Abstract
Neonatal seizures are a common neurologic emergency for which therapies have not significantly changed in decades. Improvements in diagnosis and pathophysiologic understanding of the distinct features of acute symptomatic seizures and neonatal-onset epilepsies present exceptional opportunities for development of precision therapies with potential to improve outcomes. Herein, we discuss the pathophysiology of neonatal seizures and review the evidence for currently available treatment. We present emerging therapies in clinical and preclinical development for the treatment of acute symptomatic neonatal seizures. Lastly, we discuss the role of precision therapies for genetic neonatal-onset epilepsies and address barriers and goals for develo** new therapies for clinical care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neonatal seizures are a common emergency with an incidence up to 0.95 to 2.8 per 1000 live births [1,2,3]. The reported incidence of seizures in preterm infants varies with the method of ascertainment, although in population-based and unselected cohorts incidence is estimated to be as high as 5% [4]. The most common causes of neonatal seizures—hypoxic–ischemic encephalopathy, stroke, and intracranial hemorrhage—are similar for both term and preterm infants [5]. Less common etiologies of neonatal seizures include infection, electrolyte disturbances (e.g., hypoglycemia or hypocalcemia), as well as metabolic causes. Therefore, most neonatal seizures are acute symptomatic seizures rather than a manifestation of neonatal-onset epilepsy [6].
The therapeutic approach to neonatal seizures can be tailored according to the key distinction between acute symptomatic seizures or neonatal-onset epilepsy. However, this distinction may not be clear at seizure onset and some neonates with epilepsy also have super-imposed acute brain injury [6]. Acute symptomatic seizures arise within the first week after an acquired brain injury and are usually self-limited in the neonatal period (though post-neonatal epilepsy can occur in up to ~ 20%) [7]. Neonatal-onset epilepsies are often secondary to underlying genetic or metabolic disorders; methods to assist with early diagnosis and potential for precision therapy will be discussed.
Key challenges surround the incomplete efficacy of antiseizure medications for neonatal seizures; despite standard treatments, more than half of neonates experience continued seizures after initial loading doses of antiseizure medications [8, 9]. This is likely, in part, due to immature neonatal neurophysiology which leads to excess excitation and reduced inhibition. Compared to mature adult neurons, intracellular chloride concentration is about 20–40 mM higher in immature neonatal neurons, a difference which is sufficient to shift the action of gamma-aminobutyric acid (GABA) from inhibition to excitation [10]. In mature neurons, activation of GABAA receptors by binding of GABA causes an influx of chloride; this results in neuronal membrane hyperpolarization and inhibition of action potentials. In immature neurons, GABAA receptor activation leads to an efflux of chloride, which effectively increases the likelihood of firing an action potential. Reversal of this chloride gradient is mediated by the expression of the sodium–potassium-chloride cotransporter 1 (NKCC1), which imports chloride, and the potassium-chloride cotransporter 2 (KCC2), which exports chloride [11, 12]. In the immature brain, expression of NKCC1 is higher than KCC2 which leads to the relatively high intracellular chloride concentration in immature neurons. This results in chloride efflux and cell depolarization when GABA binds to the post-synaptic receptor [11] and triggers inward calcium currents and the removal of the voltage-dependent magnesium block from the N-methyl-D-aspartate (NMDA) receptors. The net effect is promotion of calcium entry and activation of second messengers that increase brain excitability and seizure risk [13, 14]. Recurrent seizures further increase the intracellular chloride concentration, resulting in a more depolarized reversal potential of GABA [15]. Additional developmentally related expression changes in excitatory receptors that allow the brain to form appropriate activity-dependent developmental processes also leave the immature brain susceptible to hyperexcitability and seizures [13, 14, 16, 17].
Yet, despite these differences in neonatal physiology as compared to adults, current treatment practices include first-line antiseizure medications that act through the GABAA receptor (i.e., phenobarbital and benzodiazepines), which offers a potential explanation for the high risk of incomplete treatment response. However, prescription of other antiseizure medications, including fosphenytoin or levetiracetam, has not yielded superior results. Below, we discuss in detail the data for each of the current available medications, as well as emerging treatment options for neonatal seizures (Fig. 1).
Graphic illustration of sites of action for the currently available antiseizure medications used for neonatal seizures (black text, blue boxes) and therapeutics in preclinical development (red italics text, pink boxes). Note that in the neonatal brain, chloride efflux through GABAA receptors (black arrow) predominates due to the chloride gradient created from relative greater expression of NKCC1 versus KCC2. In the adult brain, this chloride gradient is reversed, allowing for chloride influx (red arrow) through the GABAA receptor. The TrkB pathway is activated following ischemia, leading to hypofunction of the KCC2 channel. Treatment with TrkB pathway modulators have been shown to improve KCC2 function in preclinical models of neonatal hypoxic–ischemic injury and reverse seizure refractoriness to phenobarbital, suggesting a future role as adjunctive therapy for refractory acute symptomatic seizures in neonates. Figure created with BioRender.com
Evaluating Data and Clinical Trial Design
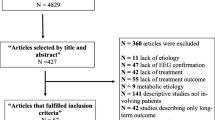
The available data to guide medication selection for the treatment of neonatal seizures are limited in quality and consist primarily of retrospective studies, with very few prospective trials. These study designs are limited by inability to adequately control for confounding variables (e.g., disease severity, medication exposure, time to treatment). This is, in part, due to variability in seizure identification—some studies assess clinical seizures only and others require amplitude-integrated EEG or conventional video-EEG monitoring. Conventional video-EEG monitoring is the gold standard for neonatal seizure identification [18] and is essential for trials of treatment efficacy given high rates of subclinical (electrographic only) seizures in neonates. Assessment of medication response has also varied. Some studies target complete seizure cessation, while others report percent seizure reduction or response within 1 h, etc. This variability reduces the opportunity to compare results across studies. Lastly, long-term developmental outcome measures are commonly not assessed, despite the critical importance of this information to families and clinicians [19,20,21]. There are a handful of randomized, controlled clinical trials in the treatment of neonatal seizures, but some of these same challenges are still apparent. For example, in the landmark study by Painter et al., comparing phenobarbital to phenytoin, continuous video-EEG monitoring was not used throughout the screening period [9]. Expert and key stakeholder recommendations are available to assist in neonatal clinical trial design and address the above limitations with specific solutions for each clinical trial phase. These recommendations are an important contribution to improve the quality of clinical trials in neonatal seizures[22]. A brief overview of proposed solutions to the limitations of current neonatal seizure treatment studies are shown in Table 1.
Treatment of Acute Symptomatic Seizures
Phenobarbital
Phenobarbital is strongly recommended by the World Health Organization for the first-line treatment of neonatal seizures and is the standard of care at most institutions, although there are limited randomized controlled trials to support this distinction [23]. Use of phenobarbital for neonatal seizures has been very consistent for decades and across geographical regions. Review of American hospital data from the Pediatric Health Information System revealed that 97% of neonates treated for seizures received phenobarbital and this practice has been very consistent over time [24,25,26,27]. When antiseizure medications are prescribed to neonates at hospital discharge, phenobarbital is also the most commonly prescribed medication [27, 28]. These data highlight the importance of phenobarbital in current treatment paradigms of neonatal seizures.
Phenobarbital exerts its effect as an allosteric modulator of the GABAA receptor. Yet, activation of the GABAA receptor in neonatal neurons results in excitation, instead of the typical inhibitory effect in adult models [29, 30]. These maturational differences in the newborn are hypothesized to underlie the reduced rates of response to phenobarbital as compared to older children and adults with seizures.
The landmark study by Painter et al. was a randomized controlled trial that directly compared phenobarbital to phenytoin as first-line treatment for neonatal seizures [9]. Complete seizure resolution occurred in 43% of infants randomized to receive phenobarbital, with an 80% reduction of seizures in 80% of neonates. More recently, a randomized controlled trial evaluated neonates treated with phenobarbital versus levetiracetam as first-line therapy after new-onset conventional EEG-confirmed seizures (NEOLEV2; NCT01720667) [31]. This study demonstrated seizure freedom at 24 h in 70% of patients treated with a single 20 mg/kg dose of phenobarbital. Notably, this phenobarbital response rate was higher than in the prior randomized controlled trial by Painter et al. [9]. There are differences in the study design between the two trials that could, in part, explain the higher response rate in the NEOLEV2 study. These include variability in EEG monitoring protocols and use of therapeutic hypothermia for infants with hypoxic-ischemic encephalopathy in NEOLEV2. Additionally, time to treatment was not reported in either study. This variable is important due to the natural temporal evolution of acute symptomatic neonatal seizures [32]. Despite differences in these two randomized controlled trials, the phenobarbital response rate in the NEOLEV2 study is encouraging. There remain concerns regarding the side effects of sedation, respiratory suppression, and hypotension [31]. Yet, these can easily be managed in the intensive care unit environment.
The potential negative long-term effects of phenobarbital on the develo** brain continue to be a discussion point in clinical practice and research. This concern is supported in non-injured animal models in which exposure to phenobarbital resulted in apoptosis of neurons in the cortex, white matter, and limbic system, as well as disruption of inhibitory synaptic development in hippocampal neurons [33,34,35,36]. These changes may explain the observed anxiety, behavioral, and cognitive changes in rodent models after exposure to phenobarbital [37, 38]. Additionally, it is proposed that damage to GABAA receptor neurons results in an enhanced excitatory network later in life [33].
However, there has also been suggestion of a neuroprotective effect of phenobarbital. In a mouse model of hypoxia induced seizures, treatment with phenobarbital (compared with saline placebo) resulted in less hippocampal neuronal death after a second-hit and later life exposure to kainic acid [37]. In this study, there were similar rates of neuronal cell death between the control group of uninjured mice without phenobarbital exposure and the phenobarbital exposed groups (group 1—hypoxia-induced seizure model exposed to phenobarbital and group 2—uninjured mice with phenobarbital exposure), although this was not controlled for the initial response to phenobarbital or seizure burden [37]. Furthermore, there was a clinical trial to evaluate for a potential preventative neuroprotective effect of phenobarbital in newborns with hypoxic–ischemic encephalopathy [39]. It was determined that early treatment with phenobarbital, prior to seizure onset, did reduce incidence of seizures but was not associated with a change in mortality or neurological outcome at hospital discharge. Long-term outcome measures were not assessed. Overall, the data support concerns for a negative effect of phenobarbital on the immature brain and a Cochrane Review concluded that prophylactic exposure in infants at risk for seizures is not recommended [40]. Importantly, the negative effect of untreated neonatal seizures is considered more clinically meaningful than the potential adverse effects of phenobarbital. Thus, phenobarbital remains the first-line standard of care treatment option for neonatal seizures. Yet, the above concerns highlight the urgent need for novel therapeutic options.
Fosphenytoin and Phenytoin
Fosphenytoin is used in up to 15% of patients with neonatal seizures [25, 26] but is typically prescribed when seizure control is inadequate after initial treatment with phenobarbital. Fosphenytoin is a phosphorylated prodrug of phenytoin and has the advantage of less cardiac toxicity and fewer local extravasation effects as compared to phenytoin, although both require careful consideration of drug interactions. The reduced risk of local skin reactions with fosphenytoin is due to the lower pH of 8.6 (compared to phenytoin pH of 11) and absence of propylene glycol. Additionally, compared to phenytoin, fosphenytoin is more likely to be compatible with other co-administered medications or infusions in an intravenous line.
