Abstract
Purpose of Review
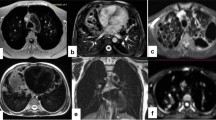
Bronchiectasis is the permanent abnormal dilation of the airways and can be associated with various pathogeneses and outcomes. Proper diagnosis and evaluation of bronchiectasis employs x-ray CT, though emerging research has also shown MRI to be sensitive to the disease. The goal of this article is to review recent research in CT and MRI of bronchiectasis and associated diseases.
Recent Findings
Techniques in quantitative CT continue to improve and may improve consistency in bronchiectasis evaluation and reduce reader scoring load. While CT is the “gold standard” for evaluation of bronchiectasis, new techniques in magnetic resonance imaging have dramatically increased in sensitivity to bronchiectasis though without patient exposure to ionizing radiation. MRI may therefore be an attractive alternative to CT in some cases, yet further clinical trials are necessary.
Summary
Although bronchiectasis is an irreversible disease, new understanding of airway structure-function relationships may improve clinical management.




Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Bueno J, Flors L. The role of imaging in the diagnosis of bronchiectasis: the key is in the distribution. Radiología. 2018;60(1):39–48. https://doi.org/10.1016/j.rxeng.2017.06.005This paper describes the current practices of bronchiectasis diagnosis, imaging findings, and their classification.
Gallucci M, di Palmo E, Bertelli L, Camela F, Ricci G, Pession A. A pediatric disease to keep in mind: diagnostic tools and management of bronchiectasis in pediatric age. Ital J Pediatr. 2017;43(1):117. https://doi.org/10.1186/s13052-017-0434-0.
Chan ED, Iseman MD. Bronchiectasis. In: Murray & Nadel’s textbook of respiratory medicine. Philadelphia: Saunders Elsevier; 2016. p. 2064.
Weycker D, Hansen GL, Seifer FD. Prevalence and incidence of noncystic fibrosis bronchiectasis among US adults in 2013. Chron Respir Dis. 2017;14(4):377–84. https://doi.org/10.1177/1479972317709649.
Contarini M, Finch S, Chalmers JD. Bronchiectasis: a case-based approach to investigation and management. Eur Respir Rev. 2018;27(149). https://doi.org/10.1183/16000617.0016-2018.
• Singh A, Bhalla AS, Jana M. Bronchiectasis revisited: imaging-based pattern approach to diagnosis. Curr Probl Diagn Radiol. 2019;48(1):53–60. https://doi.org/10.1067/j.cpradiol.2017.12.001This article discusses image-based algorithmic approaches towards the etiological diagnosis of bronchiectasis.
Verbanck S, et al. The quantitative link of lung clearance index to bronchial segments affected by bronchiectasis. Thorax. 2018;73(1):82–4. https://doi.org/10.1136/thoraxjnl-2017-210496.
Biederer J, Mirsadraee S, Beer M, Molinari F, Hintze C, Bauman G, et al. MRI of the lung (3/3)-current applications and future perspectives. Insights Imaging. 2012;3(4):373–86. https://doi.org/10.1007/s13244-011-0142-z.
Perera PL, Screaton NJ. Radiological features of bronchiectasis. 2011:44–67. https://doi.org/10.1183/1025448x.10003510.
Murphy KP, Maher MM, O'Connor OJ. Imaging of cystic fibrosis and pediatric bronchiectasis. AJR Am J Roentgenol. 2016;206(3):448–54. https://doi.org/10.2214/AJR.15.14437.
•• Hill AT, et al. British Thoracic Society Guideline for bronchiectasis in adults. Thorax. 2019;74(Suppl 1):1–69. https://doi.org/10.1136/thoraxjnl-2018-212463British Thoracic Society provided a detail guideline and good practice points in the diagnosis, treatment, and management of bronchiectasis.
Kim JS, Müller NL, Park CS, Grenier P, Herold CJ. Cylindrical bronchiectasis: diagnostic findings in thin-section CT. Am J Roentgenol. 1997;168(3):751–4.
