine learning methods for prediction of acute toxicity in organs at risk following prostate radiotherapy. Med. Phys. 38, 2859 (2011). https://doi.org/10.1118/1.3582947
H. Abdollahi, S. Mostafaei, S. Cheraghi, I. Shiri, S. Rabi Mahdavi, A. Kazemnejad, Cochlea CT radiomics predicts chemoradiotherapy induced sensorineural hearing loss in head and neck cancer patients: a machine learning and multi-variable modelling study, Phys Med 45, 192 (2018). https://doi.org/10.1016/j.ejmp.2017.10.008
S. Sharma, M. Parmar, Heart diseases prediction using deep learning neural network model, Int. J. Innov. Technol. Explor. Eng. (IJITEE) 9 (2020)
D. Gunning, Explainable artificial intelligence, Defense Advanced Research Projects Agency (DARPA), 2 (2017)
L. H. Gilpin, D. Bau, B. Z. Yuan, A. Bajwa, M. Specter, L. Kagal, in 2018 IEEE 5th International Conference on data science and advanced analytics (DSAA), 80 (2018)
Acknowledgements
This study was supported by the Research Fund of Seoul St. Mary’s Hospital, The Catholic University of Korea.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Choi, K.H., Seol, Y., Kang, Yn. et al. Using deep learning to predict radiation pneumonitis in patients treated with stereotactic body radiotherapy (SBRT) for pulmonary nodules: preliminary results. J. Korean Phys. Soc. 81, 460–470 (2022). https://doi.org/10.1007/s40042-022-00543-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40042-022-00543-6