Fosphenytoin is converted to phenytoin, the active metabolite, and then acts to stabilize the neuronal membrane by altering sodium currents. There was initial concern that parenteral fosphenytoin administration may result in reduced serum levels of free phenytoin, as early studies of pharmacokinetics were in older children and adults. However, additional studies that included neonates demonstrated adequate levels of free phenytoin serum concentration after loading doses of fosphenytoin and similar times to conversion to phenytoin as adult patients[41, 42]. Despite this, an additional challenge remains with enteral administration of phenytoin due to inconsistent (often limited) absorption and variability in serum free phenytoin levels [48]. However, a long-term follow-up study demonstrated that newborns who received initial treatment with fosphenytoin were more likely to have normal or only mild developmental delay at 18–24 months, compared with newborns treated with phenobarbital [44]. This study was limited by the retrospective design and relatively small samples size in the fosphenytoin group (n = 23 in fosphenytoin group; n = 80 in phenobarbital group) but may suggest an alternative to the potential negative effects of phenobarbital on the develo** brain.
Levetiracetam
Levetiracetam acts through the synaptic vesicle glycoprotein 2A (SV2A), which is a protein involved in the release of neurotransmitters, although the exact mechanism is not known. Levetiracetam is used less commonly than phenobarbital for the initial treatment of neonatal seizures. Over the past decade, use of levetiracetam increased from < 10% of all neonates with seizures to nearly 40%, surpassing the use of fosphenytoin/phenytoin [26, 28]. Recent interest in levetiracetam is likely multifactorial and includes its availability for parenteral administration, relative safety profile, minimal drug interactions, likelihood of less adverse effects than phenobarbital on the newborn brain, and improved efficacy compared to phenobarbital in infantile epilepsy [49].
Initial single-center, retrospective studies of levetiracetam reported efficacy in both term and preterm infants with a complete seizure cessation widely ranging between 26 and 86% of patients [50,51,52,53,54]. However, these studies were limited by primarily retrospective study designs, lack of a control group, and variable outcomes measures, as discussed previously. Yet, these numerous preliminary studies provided encouraging initial data and rationale for the NEOLEV2 study, a randomized controlled phase IIb efficacy, dose-escalation study of first-line treatment with levetiracetam compared to treatment with phenobarbital. Seizure cessation for 24 h occurred in significantly more patients treated with phenobarbital compared to levetiracetam (80% vs 28%, p < 0.001) [31]. After dose escalation, with an additional 20 mg/kg of levetiracetam (total dose 60 mg/kg), the seizure freedom rate at 24 h increased to 35%. Despite some efficacy demonstrated by levetiracetam, this study provides strong evidence of the superiority of phenobarbital as a first-line antiseizure medication and lack of seizure control with up to 60 mg/kg in loading doses of levetiracetam as first-line treatment for neonatal seizures. Although not powered to evaluate levetiracetam as a second-line antiseizure medication for neonatal seizures, it is notable that none of the neonates with seizures refractory to two loading doses of phenobarbital responded to levetiracetam. Thus, the NEOLEV2 study provides quite conclusive data that the secular trend of prescribing levetiracetam for neonatal seizures is not justified. As a result, phenobarbital remains the first-line standard of care.
Animal studies have not clearly demonstrated neuronal apoptosis with average doses of levetiracetam, although there is a possible dose-dependent effect with neuronal apoptosis after exposure to high doses (70 mg/kg) of levetiracetam as compared to low doses (7 mg/kg) in a neonatal hypoxia mouse model [55]. However, long-term outcomes of high-dose levetiracetam exposure were not evaluated. Short-term follow-up studies have reported improved tone and posture among infants treated with levetiracetam compared with neonates treated with phenobarbital [56], although preliminary data suggest long-term neurodevelopmental outcomes appear similar [57].
Treatment of Status Epilepticus in Neonates
Guidelines from the American Clinical Neurophysiology Society define neonatal status epilepticus as seizure duration totaling > 50% of a 1-h epoch [58]. The causes of neonatal status epilepticus are comparable to neonatal seizures in general, with hypoxic–ischemic encephalopathy or intracranial hemorrhage most common. There are high rates of morbidity and mortality associated with neonatal status epilepticus, with death occurring in up to half of preterm neonates [59].
Benzodiazepines
Benzodiazepines are first-line treatment for pediatric status epilepticus, but there are limited data to guide their use in neonatal status epilepticus. Benzodiazepines exert effect through the GABAA receptors as allosteric agonists, with the same challenges related to the maturational pattern in the newborn brain as phenobarbital. Additionally, similar to phenobarbital, animal models demonstrate that midazolam may increase status epilepticus-associated neuronal injury with no increase in animal survival [36, 60].
Available data regarding the use of benzodiazepines in neonates for seizures are primarily limited to retrospective studies. The response rate is varied with complete seizure response occurring in < 20% of neonates treated with 0.1 mg/kg midazolam as first-line treatment [61] and between 0 and 100% when midazolam or clonazepam are used as second-line treatment for ongoing seizures [62,63,64]. Nearly half of the neonates treated with midazolam as first-line treatment had continued seizures [61]; given the limitations in study design this number may, in fact, be higher.
In clinical studies, hypotension was the most frequently reported adverse event, and occurred in nearly 10% of infants, although transient hypoxia, apnea, decreased urinary output, and tachycardia also can occur [61, 64]. Additionally, in very preterm neonates (24–32 weeks gestation) exposure to midazolam was found to be inversely associated with hippocampal volume and cognitive outcomes [65]. The inconsistent response to benzodiazepines in neonates, as well as the potential additive neurotoxic effect on the newborn brain, highlights the need for alternative treatment options for neonatal status epilepticus.
Lidocaine
Lidocaine is commonly used as a local anesthetic but has been employed for second and third-line treatment of neonatal seizures [26]. It is also an anti-arrhythmia drug and has a narrow therapeutic window. Additionally, lidocaine is metabolized in the liver by the cytochrome p450 system, which can be influenced by gestational age and therapeutic hypothermia; however, this can be mitigated with the proposed dosing regimens available for preterm and term neonates [66,67,68].
Retrospective and small clinical studies demonstrate efficacy of lidocaine in neonates for whom phenobarbital failed to control seizures. The response rate to lidocaine infusions has been reported to be approximately 50–70% [63, 64, 69]. However, in the largest retrospective study (n = 413) only approximately 20% of infants had a sustained response and did not require additional antiseizure medications after second line treatment with lidocaine infusion[69]. Additionally, data suggest lidocaine may be more effective in term than preterm infants [69].
Large retrospective studies have identified cardiac arrhythmias in up to 4.8% of neonates during infusion with lidocaine [70], although with a reduced dosing regimen this number decreased to < 1% [71]. This highlights the importance of continuous cardiac monitoring during treatment with lidocaine. Future well-designed studies would be beneficial to define the role of lidocaine in the treatment of neonatal seizures. Until such data become available, we suggest consideration of lidocaine for neonates with status epilepticus despite loading doses of ≥ 40 mg/kg of phenobarbital. Note that exposure to fosphenytoin/phenytoin and presence of congenital heart disease are contraindications due to the risk of arrhythmia. Additionally, the clinical team must have a plan for subsequent treatment after the 48 h of lidocaine are completed.
Duration of Treatment with Antiseizure Medication
It is important to also consider the duration of treatment with either current or emerging therapeutics for neonatal seizures in order to reduce any potential risk of treatment on the immature neonatal brain. Neonatal seizures are predominantly acute symptomatic seizures and the highest seizure burden is typically in the first 24 h after onset [32]. Seizures usually resolve within several days, but up to 20% go on to develop post-neonatal epilepsy [137, 138]. The incidence of post-neonatal epilepsy and of abnormal neurodevelopmental outcomes does not appear to be reduced by longer duration of treatment with antiseizure medications [137, 139]. A recent prospective, multicenter comparative effectiveness study by the Neonatal Seizure Registry confirmed that discontinuation of antiseizure medication after resolution of acute symptomatic seizures and prior to hospital discharge does not alter future epilepsy risk, rates of cerebral palsy, or 2-year neurodevelopmental outcome [140].
The World Health Organization (WHO) recommends discontinuation of antiseizure medication in neonates with a normal neurological exam and/or normal EEG after at least 72 h of seizure freedom [23]. This recommendation is intended for neonates with acute symptomatic seizures, and not for infants with neonatal-onset epilepsy. However, in neonates with acute symptomatic seizures, there remains significant variability in how long antiseizure medications are continued, with medications often maintained after hospital discharge at most centers [27]. A longer duration of seizures in the neonatal period, abnormal MRI brain, and some seizure etiologies are risk factors for longer duration of treatment [27, 138, 141]. It is also known that the hospital site influences duration of treatment, as well as availability of a neonatal neurocritical care service [27, 142]. This highlights the importance of institutional efforts to standardize the identification and treatment of neonatal seizures and reduce unnecessarily prolonged exposure to antiseizure medication. Most neonates with acute symptomatic neonatal seizures do not require continued medication after hospital discharge. Conversely, infants with neonatal-onset epilepsy usually do require long-term treatment.
Emerging Treatment Options
Bumetanide
Bumetanide is a loop diuretic that blocks the Na–K-Cl co-transporter. Early animal models suggested a potential benefit when combined with phenobarbital for treatment of neonatal seizures [72], although this was not a completely consistent result and it has not been replicated in all rodent models of birth asphyxia [73]. Additionally, there is concern regarding the ability of bumetanide to cross the blood–brain barrier and reach intended targets [74].
In an initial open-label, dose escalation, feasibility study (NEMO trial; NCT01434225) of bumetanide administered with a second dose of phenobarbital as second-line therapy after phenobarbital failure (N = 14), the primary seizure efficacy endpoint (80% seizure reduction) occurred in less than half the cohort [75]. However, 5 of the neonates did not have seizures in the baseline period. It has been argued that if these neonates were excluded from efficacy analysis, then 5/9 neonates demonstrated a > 80 seizure reduction and reached the primary clinical efficacy endpoint of a > 50% response rate [76]. Additionally, 3 of the 14 neonates demonstrated hearing loss, although co-treatment with aminoglycoside was common and there was no control group to compare the rate of hearing loss in neonates who received standard treatment without bumetanide. The study was ended early due to insufficient efficacy and concern about the potential increased prevalence of hearing loss. Subsequently, a randomized, double-blind, dose-escalation trial (NCT00830531) designed to assess the safety and pharmacokinetics of bumetanide did not show a significant difference in hearing impairment between control (phenobarbital alone) and bumetanide treated groups [77].
In the randomized control trial, neonates (postmenstrual age 34–44 weeks) with persistent seizures despite initial loading doses of 20–40 mg/kg phenobarbital were randomized to subsequent treatment with either bumetanide plus a 5–10 mg/kg phenobarbital dose or phenobarbital 5–10 mg/kg alone (with saline as a control). There was a statistically significant reduction in seizure burden with escalating doses of bumetanide (0.1, 0.2, or 0.3 mg/kg) compared to the control group; however, the interpretation was complicated as seizure severity was unexpectedly not randomly distributed across groups. Yet, it appeared that infants with high seizure burden had more than expected reduction in seizures after bumetanide. Importantly, this was a pilot safety trial not intended to assess primary efficacy outcomes. However, this study revealed important initial data regarding tolerated bumetanide doses and safety data for future trials design.