Webb WR, Muller NL, Naidich DP. Standardized terms for high-resolution computed tomography of the lung: a proposed glossary. J Thorac Imaging. 1993;8(3):167–75.
Reid LM. Reduction in bronchial subdivision in bronchiectasis. Thorax. 1950;5(3):233–47.
Milliron B, et al. Bronchiectasis: mechanisms and imaging clues of associated common and uncommon diseases. Radiographics. 2015;35(4):1011–30. https://doi.org/10.1148/rg.2015140214.
Reiff DB, Wells AU, Carr DH, Cole PJ, Hansell DM. CT findings in bronchiectasis: limited value in distinguishing between idiopathic and specific types. AJR Am J Roentgenol. 1995;165(2):261–7. https://doi.org/10.2214/ajr.165.2.7618537.
Agarwal R, Gupta D, Aggarwal AN, Saxena AK, Chakrabarti A, **dal SK. Clinical significance of hyperattenuating mucoid impaction in allergic bronchopulmonary aspergillosis: an analysis of 155 patients. Chest. 2007;132(4):1183–90. https://doi.org/10.1378/chest.07-0808.
Aksamit TR, O'Donnell AE, Barker A, Olivier KN, Winthrop KL, Daniels MLA, et al. Adult patients with bronchiectasis: a first look at the US bronchiectasis research registry. Chest. 2017;151(5):982–92. https://doi.org/10.1016/j.chest.2016.10.055.
Cantin L, Bankier AA, Eisenberg RL. Bronchiectasis. AJR Am J Roentgenol. 2009;193(3):W158–71. https://doi.org/10.2214/AJR.09.3053.
Kwak N, Lee CH, Lee HJ, Kang YA, Lee JH, Han SK, et al. Non-tuberculous mycobacterial lung disease: diagnosis based on computed tomography of the chest. Eur Radiol. 2016;26(12):4449–56. https://doi.org/10.1007/s00330-016-4286-6.
• Rademacher J, Welte T. Bronchiectasis--diagnosis and treatment. Dtsch Arztebl Int. 2011;108(48):809–15. https://doi.org/10.3238/arztebl.2011.0809This is a review article about the diagnostic evaluation and treatment in patients with non-cystic fibrosis bronchictasis.
Dodd JD, Souza CA, Muller NL. Conventional high-resolution CT versus helical high-resolution MDCT in the detection of bronchiectasis. AJR Am J Roentgenol. 2006;187(2):414–20. https://doi.org/10.2214/AJR.05.0723.
Hill LE, Ritchie G, Wightman AJ, Hill AT, Murchison JT. Comparison between conventional interrupted high-resolution CT and volume multidetector CT acquisition in the assessment of bronchiectasis. Br J Radiol. 2010;83(985):67–70. https://doi.org/10.1259/bjr/96908158.
Bhalla M, Turcios N, Aponte V, Jenkins M, Leitman BS, McCauley D, et al. Cystic fibrosis: scoring system with thin-section CT. Radiology. 1991;179(3):783–8. https://doi.org/10.1148/radiology.179.3.2027992.
Brody AS, Klein JS, Molina PL, Quan J, Bean JA, Wilmott RW. High-resolution computed tomography in young patients with cystic fibrosis: distribution of abnormalities and correlation with pulmonary function tests. J Pediatr. 2004;145(1):32–8. https://doi.org/10.1016/j.jpeds.2004.02.038.
Nathanson I, et al. Ultrafast computerized tomography of the chest in cystic fibrosis: a new scoring system. Pediatr Pulmonol. 1991;11(1):81–6. https://doi.org/10.1002/ppul.1950110112.
Naidich DP, et al. Computed tomography of bronchiectasis. J Comput Assist Tomogr. 1982;6(3):437–44.
