Abstract
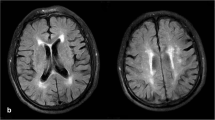
Leukoaraiosis (LA) is associated with structural and functional cerebrovascular impairment, which may compromise the capacity of ischemic tissue to maximize reperfusion after intravenous thrombolysis (IVT). We aimed to determine whether severe LA is correlated with reperfusion inefficiency, which contributes to infarct growth and poor functional outcome. We analyzed data from our consecutive acute ischemic stroke (AIS) patients who had acquired baseline and 24-h follow-up diffusion- and perfusion-weighted imaging. Reperfusion was defined as reduction of ≥70 % of hypoperfusion lesion at 24 h from baseline. Severe LA was defined as Fazekas score 2 or 3 on FLAIR images. We investigated the relationship between severity of LA and reperfusion status. Multivariate statistical analysis was carried out for modeling the independent predictors of reperfusion, infarct growth, and functional outcome. Finally, 79 patients were included, among them 30 (37.97 %) had severe LA. Reperfusion was observed in 41 (51.89 %) patients, the proportion of reperfusion was very similar in patients with and without severe LA (53.33 vs 51.02 %, p = 1.000). Large artery occlusion was the only independent unfavorable predictor for reperfusion (OR = 0.202, 95 % confidence interval, 0.060–0.673; p = 0.014). Multiple linear regression analysis revealed that severe LA was independently associated with infarct growth (standardized coefficients = 0.191, p = 0.040). Severe LA was also an independent predictor of poor outcome (mRS ≥ 3) (OR = 4.004, 95 % confidence interval, 1.267–12.656, p = 0.018) after adjusting for reperfusion and baseline severity of stroke. Severe LA was associated with infarct growth and poor outcome independent of reperfusion status, which may expand the notion that LA contributes the intrinsic vulnerability of brain tissue to acute ischemic insults. The burden of LA may not serve as an imaging indicator of reperfusion inefficiency after IVT for AIS patients.
Similar content being viewed by others
References
Arsava EM, Rahman R, Rosand J, Lu J, Smith EE, Rost NS, et al. Severity of leukoaraiosis correlates with clinical outcome after ischemic stroke. Neurology. 2009;72(16):1403–10. doi:10.1212/WNL.0b013e3181a18823.
Feng C, Tan Y, Wu YF, Xu Y, Hua T, Huang J, et al. Leukoaraiosis correlates with the neurologic deterioration after small subcortical infarction. J Stroke Cerebrovasc Dis : Off J Nat Stroke Assoc. 2014;23(6):1513–8. doi:10.1016/j.jstrokecerebrovasdis.2013.12.032.
Ay H, Arsava EM, Rosand J, Furie KL, Singhal AB, Schaefer PW, et al. Severity of leukoaraiosis and susceptibility to infarct growth in acute stroke. Stroke; J Cereb Circ. 2008;39(5):1409–13. doi:10.1161/STROKEAHA.107.501932.
Henninger N, Lin E, Haussen DC, Lehman LL, Takhtani D, Selim M, et al. Leukoaraiosis and sex predict the hyperacute ischemic core volume. Stroke; J Cereb Circ. 2013;44(1):61–7. doi:10.1161/STROKEAHA.112.679084.
Giurgiutiu DV, Yoo AJ, Fitzpatrick K, Chaudhry Z, Leslie-Mazwi T, Schwamm LH, et al. Severity of leukoaraiosis, leptomeningeal collaterals, and clinical outcomes after intra-arterial therapy in patients with acute ischemic stroke. J Neurointerventional surg. 2015;7(5):326–30. doi:10.1136/neurintsurg-2013-011083.
Tomimoto H, Akiguchi I, Wakita H, Osaki A, Hayashi M, Yamamoto Y. Coagulation activation in patients with Binswanger disease. Arch Neurol. 1999;56(9):1104–8. doi:10.1001/archneur.56.9.1104.
Iwamoto T, Kubo H, Takasaki M. Platelet activation in the cerebral-circulation in different subtypes of ischemic stroke and Binswangers-disease. Stroke; J Cereb Circ. 1995;26(1):52–6.