Topiramate
Topiramate has multiple mechanisms of action, including glutamate-receptor inhibition and blockade of Na + channels, high-voltage Ca + currents, and carbonic anhydrase isoenzymes. These characteristics have raised the potential of a neuroprotective effect of topiramate through reduction of excitatory pathways. This has been supported by both in vitro and in vivo clinical studies, including models in the newborn such as periventricular leukomalacia models [78]. There is also report of increased safety in animal models as compared to phenobarbital or benzodiazepines, as well neuronal apoptosis only with doses significantly higher than currently used treatment doses [79, 80]. Two randomized clinical trials of topiramate initiation at the start of therapeutic hypothermia compared to hypothermia alone revealed a decrease in seizure burden and need for less antiseizure medications in the first 24 h, although the latter was not assessed for significance [81]. There was no significant effect on mortality or neurological disability [81, 82]. While the rate of post-neonatal epilepsy was lower among neonates treated with topiramate plus hypothermia compared to hypothermia alone, this was not statistically significant (14.3% vs 30.4%, P = 0.21) [82]. The first study by Filippi et al. included 21 neonates in the topiramate group, while the subsequent study by Nunez-Ramiro et al. was slightly larger with 57 neonates in the topiramate group [81, 82]. These relatively small sample sizes are a limiting factor and future studies are warranted, especially as no adverse events were attributed to topiramate administration. There is an ongoing clinical trial of topiramate in newborns with hypoxic–ischemic encephalopathy treated with therapeutic hypothermia that is currently recruiting participants (NCT01765218) with an expected completion date of May 2022.
There are few data regarding topiramate for the acute treatment of seizures in neonates. Its use is, in large part, limited by absence of an intravenous formulation. In a recent large multi-center review of practice variation in treatment of neonatal seizures, topiramate was used < 1% of the time; however, the paper did not specify whether topiramate was prescribed for acute symptomatic seizures or neonatal epilepsy [26]. A retrospective case series of neonates treated with topiramate suggests tolerability and safety, as well as efficacy in some patients [83], but larger prospective studies are needed.
Brivaracetam
Brivaracetam is a n-propyl analogue of levetiracetam designed with high affinity for the synaptic vesicle protein 2A (SV2A), a glycoprotein present in the membranes of synaptic vesicles. Brivaracetam is well tolerated in the setting of renal impairment, has minimal interactions with other medications, and is available in intravenous formulation. Like levetiracetam, the precise mechanism of this medication is not known, and these drugs may each act differently on the SV2A protein. Animal studies suggest that there may be developmental differences in SV2A with reduced expression in newborn models, although antiseizure properties of brivaracetam are demonstrated in these models [84]. There are limited clinical data regarding brivaracetam in the newborn period, although this medication has been well-tolerated in pediatric studies with side effects of mild somnolence, psychosis/behavior changes, and stomach upset/decreased appetite [85,86,87]. There is an active, open-label, single-arm study to evaluate the pharmacokinetics, efficacy, and safety of brivaracetam in neonates with repeated electroencephalographic seizures despite initial antiseizure medication (NCT03325439). The expected completion date is January 2022.
Lacosamide
Lacosamide is a sodium-channel blocking agent with a novel mechanism through slow inactivation of voltage-gated sodium channels. It was introduced for adult epilepsy treatment in 2008 and studies report its use in pediatric epilepsy management with limited side effects even with intravenous administration [88]. Due to its action on the sodium channel, there can be associated PR interval prolongation, although this has rarely occurred with intravenous administration in children.
There was a potential neuroprotective effect of lacosamide demonstrated in animal models of traumatic brain injury and status epilepticus [89, 90]. A model of neonatal arterial ischemic infarction revealed reduced areas of ischemia after pretreatment with oral lacosamide, although there was a dose-dependent response with higher rates of toxicity and mortality seen with dose escalation [91]. It remains unclear whether there is a neuroprotective effect in the newborn brain, or any associated neuronal apoptosis associated with exposure.
There are limited data available regarding the use of lacosamide in the neonatal period. Studies aimed at characterizing the pharmacokinetics in term and preterm neonates are important to help guide clinical use. Review of the literature demonstrates two patients who received lacosamide at age 1 month with no adverse events reported [92, 93]. There is a planned, multi-center, open label randomized active comparator study to evaluate the efficacy, safety, and pharmacokinetics of lacosamide in neonates with repeated electroencephalographic neonatal seizures (NCT04519645).
Ketamine
Ketamine is a non-competitive N-methyl-D-aspartate (NMDA) receptor antagonist that crosses the blood–brain barrier and is clinically used as a dissociative anesthetic. During refractory status epilepticus there is loss of GABA receptor inhibition as GABA receptors internalize and the concentration of NMDA receptors increases [94, 95]. This loss of GABA inhibition and activation of NMDA receptors can further propagate seizure activity and contribute to self-sustained status epilepticus [96]. In animal models, treatment with ketamine can be used to halt this response and resolve self-sustaining refractory status epilepticus [96, 97].
In a rat model of perinatal brain injury, exposure to ketamine resulted in a partial neuroprotective response with reduced energy requirements and restored levels of ATP compared to controls [98]. However, additional in vivo animal studies suggest neuronal apoptosis with ketamine exposure and reduced cognitive testing outcomes in follow-up studies, although the exact dose and vulnerable ages are not known [99, 100].
Ketamine is also used as an analgesic. Data derived from its use in the delivery room of preterm infants at the time of intubation revealed no difference in neurological outcomes at age 2 years compared with controls [101]. There may be a ketamine dosing threshold and duration of treatment necessary for negative effect and neuronal apoptosis.
The use of ketamine for treatment of neonatal seizures is primarily based on case reports with little information regarding dosing, safety, or efficacy [102, 103]. There are more extensive data regarding the use of ketamine in children and adults, although there are no randomized controlled trials of this agent. A review of ketamine for the treatment of status epilepticus in children suggested an overall response rate of 73% in children and only rare adverse effects [104]. These encouraging data highlight the importance of future studies to further evaluate ketamine for the treatment of recurrent neonatal seizures and status epilepticus.
Preclinical Studies
Given the unique pathophysiology of neonatal seizures [14], identification of potential treatments of neonatal seizures cannot rely solely on extrapolation of antiseizure medication data from older children and adults. Animal models in various species have been developed to mimic the consequences of neonatal hypoxic-ischemic injury (reviewed in [105]). However, the majority of hypoxia-related seizure models are performed with rodents. In rats, hypoxic seizures are induced only during the critical developmental window between post-natal day (P) 6–12, which roughly corresponds to term brain development in humans [106,107,108]. Neonatal mice have been used at the P7-9, during the maximal transition in synaptic receptor maturation, similar to term human brain development [106].
In the hypoxia model, acute seizures are induced with exposure to varying degrees of global hypoxia for varying durations. Several models display spontaneous recurrent seizures, without significant neuronal death, following the acute insult [106]. In contrast, hypoxia–ischemia models consist of unilateral ligation of the common carotid artery in addition to a period of hypoxia exposure. This provides a more severe insult and produces more substantial tissue damage in addition to more severe recurrent seizures in the long-term compared with the hypoxia model [106, 109]. This results in the recapitulation of many of the features seen in human neonatal brain injury, including tissue pathology, cognitive/behavioral deficits, and seizures during and after the insult [106, 110]. In addition, chemoconvulsant seizures have been induced with kainic acid or flurothyl to assess efficacy of various antiseizure medications in neonatal rodents [111, 112].
Chemoconvulsant modeling is technically easier to perform than current hypoxic-ischemic models, with consistent elicitation of seizures by exposure to the chemoconvulsant agent. This approach may allow for relatively high-throughput screening of candidate anti-seizure compounds, while providing insight into mechanisms required for appropriate treatment of neonatal seizures. However, care should be taken in interpretation of results derived from this appraoch, as these models do not recapitulate the same complex cascade of cellular and molecular mechanisms that lead to hypoxic-ischemic seizures in neonates; candidate drug efficacy should also be examined in more physiologically relevant models of hypoxic–ischemic injury.
Potassium-Channel Openers
Compared with the mature brain, GABAergic inhibition is decreased in the neonatal brain. Given this, potassium channels play a unique role in controlling excitability during early development, as discussed above [11, 12] and likely relate to the development and subsequent resolution of KCNQ2/3 related self-limited familial neonatal epilepsies [113]. This suggests that use of potassium channel openers may be an effective approach to enhance inhibition and treat neonatal seizures.
Flupiritine has been approved in Europe for decades as a non-opioid analgesic. It has been shown to activate G-protein regulated inward rectifying K + (GIRK) channels, which may indirectly inhibit NMDA receptor activity. Activation of GIRK channels leads to hyperpolarization of the neuronal membrane, with resulting stabilization of the resting neuronal membrane [114]. A series of eloquent experiments by Raol and colleagues examined the effects of flupiritine in several models of neonatal seizures. They initially reported flupiritine to be more efficacious in preventing and stop** chemoconvulsant induced seizures than phenobarbital or diazepam in neonatal rats [115]. They later showed efficacy in treating seizures in a hypoxia model [116] and hypoxia–ischemia model [117] of neonatal seizures in rats. In follow-up studies, they also reported that flupiritine treatment reduced injury induced volume loss and partially reversed learning and memory impairments [118]. Unfortunately, the withdrawal of flupiritine from the European market was recommended in 2018 due to the risk of liver injury with prolonged use [119].
Retigabine/ezogabine is chemically similar to flupiritine and also showed antiseizure effects in limited preclinical models of chemoconvulsant induced seizures in neonatal rats [120]. Ezogabine was previously FDA approved as an adjunctive treatment for focal seizures, though it was withdrawn from clinical use in 2017 due to skin and eye abnormalities. Prior to withdrawal, ezogabine was explored as a potential precision therapy for KCNQ2 developmental and epileptic encephalopathy (KCNQ2-DEE), potentially showing some benefit in patients treated prior to age 6 months [121], though none of the patients received ezogabine treatment in the neonatal period. Targeting potassium channels in the acute neonatal period may be of future benefit in treating acute symptomatic neonatal seizures in addition to targeting specific genetic etiologies. A phase 3 clinical trial of a pediatric re-formulated ezogabine (XEN496) is expected in 2021 as an orphan drug specifically for KCNQ2-DEE (NCT04639310).