Diaz AA, Young TP, Maselli DJ, Martinez CH, Gill R, Nardelli P, et al. Quantitative CT measures of bronchiectasis in smokers. Chest. 2017;151(6):1255–62. https://doi.org/10.1016/j.chest.2016.11.024.
Parr DG, Guest PG, Reynolds JH, Dowson LJ, Stockley RA. Prevalence and impact of bronchiectasis in alpha1-antitrypsin deficiency. Am J Respir Crit Care Med. 2007;176(12):1215–21. https://doi.org/10.1164/rccm.200703-489OC.
de Brito MC, et al. Radiologist agreement on the quantification of bronchiectasis by high-resolution computed tomography. Radiol Bras. 2017;50(1):26–31. https://doi.org/10.1590/0100-3984.2015.0146.
Alzeer AH. HRCT score in bronchiectasis: correlation with pulmonary function tests and pulmonary artery pressure. Ann Thorac Med. 2008;3(3):82–6. https://doi.org/10.4103/1817-1737.39675.
Chalmers JD, Goeminne P, Aliberti S, McDonnell M, Lonni S, Davidson J, et al. The bronchiectasis severity index. An international derivation and validation study. Am J Respir Crit Care Med. 2014;189(5):576–85. https://doi.org/10.1164/rccm.201309-1575OC.
Martinez-Garcia MA, et al. Multidimensional approach to non-cystic fibrosis bronchiectasis: the FACED score. Eur Respir J. 2014;43(5):1357–67. https://doi.org/10.1183/09031936.00026313.
Rosales-Mayor E, Polverino E, Raguer L, Alcaraz V, Gabarrus A, Ranzani O, et al. Comparison of two prognostic scores (BSI and FACED) in a Spanish cohort of adult patients with bronchiectasis and improvement of the FACED predictive capacity for exacerbations. PLoS One. 2017;12(4):e0175171. https://doi.org/10.1371/journal.pone.0175171.
Costa JC, et al. The Bronchiectasis Severity Index and FACED score for assessment of the severity of bronchiectasis. Pulmonology. 2018. https://doi.org/10.1016/j.rppnen.2017.08.009.
Webb WR, Muller NL, Naidich DP. High-Resolution CT of the Lung. 4th ed. Lippincott Williams and Wilkins; 2009. p. 603.
• Pu J, et al. CT based computerized identification and analysis of human airways: a review. Med Phys. 2012;39(5):2603–16. https://doi.org/10.1118/1.4703901This review article is based on computerized identification and analysis of human airways.
Quan K, et al. Tapering analysis of airways with bronchiectasis. Proc. SPIE 10574, Medical Imaging 2018: Image Processing, 105742G (2018). https://doi.org/10.1117/12.2292306.
Aykac D, Hoffman EA, McLennan G, Reinhardt JM. Segmentation and analysis of the human airway tree from three-dimensional X-ray CT images. IEEE Trans Med Imaging. 2003;22(8):940–50. https://doi.org/10.1109/TMI.2003.815905.
Estepar RS, et al. Accurate airway wall estimation using phase congruency. Med Image Comput Comput Assist Interv. 2006;9(Pt 2):125–34.
Fabijanska A. Two-pass region growing algorithm for segmenting airway tree from MDCT chest scans. Comput Med Imaging Graph. 2009;33(7):537–46. https://doi.org/10.1016/j.compmedimag.2009.04.012.
Gu S, Fuhrman C, Meng X, Siegfried JM, Gur D, Leader JK, et al. Computerized identification of airway wall in CT examinations using a 3D active surface evolution approach. Med Image Anal. 2013;17(3):283–96. https://doi.org/10.1016/j.media.2012.11.003.
Mori K, et al. Recognition of bronchus in three-dimensional X-ray CT images with applications to virtualized bronchoscopy system, in Proceedings of 13th International Conference on Pattern Recognition. 1996. Vienna, Austria. p. 528–532.