Tyrosine Receptor Kinase B Modulators
The age-dependent upregulation of the K + -Cl- co-transporter (KCC2) plays a role in the shift of GABAergic signaling from depolarizing to hyperpolarizing [11, 12] and thus contributes to pharmacoresistant seizures. Excitotoxic injury has been shown to phosphorylate tyrosine receptor kinase B (TrkB) pathway signaling [122]. Recent preclinical studies have sought to modulate KCC2 to improve the efficacy of GABAA agonists in neonatal seizures via antagonism of TrkB signaling. In a mouse model of phenobarbital-refractory postischemic seizures, the postischemic activation of the TrkB pathway resulted in the hypofunction of KCC2 [123]. This study utilized a carotid-ligation ischemic seizure model in which seizures were found to be refractory to phenobarbital at P7, but responsive to phenobarbital at P10, further under-scoring the age-dependent nature of neonatal seizure pathophysiology. Administration of a small-molecule TrkB antagonist, ANA12, reversed phenobarbital resistant seizures at P7 by preventing activation of the TrkB/phospholipase C, gamma 1 (PLCgamma1) pathway in a dose-dependent manner, though it showed no change in seizure rescue at P10 [123]. Significantly, treatment with ANA12 also led to long-term benefits in improving sleep dysfunction and activity-dependent markers of cognition [124]. Similar results were reported from follow-up studies utilizing a brain-derived neurotrophic factor (BDNF) memetic, LM22A-4, also prevented BDNF-mediated TrkB/PLCgamma1 pathway activation and KCC2 hypofunction [125]. Interestingly, the full TrkB agonists, HIOC, and deoxygedunin also significantly rescued the phenobarbital refractory phenotype and prevented postischemic degradation of KCC2 [125].
Taken together, these studies suggest that inhibition of cascades associated with endogenous BDNF/TrkB pathway activation may prevent the emergence of refractory neonatal seizures. Indeed, the role of TrkB activation in epileptogenesis was shown in a study utilizing the TrkB inhibitor, lestaurtinib (CEP-701), to reverse TrkB phosphorylation following hypoxia. This prevented seizure susceptibility to a “second hit” with a chemoconvulsant [126]. These studies provide promising evidence that targeting the TrkB pathway may be a successful strategy for prevention of refractory seizures in neonates and could lead to improved neurodevelopmental outcomes following hypoxic–ischemic injury.
Cannabinoid-Related Agents
Recent interest in cannabidiol as a novel antiseizure medication has led to further examination of the manipulation of the endogenous cannabinoid (endocannabinoid) system in the treatment of neonatal seizures. The endocannabinoid system is thought to modulate neuronal hyperexcitability in adult brains but targeting the cannabinoid system in develo** brains is still poorly understood.
A study designed to examine cannabinoid manipulation in chemoconvulsant and hypoxia-induced seizure models in P10 and P20 rats demonstrated that cannabinoid agonists WIN 55,212–2 (WIN) and arachidonyl-2′-chloroethylamide (ACEA) exerted anticonvulsant effects in a benzodiazepine inverse agonist model of clonic seizures utilizing the chemoconvulsant methyl-6,7-dimethoxy-4-ethyl-beta-carboline-3-carboxylate (DMCM). WIN also exhibited modest, but significant, antiseizure effects in PTZ- and acute hypoxia-induced seizures [127]. Conversely, CB1 receptor antagonism increased seizure severity.
Later studies examined treatment with cannabidivarin (CBDV), the propyl analog of cannabidiol (CBD). The effects of CBDV were age- and model-dependent, with little efficacy at P10, but significant antiseizure effects at P20 in the maximal electric shock model and DMCM-evoked seizures [128]. These results suggest that targeting of the endocannabinoid system for the treatment of neonatal seizures deserves further attention in pre-clinical studies, with additional focus on toxicity of manipulating the endocannabinoid system in the develo** brain, given the known deleterious neurodevelopmental effects of in utero cannabis exposure [129].
Other Agents
The unique physiology of the neonatal brain raises the possibility of targeting unique mechanisms to dampen hyperexcitability. The mechanisms of pharmacoresistant status epilepticus are poorly understood, but there is a need to explore mechanisms beyond regulating GABA or sodium channels, which are currently the first- and second-line approaches in managing neonatal status epilepticus [26, 27, 130]. A recent study in neonatal rats aimed to alter metabolism for seizure control, arguing that neuronal activity is highly energy-dependent and requires significant glucose metabolism [131]. The investigators aimed to utilize a glycolysis inhibitor, 2-deoxyglucose (2-DG) to compete with glucose for cell entry and inhibit glycolysis and neuronal ATP production. In the rat model of pilocarpine-induced neonatal status epilepticus, 2-DG was as effective at aborting status epilepticus as phenobarbital or levetiracetam [131]. Though this appears to be an intriguing target in the treatment of refractory status epilepticus, significant work needs to be done to ensure that these results translate to more physiologic models of hypoxic-ischemic induced refractory seizures and to examine adverse effects of systemic inhibition of glycolysis, even if administered only for a short time.
An additional recent study has implicated chloride channels, specifically the voltage-dependent CLC-3 Cl- channels as playing a significant role in neonatal seizures [132]. The investigators reported that CLC-3 Cl- channels mediated a large voltage-dependent outward rectifying Cl- current in neonatal, but not adult, mouse brains, and this current was blocked with the administration of sodium-gluconate in vitro. Intriguingly, this in vitro finding was translated to several in vivo models. Administration of sodium gluconate blocked kainic acid induced status epilepticus in neonatal, but not adult rats. Additionally, in the hypoxia–ischemia model of neonatal seizures, administration suppressed epileptiform bursts as well as phenobarbital and their effects were synergistic when co-administered [132]. These results are impressive and deserve further attention in the human condition, as gluconate is already FDA approved as a food additive. The authors noted that the gluconate concentrations needed to treat seizures were rather high and that brain penetration and side effects would need to be evaluated further.
Kainate and AMPA receptors may be additional targets for neonatal seizures, as they show peak brain expression during late embryonic and early postnatal periods [14]. Indeed, knocking out the GluK2 kainic acid receptor subunit or blocking kainic acid receptors by a novel drug, UBP310, blocked excitatory neurotransmission in vitro [133]. In vivo, GluK2 knockout mice and those treated with UBP310 were less susceptible to seizures during reoxygenation following hypoxia [133]. Given the importance of kainate receptor signaling on brain development, blocking kainic acid receptors may result in significant toxicity, which has not been fully assessed. The noncompetitive AMPA antagonist, talampanel, suppressed hypoxia-induced neonatal seizures and also prevented enhanced seizure susceptibility later in life [134]. Notably, treatment with talampanel did not result in any increase in cell death, suggesting that AMPA receptor antagonism may be a safe and effective target for hypoxia-induced neonatal seizures.
Lastly, bumepamine, a lipophilic benzylamine derivative of bumetanide has been considered for use in neonatal seizures in preclinical models. Bumepamine was first developed in 1978 by Nielsen and Feit [135]. It demonstrates 80% lower diuretic activity and lower ionization rate at physiological pH compared to bumetanide. Additionally, bumepamine has shown a more potent dose dependent effect as compared to bumetanide in potentiating the effect of phenobarbital in animal models of chronic epilepsy, although the mechanism of this effect is not fully understood [136]. These factors have prompted interest in this compound as a treatment for neonatal seizures. However, data at this time are limited to animal models.
Neonatal-Onset Epilepsy
Though neonatal-onset epilepsies make up only 13% of patients with neonatal seizures in the neonatal intensive care unit [6], the early identification of epilepsy rather than acute symptomatic seizures can have significant consequences for guidance of management and informing prognosis in these cases. As rapid genetic testing becomes more widely available, our future ability to deliver precision medicine will provide opportunities to improving outcomes for children with neonatal-onset epilepsies. However, until such time that rapid genetic testing is standard of care, clinicians must be aware of clinical features that may indicate a genetic etiology that may be responsive to targeted treatment. Neonatal-onset epilepsies with a genetic etiology may be related to structural brain abnormalities, metabolic diseases, or other genetic syndromes [143]. Targeted therapies are available for some genetic etiologies of neonatal-onset epilepsy, with others in preclinical development (Table 2).
Structural Brain Abnormalities
Structural brain anomalies may be identified by in utero imaging or with early magnetic resonance imaging (MRI) during initial seizure work-up. A recent report of neonatal epilepsy found that ~ 29% of neonatal-onset epilepsies were related to congenital brain malformations [6]. Congenital malformations of brain development may be multifactorial, though multiple pathogenic genes and chromosomal anomalies have been implicated. Early imaging is essential to narrowing the differential diagnosis, as many of these malformations are due to genetic syndromes that may be associated with extracerebral congenital anomalies. Early consultation with a geneticist is recommended to ensure that the appropriate diagnostic tests are pursued [129]. Isolated structural malformations can lead to neonatal seizures due to focal or diffuse abnormalities in brain structure or neuronal migration, including agenesis of the corpus callosum (L1CAM, ZEB2, TUBA1, TUBB2A, etc.), polymicrogyria (ADGRG1, AKT2, MTOR, PTEN, etc.), lissencephaly (PAFAH1B1, TUBA1A, DCX, ARX, FKTN), schizencephaly (EMX2, SIX3, SHH, COL4A1), megalencephaly (MTOR, SHH, PIK3CA, LYK5/STRADA), holoprosencephaly (SHH, ZIC2, SIX3, TGIF1), and heterotopias (RELN, DCX, TUBBA1A, etc.) [144]. Though age of seizure onset can vary in patients with structural abnormalities, most with an early presentation of seizures have a disorder of neuronal migration [6]. Neonates with epilepsy due to brain malformations are more likely to die or to be discharged to hospice care than those with other genetic epileptic encephalopathies [6], underscoring the severity of their epilepsy and need for additional therapeutic interventions.
Targeted therapeutics in structurally related neonatal-onset epilepsies are limited. Though people with tuberous sclerosis complex rarely have seizures starting in the neonatal period, the ability to identify these infants as high-risk patients may allow for early intervention to prevent epileptogenesis. A recent study of infants with tuberous sclerosis complex (TSC1, TSC2) aimed to improve outcomes at 24 months by treating with vigabatrin prior to seizure onset, but after the first interictal discharges were detected, versus conventional treatment once seizures had developed [145]. Children in the early treatment group, compared with controls, had a later onset of epilepsy and a decreased incidence of infantile spasms and refractory epilepsy. Interestingly, there was no significant difference in developmental outcomes at 24 months of age, suggesting that developmental delays related to tuberous sclerosis complex may be somewhat independent from seizure severity [145]. However, this is contradictory to larger long-term studies that suggest that early onset and severe epilepsy in the first 2 years of life is associated with long-term intellectual disabilities in individuals with tuberous sclerosis complex [146]. Given this disconnect, longer-term evaluation of children who received early treatment with vigabatrin deserves evaluation, as the suppression of epileptogenesis with early treatment remains intriguing.
The mammalian target of rapamycin (mTOR) pathway includes several genes that may be related to early-onset structural epilepsies including DEPDC5, TSC1, TSC2, AKT3, and MTOR. The use of mTor inhibitors, such as everolimus and rapamycin, have shown limited success in the treatment of epilepsy in these disorders, though they have not been fully explored in the neonatal period or prior to seizure onset [147, 148]. Additionally, early evaluation for epilepsy surgery may be considered in patients with treatment-resistant focal seizures due to a structural etiology, even those with a genetic basis [149].
Metabolic Disorders
Though rare, it is important to recognize treatable metabolic neonatal epileptic encephalopathies (reviewed in [150]). Clinical features that may raise suspicion for an underlying metabolic disorder include an initial symptom-free period followed by feeding difficulty and lethargy, hypotonia, respiratory distress and abnormal laboratory test result including hypoglycemia, non-anion gap metabolic acidosis, ketosis, hyperammonemia, elevated lactate, and transaminitis [136, 137, 145]. Seizures in metabolic disorders may be either a primary manifestation or secondary to metabolic abnormalities and EEG may show a burst-suppression or hypsarrhythmia pattern [145]. Imaging may show evidence of severe injury without a clinical history to suggest an obvious hypoxic injury at birth [145]. Magnetic resonance spectrography (MRS) may be an essential tool in identifying suspected metabolic disorders [137].
Potentially treatable causes of metabolic neonatal-onset seizures include pyridoxine-dependent epilepsy, PNPO deficiency, nonketotic hyperglycinemia, organic acidurias, urea cycle disorders, peroxisomal disorders, folinic acid-responsive seizures, biotinidase deficiency, molybdenum cofactor deficiency, sulphite oxidase deficiency, and congenital disorders of glycosylation (reviewed in [144]). Even with appropriate treatments, responses are often varied; metabolic epileptic encephalopathies are frequently associated with poor outcomes. This underscores the need for early identification and the development of more precise and effective targeted therapies.
Preclinical and clinical studies of therapeutics for metabolic epileptic encephalopathies are limited. There are current clinical trials of cyclic pyranopterin monophosphate (cPNP) for the treatment of Molybdenum cofactor deficiency (NCT02629393) after treatment in an initial compassionate-use cohort showed safety and efficacy, most notably in the patients who were treated before the onset of recurrent seizures [151]. Preclinical studies are also examining the use of viral vectors to increase hepatic expression of molybdopterin synthase [152].
Current treatments of pyridoxine-dependent epilepsy have focused on pyridoxine supplementation, with some evidence supporting additional lysine restriction and arginine supplementation [153]. Emerging therapeutic strategies for pyridoxine-dependent epilepsy include ALDHA7A1 directed antisense therapy [154] and targeting of upstream lysine degradation pathways to prevent the build-up of toxic metabolites [153, 155]. Gene therapies for inherited neurometabolic diseases continue to be investigated as a means of precision therapy for these rare diseases. Importantly, immune tolerance to foreign proteins in the neonate may be an important factor in successful gene or protein replacement therapies, making early diagnosis essential for successful treatment [156, 157].
Genetic Neonatal Epilepsy Syndromes
Neonatal epilepsy syndromes often present in the first days to weeks of life. Clinical identification of a genetic neonatal epilepsy syndrome is useful to establish a diagnosis and etiology, understand the pathophysiology, guide treatment, estimate prognosis, and identify expected comorbidities [158]. Interestingly, neonatal-onset epilepsies have a broad range of phenotypic severity, with some self-limited and others severe and progressive, even though they may have common genetic loci. Monogenetic causes of neonatal-onset epilepsies have been reviewed extensively as our diagnostic testing and understanding of specific genetic disorders continue to expand [130, 144]. Yet, targeted therapeutic options remain inadequate and only clinically relevant to a few known disorders.
In a recent study of neonatal-onset epilepsies, autosomal dominant pathogenic variants in KCNQ2 were the most common finding on genetic testing [6]. KCNQ2 encodes a voltage-gated potassium channel (Kv7.2) responsible for dichotomous epilepsy syndromes. Self-limited familial neonatal epilepsy due to (often familial) pathogenic variants in KCNQ2 often presents in the first few days of life with focal tonic seizures, often with apnea, vocalizations, or autonomic changes [154]. Seizures are typically brief, but cluster and require treatment. Interictal EEG is normal. Seizures abate within the first year of life, though up to 15% of individuals may develop epilepsy later in life [159]. Conversely, KCNQ2 related neonatal encephalopathy presents with a much more severe phenotype. Patients present with early onset, often tonic seizures that are difficult to control, and have a severely abnormal interictal EEG that may display a burst suppression pattern or multifocal discharges. Seizure frequency tends to decrease over time, but children have poor developmental outcomes. Targeted therapy with the potassium channel opener, ezogabine, was potentially beneficial in treating refractory seizures in patients with KCNQ2 encephalopathy, especially in patients treated before 6 months of age, whereas patients treated at older ages showed a less robust response [121]. Unfortunately, ezogabine was discontinued by the manufacturer in 2017 due to skin discoloration and potential vision loss due to retinal pigmentation [160]. Interestingly, treatment with sodium channel blockers, such as carbamazepine or phenytoin, has been reported to be relatively effective in treating seizures in KCNQ2-DEE. In a recent study of children with KCNQ2-DEE, 53% were seizure free on carbamazepine and 33% responded the phenytoin [161]. It is unclear how sodium-channel blockers act in a potassium channel mutation, though the authors suggested that voltage-gated sodium channels co-localize with KCNQ potassium channels and that modulation of one channel may significantly affect the function of the channel complex [161].
Pathogenic variants in voltage-gated sodium channel subunits, including SCN1A and SCN2A, are associated with several neonatal-onset epilepsy syndromes. Loss-of-function mutations in SCN1A are most commonly implicated in Dravet syndrome with seizure onset in the first year of life. However, SCN1A is rarely implicated in epilepsy of infancy with migrating focal seizures (EIMFS) and early onset SCN1A-DEE with seizure onset in the neonatal period [162]. It is notable that in SCN1A-DEE, most patients have a recurrent de novo missense mutation, Thr226Met variant, which is proposed to create a dual-action, gain-of-function and loss-of-function phenotype, contrary to the loss-of-function phenotype most commonly seen in Dravet syndrome [163, 164]. This would suggest that children with SCN1A-DEE may have seizures responsive to sodium-channel blockers, even though these medications are contraindicated in SCN1A-associated Dravet syndrome. However, this has not been adequately supported in the limited published literature [163].
Pathogenic variants in SCN2A have been associated with self-limited familial or nonfamilial neonatal epilepsies as well as more severe developmental and epileptic encephalopathies with neonatal-onset, in addition to other neurologic disorders with onset beyond the neonatal period [165]. There is wide phenotypic variation associated with SCN2A pathogenic variants, though missense variants in epileptic encephalopathies are often activating, suggesting gain of function physiology [166]. As such, these children’s seizures often respond to sodium-channel blockers (e.g., phenytoin and carbamazepine [166]). Another recent case series showed response to lacosamide in two children with SCN2A associated infantile onset epilepsy after they had both shown an incomplete response to phenytoin [93].
The syndrome of epilepsy of infancy with migrating focal seizures (EIMFS) is most commonly associated with pathogenic variants in the KCNT1 gene, which encodes a subunit of a sodium-dependent potassium channel [167]. Seizures in EIMFS often begin in the neonatal period and are characterized by focal seizures that appear to migrate from one region to another on EEG. Seizures are often refractory to antiseizure medications and there is associated arrest of psychomotor development. Pathogenic variants in KCNT1 typically have a gain-of-function effect. Precision treatment with the potassium-channel blocker quinidine has been reported to be effective in controlling seizures in a small subset of patients with KCNT1 [168,169,170] although more recent, larger case series have reported mixed effects [171, 172]. Additional in vitro studies have been conducted with the KCNT1 current blocker, bepridil, showing more potent KCNT1 blockade than quinidine for two patient-associated KCNT1 variants, though it was not trialed in patients [173]. The authors suggested that bepridil may provide another agent for precision medicine in KCNT1 associated EIMFS, though it must be noted that functional evaluation of specific mutations should be considered prior to treatment with KCNT1-blocking agents [169, 173].
Conclusions
The treatment of neonatal seizures presents a unique challenge in pediatric neurology and neonatology due to the unique pathophysiologic features of the immature brain. Despite significant advances in preclinical research, current available therapeutics for acute symptomatic neonatal seizures have not changed substantially in decades. By contrast, the Food and Drug Administration (FDA) and European Medicines Agency (EMA) have approved greater than 20 new antiseizure medications for adults, none of which are approved for newborn infants [174]. The challenges in bringing new drug treatments to clinical trials for neonatal seizures are great. There are ethical considerations in balancing the risks and benefits in administering a new drug when safety and efficacy data from adults cannot be adequately extrapolated to neonates. Logistic considerations are even greater, as participants are recruited within hours to days following birth, with consent provided by parents who have likely also gone through a series of parallel medically and emotionally traumatic events. In addition, adequate EEG monitoring—with real-time interpretation—and ability to perform frequent blood monitoring is necessary to perform high quality trials. It is also recommended to include a control arm; either with current first-line therapy (i.e., phenobarbital) or to design trials that directly compare second-line treatment options for seizures that persist despite phenobarbital. These steps require close multidisciplinary collaboration.
Given these challenges, collaboration across multiple centers is essential for future trials. Rapid distinction between acute symptomatic seizures versus neonatal-onset epilepsy with early appropriate imaging, laboratory and genetic testing is crucial as we move toward precision medicine. Use of electronic health records and learning healthcare systems [175]—particularly for identification of children with rare neonatal-onset epilepsies or for long-term follow-up data—could allow study sites to maintain consistent data collection and lead to more robust interpretation of the gathered data. The learning healthcare system construct could also be applied for assessment of implementation of new trial results in real-world clinical practice.
The need for new treatments for neonatal seizures is evident. However, despite limited new antiseizure medications for neonatal seizures in the past, there is hope for the future. Emerging clinical trials and preclinical data are encouraging, as is the expanding genetic landscape and potential for precision therapy. Long-term developmental outcomes remain of paramount importance and our hope is that in the next decade we will have antiseizure medications that are not only more effective than our current treatment options for neonatal seizures, but also decrease the risk of neuronal injury in the develo** brain. The combination of these features will provide the best hope for the future of neonates with seizures.
References
Lanska MJ, Lanska DJ. Neonatal Seizures in the United States: Results of the National Hospital Discharge Survey, 1980-1991. Neuroepidemiology. 1996;15:117–125.
Saliba RM, Annegers JF, Waller DK, et al. Incidence of neonatal seizures in Harris County, Texas, 1992-1994. Am J Epidemiol. 1999;150:763–769.
Glass HC, Pham TN, Danielsen B, et al. Antenatal and Intrapartum Risk Factors for Seizures in Term Newborns: A Population-Based Study, California 1998-2002. J Pediatr. 2009;154:24-28.e1.
Lloyd RO, O’Toole JM, Pavlidis E, et al. Electrographic Seizures during the Early Postnatal Period in Preterm Infants. J Pediatr. 2017;187:18–25.e2.
Glass HC, Shellhaas RA, Wusthoff CJ, et al. Contemporary Profile of Seizures in Neonates: A Prospective Cohort Study. J Pediatr. 2016;174:98-103.e1.
Shellhaas RA, Wusthoff CJ, Tsuchida TN, et al. Profile of neonatal epilepsies. Neurology. 2017;89:893–899.
Uria-Avellanal C, Marlow N, Rennie JM. Outcome following neonatal seizures. Semin Fetal Neonatal Med. 2013;18:224–232.
Glass HC, Soul JS, Chu CJ, et al. Response to antiseizure medications in neonates with acute symptomatic seizures. Epilepsia. 2019;60:e20–e24.