Kiraly AP, Higgins WE, McLennan G, Hoffman EA, Reinhardt JM. Three-dimensional human airway segmentation methods for clinical virtual bronchoscopy. Acad Radiol. 2002;9(10):1153–68. https://doi.org/10.1016/S1076-6332(03)80517-2.
Lo P, Sporring J, Ashraf H, Pedersen JJ, de Bruijne M. Vessel-guided airway tree segmentation: a voxel classification approach. Med Image Anal. 2010;14(4):527–38. https://doi.org/10.1016/j.media.2010.03.004.
Nakano Y, Muro S, Sakai H, Hirai T, Chin K, Tsukino M, et al. Computed tomographic measurements of airway dimensions and emphysema in smokers. Correlation with lung function. Am J Respir Crit Care Med. 2000;162(3 Pt 1):1102–8. https://doi.org/10.1164/ajrccm.162.3.9907120.
Ochs RA, et al. Automated classification of lung bronchovascular anatomy in CT using AdaBoost. Med Image Anal. 2007;11(3):315–24. https://doi.org/10.1016/j.media.2007.03.004.
Ortner M, et al. 3D vector flow guided segmentation of airway wall in MSCT. In: Proceedings of the 6th International Conference on Advances in Visual Computing 2010. Springer: Las Vegas, NV. p. 302–311.
Saba OI, Hoffman EA, Reinhardt JM. Maximizing quantitative accuracy of lung airway lumen and wall measures obtained from X-ray CT imaging. J Appl Physiol (1985). 2003;95(3):1063–75. https://doi.org/10.1152/japplphysiol.00962.2002.
Sonka M, Park W, Hoffman EA. Rule-based detection of intrathoracic airway trees. IEEE Trans Med Imaging. 1996;15(3):314–26. https://doi.org/10.1109/42.500140.
DeBoer EM, et al. Automated CT scan scores of bronchiectasis and air trap** in cystic fibrosis. Chest. 2014;145(3):593–603. https://doi.org/10.1378/chest.13-0588.
• Yu N, et al. Computerized identification of bronchiectasis using a 3D quantitative CT protocol. J Med Imaging Health Inform. 2016;6(5):1303–8. https://doi.org/10.1166/jmihi.2016.1917This study proposes a novel three-dimensional automatic method to identify bronchiectasis.
Xu Z, Bagci U, Foster B, Mansoor A, Udupa JK, Mollura DJ. A hybrid method for airway segmentation and automated measurement of bronchial wall thickness on CT. Med Image Anal. 2015;24(1):1–17. https://doi.org/10.1016/j.media.2015.05.003.
Perez-Rovira A, et al. Automatic airway-artery analysis on lung CT to quantify airway wall thickening and bronchiectasis. Med Phys. 2016;43(10). https://doi.org/10.1118/1.4963214.
Odry BL, et al. An evaluation of automated broncho-arterial ratios for reliable assessment of bronchiectasis. Proceedings of SPIE - The International Society for Optical Engineering 6915, 2008. https://doi.org/10.1117/12.772579.
Meng Q, et al. Accurate airway segmentation based on intensity structure analysis and graph-cut. Proceedings of the SPIE 2016. 97842G. https://doi.org/10.1117/12.2216670.
Charbonnier JP, Rikxoort EMV, Setio AAA, Schaefer-Prokop CM, Ginneken BV, Ciompi F. Improving airway segmentation in computed tomography using leak detection with convolutional networks. Med Image Anal. 2017;36:52–60. https://doi.org/10.1016/j.media.2016.11.001.
Weinheimer, O., et al., Fully automated lobe-based airway taper index calculation in a low dose MDCT CF study over 4 time-points. Medical Imaging: Image Processing. 2017. https://doi.org/10.1117/12.2254387.
Juarez AGU, Tiddens H, de Bruijne M. Automatic airway segmentation in chest CT using convolutional neural networks. Image Analysis for Moving Organ, Breast, and Thoracic Images. 2018. p. 238–250. https://doi.org/10.1007/978-3-030-00946-5_24.