Painter MJ, Scher MS, Stein AD, et al. Phenobarbital Compared with Phenytoin for the Treatment of Neonatal Seizures. N Engl J Med. 1999;341:485–489.
Yamada J, Okabe A, Toyoda H, et al. Cl- uptake promoting depolarizing GABA actions in immature rat neocortical neurones is mediated by NKCC1. J Physiol. 2004;557:829–841.
Dzhala VI, Talos DM, Sdrulla DA, et al. NKCC1 transporter facilitates seizures in the develo** brain. Nat Med. 2005;11:1205–1213.
Rivera C, Voipio J, Payne JA, et al. The K+/Cl− co-transporter KCC2 renders GABA hyperpolarizing during neuronal maturation. Nature. 1999;397:251–255.
Carrasco M, Stafstrom CE. How Early Can a Seizure Happen? Pathophysiological Considerations of Extremely Premature Infant Brain Development. Dev Neurosci. 2018;40:417–436.
Nardou R, Ferrari DC, Ben-Ari Y. Mechanisms and effects of seizures in the immature brain. Semin Fetal Neonatal Med. 2013;18:175–184.
Dzhala VI, Kuchibhotla KV., Glykys JC, et al. Progressive NKCC1-Dependent Neuronal Chloride Accumulation during Neonatal Seizures. J Neurosci. 2010;30:11745–11761.
Stafstrom CE, Thompson JL, Holmes GL. Kainic acid seizures in the develo** brain: status epilepticus and spontaneous recurrent seizures. Dev Brain Res. 1992;65:227–236.
Miller S, Goasdoue K, Björkman St. Neonatal seizures and disruption to neurotransmitter systems. Neural Regen Res. 2017;12:216-217.
Shellhaas RA, Chang T, Tsuchida T, et al. The American Clinical Neurophysiology Societyʼs Guideline on Continuous Electroencephalography Monitoring in Neonates. J Clin Neurophysiol. 2011;28:611–617.
Lemmon ME, Donohue PK, Parkinson C, et al. Communication Challenges in Neonatal Encephalopathy. Pediatrics [Internet]. 2016;138:e20161234. Available from: www.aappublications.org/news. Accessed January 1, 2021
Lemmon ME, Donohue PK, Parkinson C, et al. Parent Experience of Neonatal Encephalopathy. J Child Neurol. 2017;32(3):286–292.
Hill E, Glass HC, Kelley K, et al. Seizures and Antiseizure Medications are Important to Parents of Newborns With Seizures. Pediatr Neurol. 2017;67:40–44.
Soul JS, Pressler R, Allen M, et al. Recommendations for the design of therapeutic trials for neonatal seizures. Pediatr Res. 2019;85:943–954.
WHO Department of Mental Health and Substance Abuse, WHO Department of Maternal Newborn Child and Adolescent Health, OASI Department of Mental Retardation Unit of Neurology and Clinical Neurophysiopathology. Guidelines on neonatal seizures. [Internet]. World Health Organ. 2011. Available from: https://apps.who.int/iris/handle/10665/77756. Accessed November 30, 2020.
Blume HK, Garrison MM, Christakis DA. Neonatal seizures: Treatment and treatment variability in 31 United States pediatric hospitals. J Child Neurol. 2009;24:148–154.
Dizon MLV, Rao R, Hamrick SE, et al. Practice variation in anti-epileptic drug use for neonatal hypoxic-ischemic encephalopathy among regional NICUs. BMC Pediatr. 2019;19:67. Accessed November 30, 2021.
Ahmad KA, Desai SJ, Bennett MM, et al. Changing antiepileptic drug use for seizures in US neonatal intensive care units from 2005 to 2014. J Perinatol. 2017;37:296–300.
Shellhaas RA, Chang T, Wusthoff CJ, et al. Treatment Duration After Acute Symptomatic Seizures in Neonates: A Multicenter Cohort Study. J Pediatr. 2017;181:298-301.e1.
Le VT, Abdi HH, Sánchez PJ, et al. Neonatal Antiepileptic Medication Treatment Patterns: A Decade of Change. Am J Perinatol. 2021;38:469-476.
Ben-Ari Y, Cherubini E, Corradetti R, et al. Giant synaptic potentials in immature rat CA3 hippocampal neurones. J Physiol. 1989;416:303–325.
Cherubini E, Rovira C, Gaiarsa JL, et al. GABA mediated excitation in immature rat CA3 hippocampal neurons. Int J Dev Neurosci. 1990;8:481–490.
Sharpe C, Reiner GE, Davis SL, et al. Levetiracetam Versus Phenobarbital for Neonatal Seizures: A Randomized Controlled Trial. Pediatrics [Internet]. 2020;145:e20193182. Available at: https://pediatrics.aappublications.org. Accessed January 1, 2021.
Lynch NE, Stevenson NJ, Livingstone V, et al. The temporal evolution of electrographic seizure burden in neonatal hypoxic ischemic encephalopathy. Epilepsia. 2012;53:549–557.
Al-Muhtasib N, Sepulveda-Rodriguez A, Vicini S, et al. Neonatal phenobarbital exposure disrupts GABAergic synaptic maturation in rat CA1 neurons. Epilepsia. 2018;59:333–344.
Kaushal S, Tamer Z, Opoku F, et al. Anticonvulsant drug-induced cell death in the develo** white matter of the rodent brain. Epilepsia. 2016;57:727–734.
Forcelli PA, Kim J, Kondratyev A, et al. Pattern of antiepileptic drug-induced cell death in limbic regions of the neonatal rat brain. Epilepsia. 2011;52:e207–e211.
Noguchi KK, Fuhler NA, Wang SH, et al. Brain pathology caused in the neonatal macaque by short and prolonged exposures to anticonvulsant drugs. Neurobiol Dis [Internet]. 2021;149:105245. Available from: https://doi.org/10.1016/j.nbd.2020.105245. Accessed February 20, 2021.
Quinlan SMM, Rodriguez-Alvarez N, Molloy EJ, et al. Complex spectrum of phenobarbital effects in a mouse model of neonatal hypoxia-induced seizures. Sci Rep [Internet]. 2018;8:9986. Available from: https://www.nature.com/articles/s41598-018-28044-2. Accessed January 1, 2021.
Forcelli PA, Kozlowski R, Synder C, et al. Effects of Neonatal Antiepileptic Drug Exposure on Cognitive, Emotional, and Motor Function in Adult Rats. J Pharmacol Exp Ther [Internet]. 2012 [cited 2020 Dec 30];340:558–566. Available from: https://doi.org/10.1124/jpet.111.188862.
Singh D, Kumar P, Narang A. A randomized controlled trial of phenobarbital in neonates with hypoxic ischemic encephalopathy. J Matern Neonatal Med. 2005;18:391–395.
Young L, Berg M, Soll R. Prophylactic barbiturate use for the prevention of morbidity and mortality following perinatal asphyxia. Cochrane Database Syst. Rev.[Internet]; 2016:5(5):CD001240. Available from: https://doi.org/10.1002/14651858.CD001240.pub3/full. Accessed December 30, 2020.
Bohannon KK, Leung N, Cook AM, et al. Evaluation of two fosphenytoin loading dose regimens and monitoring in infants and neonates less than six months of age. J Pediatr Pharmacol Ther. 2020;25:617–622.
Morton LD. Clinical experience with fosphenytoin in children. J Child Neurol. 1998;13:19–22.
Al Za’abi M, Lanner A, **aonian X, et al. Application of routine monitoring data for determination of the population pharmacokinetics and enteral bioavailability of phenytoin in neonates and infants with seizures. Ther Drug Monit. 2006;28:793-799.
Alix V, James M, Jackson AH, et al. Efficacy of Fosphenytoin as First-Line Antiseizure Medication for Neonatal Seizures Compared to Phenobarbital. J Child Neurol. 2021;36:30-37.
Sicca F, Contaldo A, Rey E, et al. Phenytoin administration in the newborn and infant. Brain Dev. 2000;22:35–40.
Kriel RL, Cifuentes RF. Fosphenytoin in infants of extremely low birth weight. Pediatr Neurol. 2001;24:219–221.
Takeoka M, Kishnamoorthy K, Soman TB, et al. Fosphenytoin in Infants. J Child Neurol. 1997;13:537–540.
Bittigau P, Sifringer M, Ikonomidou C. Antiepileptic drugs and apoptosis in the develo** brain. Ann N Y Acad Sci. 2003;993:103-114.
Grinspan ZM, Shellhaas RA, Coryell J, et al. Comparative effectiveness of levetiracetam vs phenobarbital for infantile epilepsy. JAMA Pediatr. 2018;172:352-360.
Abend NS, Gutierrez-Colina AM, Monk HM, et al. Levetiracetam for treatment of neonatal seizures. J Child Neurol. 2011;26:465–470.
Ramantani G, Ikonomidou C, Walter B, et al. Levetiracetam: Safety and efficacy in neonatal seizures. Eur J Paediatr Neurol. 2011;15:1–7.
Khan O, Cipriani C, Wright C, et al. Role of intravenous levetiracetam for acute seizure management in preterm neonates. Pediatr Neurol. 2013;49:340–343.
Kurtom W, Courchia B, Pensirikul A, et al. Lack of response to treatment with levetiracetam in extreme preterm infants with seizures. J Perinatol. 2019;39:1480–1484.
Han JY, Moon CJ, Youn YA, et al. Efficacy of levetiracetam for neonatal seizures in preterm infants. BMC Pediatr. 2018;18:1–6.
Strasser K, Lueckemann L, Kluever V, et al. Dose-dependent effects of levetiracetam after hypoxia and hypothermia in the neonatal mouse brain. 2016 [cited 2020 Dec 30]; Available from: https://doi.org/10.1016/j.brainres.2016.05.040.
Falsaperla R, Mauceri L, Pavone P, et al. Short-term neurodevelopmental outcome in term neonates treated with phenobarbital versus levetiracetam: A single-center experience. Behav Neurol [Internet]. 2019;2019:3683548. Available at: https://www.hindawi.com. Accessed January 1, 2021.
Arican P, Olgac Dundar N, Mete Atasever N, et al. Comparison of the neurocognitive outcomes in term infants treated with levetiracetam and phenobarbital monotherapy for neonatal clinical seizures. Seizure [Internet]. 2020;80:71–74. Available at: https://www.seizure-journal.com. Accessed November 30, 2020.
Tsuchida TN, Wusthoff CJ, Shellhaas RA, et al. American clinical neurophysiology society standardized EEG terminology and categorization for the description of continuous eeg monitoring in neonates: Report of the american clinical neurophysiology society critical care monitoring committee. J Clin Neurophysiol. 2013;30:161–173.
Pavlidis E, Spagnoli C, Pelosi A, et al. Neonatal status epilepticus: Differences between preterm and term newborns. Eur J Paediatr Neurol [Internet]. 2015;19:314–319. Available from: https://doi.org/10.1016/j.ejpn.2015.01.002. Accessed November 30, 2020.
Torolira D, Suchomelova L, Wasterlain CG, et al. Phenobarbital and midazolam increase neonatal seizure-associated neuronal injury. Ann Neurol. 2017;82:115–120.
Dao K, Giannoni E, Diezi M, et al. Midazolam as a first-line treatment for neonatal seizures: Retrospective study. Pediatr Int. 2018;60:498–500.