Naseri Z, Sherafat S, Abrishami Moghaddam H, Modaresi M, Pak N, Zamani F. Semi-automatic methods for airway and adjacent vessel measurement in bronchiectasis patterns in lung HRCT images of cystic fibrosis patients. J Digit Imaging. 2018;31(5):727–37. https://doi.org/10.1007/s10278-018-0076-9.
•• Roach DJ, et al. Ultrashort echo-time magnetic resonance imaging is a sensitive method for the evaluation of early cystic fibrosis lung disease. Ann Am Thorac Soc. 2016;13(11):1923–31. https://doi.org/10.1513/AnnalsATS.201603-203OCThis paper compares ultrashort echo time MR image (UTE MRI) with conventional computed tomography (CT) and showed significant correlation in their imaging scores with CF patients.
Kruger SJ, Fain SB, Johnson KM, Cadman RV, Nagle SK. Oxygen-enhanced 3D radial ultrashort echo time magnetic resonance imaging in the healthy human lung. NMR Biomed. 2014;27(12):1535–41. https://doi.org/10.1002/nbm.3158.
Ma W, Sheikh K, Svenningsen S, Pike D, Guo F, Etemad-Rezai R, et al. Ultra-short echo-time pulmonary MRI: evaluation and reproducibility in COPD subjects with and without bronchiectasis. J Magn Reson Imaging. 2015;41(5):1465–74. https://doi.org/10.1002/jmri.24680.
Ohno Y, et al. Pulmonary high-resolution ultrashort TE MR imaging: comparison with thin-section standard- and low-dose computed tomography for the assessment of pulmonary parenchyma diseases. J Magn Reson Imaging. 2016;43(2):512–32. https://doi.org/10.1002/jmri.25008.
Altes TA, Eichinger M, Puderbach M. Magnetic resonance imaging of the lung in cystic fibrosis. Proc Am Thorac Soc. 2007;4(4):321–7. https://doi.org/10.1513/pats.200611-181HT.
•• Svenningsen S, et al. Noncystic fibrosis bronchiectasis: regional abnormalities and response to airway clearance therapy using pulmonary functional magnetic resonance imaging. Acad Radiol. 2017;24(1):4–12. https://doi.org/10.1016/j.acra.2016.08.021This paper showed the capability of hyperpolarized gas MRI in finding the structure-function abnormalities in patients with non-cystic fibrosis bronchiectasis which CT could not detect and it also responded to airway clearance therapy (ACT).
Eichinger M, et al. Contrast-enhanced 3D MRI of lung perfusion in children with cystic fibrosis--initial results. Eur Radiol. 2006;16(10):2147–52. https://doi.org/10.1007/s00330-006-0257-7.
Fiel SB, et al. Magnetic resonance imaging in young adults with cystic fibrosis. Chest. 1987;91:181–4.
Fink C, et al. Partially parallel three-dimensional magnetic resonance imaging for the assessment of lung perfusion--initial results. Investig Radiol. 2003;38(8):482–8. https://doi.org/10.1097/01.rli.0000067490.97837.82.
Heidemann RM, Griswold MA, Kiefer B, Nittka M, Wang J, Jellus V, et al. Resolution enhancement in lung 1H imaging using parallel imaging methods. Magn Reson Med. 2003;49(2):391–4. https://doi.org/10.1002/mrm.10349.
Puderbach M, Eichinger M, Gahr J, Ley S, Tuengerthal S, Schmähl A, et al. Proton MRI appearance of cystic fibrosis: comparison to CT. Eur Radiol. 2007;17(3):716–24. https://doi.org/10.1007/s00330-006-0373-4.
Mayer D, et al. Hybrid segmentation and virtual bronchoscopy based on CT images. Acad Radiol. 2004;11(5):551–65. https://doi.org/10.1016/j.acra.2004.01.012.