Castro Conde JR, Hernández Borges AA, Doménech Martínez E, et al. Midazolam in neonatal seizures with no response to phenobarbital. Neurology. 2005;64:876-879.
Boylan GB, Rennie JM, Chorley G, et al. Second-line anticonvulsant treatment of neonatal seizures: A video-EEG monitoring study. Neurology. 2004;62:486-488.
Shany E, Benzaqen O, Watemberg N. Comparison of continuous drip of midazolam or lidocaine in the treatment of intractable neonatal seizures. J Child Neurol. 2007;22:255–259.
Duerden EG, Guo T, Dodbiba L, et al. Midazolam Dose Correlates with Abnormal Hippocampal Growth and Neurodevelopmental Outcome in Preterm Infants. Ann Neurol. 2016;79:548-559.
Favié LMA, Huitema ADR, van den Broek MPH, et al. Lidocaine as treatment for neonatal seizures: Evaluation of previously developed population pharmacokinetic models and dosing regimen. Br J Clin Pharmacol. 2020;86:75–84.
Malingré MM, Van Rooij LGM, Rademaker CMA, et al. Development of an optimal lidocaine infusion strategy for neonatal seizures. Eur J Pediatr. 2006;165:598–604.
Van Den Broek MPH, Huitema ADR, Van Hasselt JGC, et al. Lidocaine (lignocaine) dosing regimen based upon a population pharmacokinetic model for preterm and term neonates with seizures. Clin Pharmacokinet. 2011;50:461–469.
Weeke LC, Toet MC, Van Rooij LGM, et al. Lidocaine response rate in aEEG-confirmed neonatal seizures: Retrospective study of 413 full-term and preterm infants. Epilepsia. 2016;57:233–242.
Van Rooij LGM, Toet MC, Rademaker KMA, et al. Cardiac arrhythmias in neonates receiving lidocaine as anticonvulsive treatment. Eur. J. Pediatr. 2004;163:637–641.
Weeke LC, Schalkwijk S, Toet MC, et al. Lidocaine-Associated Cardiac Events in Newborns with Seizures: Incidence, Symptoms and Contributing Factors. Neonatology [Internet]. 2015;108:130–136. Available from: www.karger.com/neo. Accessed January 1, 2021.
Dzhala VI, Brumback AC, Staley KJ. Bumetanide enhances phenobarbital efficacy in a neonatal seizure model. Ann Neurol. 2008;63:222–235.
Johne M, Römermann K, Hampel P, et al. Phenobarbital and midazolam suppress neonatal seizures in a noninvasive rat model of birth asphyxia, whereas bumetanide is ineffective. Epilepsia. 2021;62:920–934.
Puskarjov M, Kahle KT, Ruusuvuori E, et al. Pharmacotherapeutic targeting of cation-chloride cotransporters in neonatal seizures. Epilepsia. 2014;55:806–818.
Pressler RM, Boylan GB, Marlow N, et al. Bumetanide for the treatment of seizures in newborn babies with hypoxic ischaemic encephalopathy (NEMO): An open-label, dose finding, and feasibility phase 1/2 trial. Lancet Neurol. 2015;14:469–477.
Thoresen M, Sabir H. Epilepsy: Neonatal seizure still lack safe and effective treatment. Nat Rev - Neurol. 2015;11:311–312.
Soul JS, Bergin AM, Stopp C, et al. A Pilot Randomized, Controlled, Double‐Blind Trial of Bumetanide to Treat Neonatal Seizures. Ann Neurol. 2021;89:327-340.
Follett PL, Deng W, Dai W, et al. Glutamate Receptor-Mediated Oligodendrocyte Toxicity in Periventricular Leukomalacia: A Protective Role for Topiramate. J Neurosci. 2004;24:4412–4420.
Glier C, Dzietko M, Bittigau P, et al. Therapeutic doses of topiramate are not toxic to the develo** rat brain. Exp Neurol. 2004;187:403–409.
Silverstein FS, Ferriero DM. Off-Label Use of Antiepileptic Drugs for the Treatment of Neonatal Seizures. Pediatr Neurol. 2008;39:77–79.
Nuñez-Ramiro A, Benavente-Fernández I, Valverde E, et al. Topiramate plus cooling for hypoxic-ischemic encephalopathy: A randomized, controlled, multicenter, double-blinded trial. Neonatology. 2019;116:76–84.
Filippi L, Fiorini P, Catarzi S, et al. Safety and efficacy of topiramate in neonates with hypoxic ischemic encephalopathy treated with hypothermia (NeoNATI): a feasibility study. J Matern Neonatal Med. 2018;31:973–980.
Glass HC, Poulin C, Shevell MI. Topiramate for the treatment of neonatal seizures. Pediatr Neurol. 2011;44:439–442.
Dupuis N, Matagne A, Staelens L, et al. Anti-ictogenic and antiepileptogenic properties of brivaracetam in mature and immature rats. Epilepsia. 2015;56:800–805.
Nissenkorn A, Tzadok M, Bar-Yosef O, et al. Treatment with brivaracetam in children – The experience of a pediatric epilepsy center. Epilepsy Behav. 2019;101(PtA):106541.
Liu E, Dilley D, McDonough B, et al. Safety and Tolerability of Adjunctive Brivaracetam in Pediatric Patients < 16 Years with Epilepsy: An Open-Label Trial. Pediatr Drugs. 2019;21:291–301.
McGuire S, Silva G, Lal D, et al. Safety and Efficacy of Brivaracetam in Pediatric Refractory Epilepsy: A Single-Center Clinical Experience. J Child Neurol. 2020;35:102–105.
Welsh SS, Lin N, Topjian AA, et al. Safety of intravenous lacosamide in critically ill children. Seizure. 2017;52:76–80.
Licko T, Seeger N, Zellinger C, et al. Lacosamide treatment following status epilepticus attenuates neuronal cell loss and alterations in hippocampal neurogenesis in a rat electrical status epilepticus model. Epilepsia. 2013;54:1176–1185.
Wang B, Dawson H, Wang H, et al. Lacosamide improves outcome in a murine model of traumatic brain injury. Neurocrit Care. 2013;19:125–134.
Kim GH, Byeon JH, Eun BL. Neuroprotective effect of lacosamide on hypoxic-ischemic brain injury in neonatal rats. J Clin Neurol. 2017;13:138–143.
Arkilo D, Gustafson M, Ritter FJ. Clinical experience of intravenous lacosamide in infants and young children. Eur J Paediatr Neurol. 2016;20:212–217.
Hadar F-H, Eli H, Ayelet L, et al. Lacosamide for SCN2A-related intractable neonatal and infantile seizures. Epileptic Disord. 2018;20:440–446.
Naylor DE, Liu H, Wasterlain CG. Trafficking of GABAA receptors, loss of inhibition, and a mechanism for pharmacoresistance in status epilepticus. J Neurosci. 2005;25:7724–7733.
Chen J, Naylor DE, Wasterlain CG. Advances in the pathophysiology of status epilepticus. Acta Neurol Scand. 2007;186:7–15.
Mazarati AM, Wasterlain CG. N-Methyl-D-asparate receptor antagonists abolish the maintenance phase of self-sustaining status epilepticus in rat. Neurosci Lett. 1999;265:187–190.
Wasterlain CG, Chen JWY. Mechanistic and pharmacologic aspects of status epilepticus and its treatment with new antiepileptic drugs. Epilepsia. 2008;49:63-73.
Spandou E, Karkavelas G, Soubasi V, et al. Effect of ketamine on hypoxic–ischemic brain damage in newborn rats. Brain Res. 1999;819:1–7.
Brambrink AM, Evers AS, Avidan MS, et al. Ketamine-induced Neuroapoptosis in the Fetal and Neonatal Rhesus Macaque Brain. Anesthesiology. 2012;116:372–384.
Paule MG, Li M, Allen RR, et al. Ketamine anesthesia during the first week of life can cause long-lasting cognitive deficits in rhesus monkeys. Neurotoxicol Teratol. 2011;33:220–230.
Elalouf C, Le Moing AG Le, Fontaine C, et al. Prospective follow-up of a cohort of preterm infants < 33 WG receiving ketamine for tracheal intubation in the delivery room: Neurological outcome at 1 and 2 years. Arch Pediatr. 2018;25:295–300.
Tarocco A, Ballardini E, Garani G. Use of ketamine in a newborn with refractory status epilepticus: A case report. Pediatr Neurol. 2014;51:154–156.
Freibauer A, Jones K. KCNQ2 mutation in an infant with encephalopathy of infancy with migrating focal seizures. Epileptic Disord. 2018;20:541–544.
Höfler J, Trinka E. Intravenous ketamine in status epilepticus. Epilepsia. 2018;59:198-206.
Yager JY, Ashwal S. Animal Models of Perinatal Hypoxic-Ischemic Brain Damage. Pediatr Neurol. 2009;40:156–167.
Sun H, Juul HM, Jensen FE. Models of hypoxia and ischemia-induced seizures. J Neurosci Methods. 2016;260:252–260.
Chiba S. Long-term effect of postnatal hypoxia on the seizure susceptibility in rats. Life Sci. 1985;37:1597–1604.
Jensen FE, Applegate CD, Holtzman D, et al. Epileptogenic effect of hypoxia in the immature rodent brain. Ann Neurol. 1991;29:629–637.
Levine S. Anoxic-Ischemic Encephalopathy in Rats. Am J Pathol. 1960;36:1–17.
Rice JE, Vannucci RC, Brierley JB. The influence of immaturity on hypoxic-ischemic brain damage in the rat. Ann Neurol. 1981;9:131–141.
Zhang Y, Zhang M, Liu S, et al. Xenon exerts anti-seizure and neuroprotective effects in kainic acid-induced status epilepticus and neonatal hypoxia-induced seizure. Exp Neurol. 2019;322:113054.
Nolan SO, Hodges SL, Condon SM, et al. High seizure load during sensitive periods of development leads to broad shifts in ultrasonic vocalization behavior in neonatal male and female C57BL/6J mice. Epilepsy Behav. 2019;95:26–33.
Chapman KE, Raol YH, Brooks-Kayal A. Neonatal seizures: Controversies and challenges in translating new therapies from the lab to the isolette. Eur J Neurosci. 2012;35:1857–1865.
Harish S, Bhuvana K, Bengalorkar GM, et al. Flupirtine: Clinical pharmacology. J Anaesthesiol Clin Pharmacol. 2012;28:172–177.
Raol YSH, Lapides DA, Keating JG, et al. A KCNQ channel opener for experimental neonatal seizures and status epilepticus. Ann Neurol. 2009;65:326–336.
Sampath D, Shmueli D, White AM, et al. Flupirtine effectively prevents development of acute neonatal seizures in an animal model of global hypoxia. Neurosci Lett. 2015;607:46–51.
Sampath D, Valdez R, White AM, et al. Anticonvulsant effect of flupirtine in an animal model of neonatal hypoxic-ischemic encephalopathy. Neuropharmacology. 2017;123:126–135.
Sampath D, Lam PM, Laoprasert M, et al. Effects of a potassium channel opener on brain injury and neurologic outcomes in an animal model of neonatal hypoxic–ischemic injury. Pediatr Res. 2020;88:202–208.
European Medicines Agency. Withdrawal of pain medicine flupirtine endorsed [Internet]. 2018. Available from: https://www.ema.europa.eu/en/documents/referral/flupirtine-article-31-referral-withdrawal-pain-medicine-flupirtine-endorsed_en.pdf. Accessed January 2, 2021.
Forcelli PA, Soper C, Lakhkar A, et al. Anticonvulsant effect of retigabine during postnatal development in rats. Epilepsy Res. 2012;101:135–140.
Millichap JJ, Park KL, Tsuchida T, et al. KCNQ2 encephalopathy: Features, mutational hot spots, and ezogabine treatment of 11 patients. Neurol Genet. 2016;2;e96.
Kang SK, Johnston M V., Kadam SD. Acute TrkB inhibition rescues phenobarbital-resistant seizures in a mouse model of neonatal ischemia. Eur J Neurosci. 2015;42:2792–2804.
Carter BM, Sullivan BJ, Landers JR, et al. Dose-dependent reversal of KCC2 hypofunction and phenobarbital-resistant neonatal seizures by ANA12. Sci Rep. 2018;8:11987.
Kang SK, Ammanuel S, Adler DA, et al. Rescue of PB-resistant neonatal seizures with single-dose of small-molecule TrkB antagonist show long-term benefits. Epilepsy Res. 2020;159:106249.
Kipnis PA, Sullivan BJ, Carter BM, et al. TrkB agonists prevent postischemic emergence of refractory neonatal seizures in mice. JCI Insight. 2020;5:e136007.
Obeid M, Rosenberg EC, Klein PM, et al. Lestaurtinib (CEP-701) attenuates “second hit” kainic acid-induced seizures following early life hypoxic seizures. Epilepsy Res. 2014;108:806–810.
Huizenga MN, Wicker E, Beck VC, et al. Anticonvulsant effect of cannabinoid receptor agonists in models of seizures in develo** rats. Epilepsia. 2017;58:1593–1602.
Huizenga MN, Sepulveda-Rodriguez A, Forcelli PA. Preclinical safety and efficacy of cannabidivarin for early life seizures. Neuropharmacology. 2019;148:189–198.
Badowski S, Smith G. Cannabis use during pregnancy and postpartum. Can Fam Physician. 2020;66:98–103.
Ziobro J, Shellhaas RA. Neonatal Seizures: Diagnosis, Etiologies, and Management. Semin Neurol. 2020;40:246–256.
Janicot R, Stafstrom CE, Shao LR. 2-Deoxyglucose terminates pilocarpine-induced status epilepticus in neonatal rats. Epilepsia. 2020;61:1528–1537.
Wu Z, Huo Q, Ren L, et al. Gluconate suppresses seizure activity in develo** brains by inhibiting CLC-3 chloride channels. Mol Brain. 2019;12:50.
Grosenbaugh DK, Ross BM, Wagley P, et al. The Role of Kainate Receptors in the Pathophysiology of Hypoxia-Induced Seizures in the Neonatal Mouse. Sci Rep. 2018;8:7035.
Aujla PK, Fetell MR, Jensen FE. Talampanel suppresses the acute and chronic effects of seizures in a rodent neonatal seizure model. Epilepsia. 2009;50:694–701.
Nielsen O., Feit PW. Structure-activity relationships of aminobenzoic acid diuretics and related compounds (1). Diuret Agens. 1978;83:12–23.
Brandt C, Seja P, Töllner K, et al. Bumepamine, a brain-permeant benzylamine derivative of bumetanide, does not inhibit NKCC1 but is more potent to enhance phenobarbital’s anti-seizure efficacy. Neuropharmacology. 2018;143:186–204.
Guillet R, Kwon J. Seizure recurrence and developmental disabilities after neonatal seizures: Outcomes are unrelated to use of phenobarbital prophylaxis. J Child Neurol. 2007;22:389–395.
Natarajan N, Beatty CW, Gust J, et al. Provider Practices of Phenobarbital Discontinuation in Neonatal Seizures. J Child Neurol. 2018;33:153–157.
Fitzgerald MP, Kessler SK, Abend NS. Early discontinuation of antiseizure medications in neonates with hypoxic–ischemic encephalopathy. Epilepsia. 2017;58:1047–1053.
Glass HC, Soul JS, Chan T, et al. Duration of antiseizure medication treatment and 2-year outcome after acute symptomatic neonatal seizures - a Neonatal Seizure Registry study. 16th Int Child Neurol Virtual Congr. 2020.
Bartha AI, Shen J, Katz KH, et al. Neonatal Seizures: Multicenter Variability in Current Treatment Practices. Pediatr Neurol. 2007;37:85–90.
Wietstock SO, Bonifacio SL, McCulloch CE, et al. Neonatal neurocritical care service is associated with decreased administration of seizure medication. J Child Neurol. 2015;30:1135–1141.
Cornet MC, Sands TT, Cilio MR. Neonatal epilepsies: Clinical management. Semin Fetal Neonatal Med. 2018;23:204–212.
Kaur S, Pappas K. Genetic Etiologies of Neonatal Seizures. Neoreviews. 2020;21:e663-e672.
Moavero R, Kotulska K, Lagae L, et al. Is autism driven by epilepsy in infants with Tuberous Sclerosis Complex? Ann Clin Transl Neurol. 2020;7:1371–1381.
Tye C, Mcewen FS, Liang H, et al. Long-term cognitive outcomes in tuberous sclerosis complex. Dev Med Child Neurol. 2020;62:322–329.
Parrini E, Conti V, Dobyns WB, et al. Genetic basis of brain malformations. Mol Syndromol. 2016;7:220–233.
Saffari A, Brösse I, Wiemer-Kruel A, et al. Safety and efficacy of mTOR inhibitor treatment in patients with tuberous sclerosis complex under 2 years of age - A multicenter retrospective study. Orphanet J Rare Dis. 2019;14:1–13.
Wilmshurst JM, Gaillard WD, Vinayan KP, et al. Summary of recommendations for the management of infantile seizures: Task Force Report for the ILAE Commission of Pediatrics. Epilepsia. 2015;56:1185–1197.
Pearl PL. Amenable Treatable Severe Pediatric Epilepsies. Semin Pediatr Neurol. 2016;23:158–166.
Schwahn BC, Van Spronsen FJ, Belaidi AA, et al. Efficacy and safety of cyclic pyranopterin monophosphate substitution in severe molybdenum cofactor deficiency type A: A prospective cohort study. Lancet. 2015;386:1955–1963.
Reiss J. Molybdenum cofactor deficiency type B knock-in mouse models carrying patient-identical mutations and their rescue by singular AAV injections. Hum Genet. 2019;138:355–361.
Pena IA, MacKenzie A, Van Karnebeek CDM. Current knowledge for pyridoxine-dependent epilepsy: a 2016 update. Expert Rev Endocrinol Metab. 2017;12:5–20.
Pérez B, Gutiérrez-Solana LG, Verdú A, et al. Clinical, biochemical, and molecular studies in pyridoxine-dependent epilepsy. Antisense therapy as possible new therapeutic option. Epilepsia. 2013;54:239–248.
Al Teneiji A, Bruun TUJ, Cordeiro D, et al. Phenotype, biochemical features, genotype and treatment outcome of pyridoxine-dependent epilepsy. Metab Brain Dis. 2017;32:443–451.
Poletti V, Biffi A. Gene-Based Approaches to Inherited Neurometabolic Diseases. Hum Gene Ther. 2019;30:1222–1235.
Hinderer C, Bell P, Louboutin J-P, et al. Neonatal tolerance induction enables accurate evaluation of gene therapy for MPS I in a canine model. Mol Genet Metab. 2016;119:124–130.
Pearl PL. Epilepsy Syndromes in Childhood. Continuum. 2018;24:186–209.
Maljevic S, Lerche H. Potassium channel genes and benign familial neonatal epilepsy. Prog Brain Res. 2014;213:17-53.
Reif PS, Tsai MH, Helbig I, et al. Precision medicine in genetic epilepsies: break of dawn? Expert Rev Neurother. 2017;17:381–392.
Pisano T, Numis AL, Heavin SB, et al. Early and effective treatment of KCNQ2 encephalopathy. Epilepsia. 2015;56:685–691.
Scheffer IE, Nabbout R. SCN1A-related phenotypes: Epilepsy and beyond. Epilepsia. 2019;60:S17–S24.
Sadleir LG, Mountier EI, Gill D, et al. Not all SCN1A epileptic encephalopathies are Dravet syndrome. Neurology. 2017;89:1035–1042.
Berecki G, Bryson A, Terhag J, et al. SCN1A gain of function in early infantile encephalopathy. Ann Neurol. 2019;85:514–525.
Reynolds C, King MD, Gorman KM. The phenotypic spectrum of SCN2A-related epilepsy. Eur J Paediatr Neurol. 2020;24:117–122.
Wolff M, Johannesen KM, Hedrich UBS, et al. Genetic and phenotypic heterogeneity suggest therapeutic implications in SCN2A-related disorders. Brain. 2017;140:1316–1336.
McTague A, Appleton R, Avula S, et al. Migrating partial seizures of infancy: Expansion of the electroclinical, radiological and pathological disease spectrum. Brain. 2013;136:1578–1591.
Milligan CJ, Li M, Gazina EV, et al. KCNT1 gain of function in 2 epilepsy phenotypes is reversed by quinidine. Ann Neurol. 2014;75:581-590.
Mikati MA, Jiang YH, Carboni M, et al. Quinidine in the treatment of KCNT1-positive epilepsies. Ann Neurol. 2015;78:995–999.
Bearden D, Strong A, Ehnot J, et al. Targeted treatment of migrating partial seizures of infancy with quinidine. Ann Neurol. 2014;76:457–461.
Borlot F, Abushama A, Morrison‐Levy N, et al. KCNT1‐related epilepsy: An international multicenter cohort of 27 pediatric cases. Epilepsia. 2020;61:679–692.
Fitzgerald MP, Fiannacca M, Smith DM, et al. Treatment Responsiveness in KCNT1-Related Epilepsy. Neurotherapeutics. 2019;16:848–857.
Rizzo F, Ambrosino P, Guacci A, et al. Characterization of two de novo KCNT1 mutations in children with malignant migrating partial seizures in infancy. Mol Cell Neurosci. 2016;72:54–63.
Pressler RM, Lagae L. Why we urgently need improved seizure and epilepsy therapies for children and neonates. Neuropharmacology. 2020;170:107854.
Grinspan ZM, Patel AD, Shellhaas RA, et al. Design and implementation of electronic health record common data elements for pediatric epilepsy: Foundations for a learning health care system. Epilepsia. 2021;62:198-216.
Wusthoff CJ, Sullivan J, Glass HC, et al. Interrater agreement in the interpretation of neonatal electroencephalography in hypoxic-ischemic encephalopathy. Epilepsia. 2017;58:429–435.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ziobro, J.M., Eschbach, K. & Shellhaas, R.A. Novel Therapeutics for Neonatal Seizures. Neurotherapeutics 18, 1564–1581 (2021). https://doi.org/10.1007/s13311-021-01085-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13311-021-01085-8