Sodhi KS, Gupta P, Shrivastav A, Saxena AK, Mathew JL, Singh M, et al. Evaluation of 3 T lung magnetic resonance imaging in children with allergic bronchopulmonary aspergillosis: pilot study. Eur J Radiol. 2019;111:88–92. https://doi.org/10.1016/j.ejrad.2018.12.021.
Eichinger M, Optazaite DE, Kopp-Schneider A, Hintze C, Biederer J, Niemann A, et al. Morphologic and functional scoring of cystic fibrosis lung disease using MRI. Eur J Radiol. 2012;81(6):1321–9. https://doi.org/10.1016/j.ejrad.2011.02.045.
Helbich TH, et al. Cystic fibrosis: CT assessment of lung involvement in children and adults. Radiology. 1999;213(2):537–44. https://doi.org/10.1148/radiology.213.2.r99nv04537.
Sileo C, Corvol H, Boelle PY, Blondiaux E, Clement A, Ducou le Pointe H. HRCT and MRI of the lung in children with cystic fibrosis: comparison of different scoring systems. J Cyst Fibros. 2014;13(2):198–204. https://doi.org/10.1016/j.jcf.2013.09.003.
Ohno Y, Koyama H, Yoshikawa T, Matsumoto K, Takahashi M, van Cauteren M, et al. T2* measurements of 3-T MRI with ultrashort TEs: capabilities of pulmonary function assessment and clinical stage classification in smokers. AJR Am J Roentgenol. 2011;197(2):W279–85. https://doi.org/10.2214/AJR.10.5350.
Altes TA, Johnson M, Fidler M, Botfield M, Tustison NJ, Leiva-Salinas C, et al. Use of hyperpolarized helium-3 MRI to assess response to ivacaftor treatment in patients with cystic fibrosis. J Cyst Fibros. 2017;16(2):267–74. https://doi.org/10.1016/j.jcf.2016.12.004.
Maglione M, Montella S, Mollica C, Carnovale V, Iacotucci P, de Gregorio F, et al. Lung structure and function similarities between primary ciliary dyskinesia and mild cystic fibrosis: a pilot study. Ital J Pediatr. 2017;43(1):34. https://doi.org/10.1186/s13052-017-0351-2.
Nyilas S, et al. Novel magnetic resonance technique for functional imaging of cystic fibrosis lung disease. Eur Respir J. 2017;50(6). https://doi.org/10.1183/13993003.01464-2017.
Wielputz MO, et al. Multicentre standardisation of chest MRI as radiation-free outcome measure of lung disease in young children with cystic fibrosis. J Cyst Fibros. 2018;17(4):518–27. https://doi.org/10.1016/j.jcf.2018.05.003.
Leutz-Schmidt P, Stahl M, Sommerburg O, Eichinger M, Puderbach MU, Schenk JP, et al. Non-contrast enhanced magnetic resonance imaging detects mosaic signal intensity in early cystic fibrosis lung disease. Eur J Radiol. 2018;101:178–83. https://doi.org/10.1016/j.ejrad.2018.02.023.
Pennati F, et al. Assessment of pulmonary structure-function relationships in young children and adolescents with cystic fibrosis by multivolume proton-MRI and CT. J Magn Reson Imaging. 2018;48(2):531–42. https://doi.org/10.1002/jmri.25978.
Stahl M, et al. Comparison of lung clearance index and magnetic resonance imaging for assessment of lung disease in children with cystic fibrosis. Am J Respir Crit Care Med. 2017;195(3):349–59. https://doi.org/10.1164/rccm.201604-0893OC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Ummul Afia Shammi and Robert P Thomen declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Bronchiectasis
Rights and permissions
About this article
Cite this article
Shammi, U.A., Thomen, R.P. Role of New Imaging Capabilities with MRI and CT in the Evaluation of Bronchiectasis. Curr Pulmonol Rep 8, 166–176 (2019). https://doi.org/10.1007/s13665-019-00240-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13665-019-00240-z