Xu H, Stamova B, Jickling G, Tian Y, Zhan X, Ander BP, et al. Distinctive RNA expression profiles in blood associated with white matter hyperintensities in brain. Stroke; J Cereb Circ. 2010;41(12):2744–9. doi:10.1161/STROKEAHA.110.591875.
Uh J, Yezhuvath U, Cheng Y, Lu H. In vivo vascular hallmarks of diffuse leukoaraiosis. J Magn Reson Imaging : JMRI. 2010;32(1):184–90. doi:10.1002/jmri.22209.
Purkayastha S, Fadar O, Mehregan A, Salat DH, Moscufo N, Meier DS, et al. Impaired cerebrovascular hemodynamics are associated with cerebral white matter damage. J Cereb Blood Flow Metab. 2014;34(2):228–34. doi:10.1038/jcbfm.2013.180.
Fazekas F, Kleinert R, Offenbacher H, Schmidt R, Kleinert G, Payer F, et al. Pathological correlates of incidental MRI white-matter signal hyperintensities. Neurology. 1993;43(9):1683–9.
Brown WR, Moody DM, Challa VR, Thore CR, Anstrom JA. Venous collagenosis and arteriolar tortuosity in leukoaraiosis. J Neurol Sci. 2002;203–204:159–63.
Zupan M, Sabovic M, Zaletel M, Popovic KS, Zvan B. The presence of cerebral and/or systemic endothelial dysfunction in patients with leukoaraiosis—a case control pilot study. BMC Neurol. 2015;15:158. doi:10.1186/s12883-015-0416-z.
Zhang J, Puri AS, Khan MA, Goddeau Jr RP, Henninger N. Leukoaraiosis predicts a poor 90-day outcome after endovascular stroke therapy. AJNR Am J Neuroradiol. 2014;35(11):2070–5. doi:10.3174/ajnr.A4029.
Arba F, Palumbo V, Boulanger JM, Pracucci G, Inzitari D, Buchan AM, et al. Leukoaraiosis and lacunes are associated with poor clinical outcomes in ischemic stroke patients treated with intravenous thrombolysis. Int J Stroke. 2016;11(1):62–7. doi:10.1177/1747493015607517.
Zhang S, Tang H, Yu YN, Yan SQ, Parsons MW, Lou M. Optimal magnetic resonance perfusion thresholds identifying ischemic penumbra and infarct core: a Chinese population-based study. CNS Neurosci Ther. 2015;21(3):289–95. doi:10.1111/cns.12367.
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities AT 1.5-T in Alzheimer dementia and normal aging. Am J Roentgenol. 1987;149(2):351–6.
Cho TH, Nighoghossian N, Mikkelsen IK, Derex L, Hermier M, Pedraza S, et al. Reperfusion within 6 hours outperforms recanalization in predicting penumbra salvage, lesion growth, final infarct, and clinical outcome. Stroke; J Cereb Circ. 2015;46(6):1582–9. doi:10.1161/STROKEAHA.114.007964.
Dalkara T, Arsava EM. Can restoring incomplete microcirculatory reperfusion improve stroke outcome after thrombolysis? J Cereb Blood Flow Metab : Off J Int Soc Cereb Blood Flow Metab. 2012;32(12):2091–9. doi:10.1038/jcbfm.2012.139.
Heistad DD, Mayhan WG, Coyle P, Baumbach GL. Impaired dilatation of cerebral arterioles in chronic hypertension. Blood Vessels. 1990;27(2–5):258–62.
del Zoppo GJ, Mabuchi T. Cerebral microvessel responses to focal ischemia. J Cereb Blood Flow Metab : Off J Int Soc Cereb Blood Flow Metab. 2003;23(8):879–94. doi:10.1097/01.WCB.0000078322.96027.78.
Moody DM, Thore CR, Anstrom JA, Challa VR, Langefeld CD, Brown WR. Quantification of afferent vessels shows reduced brain vascular density in subjects with leukoaraiosis. Radiology. 2004;233(3):883–90. doi:10.1148/radiol.2333020981.
Warach S, Latour LL. Evidence of reperfusion injury, exacerbated by thrombolytic therapy, in human focal brain ischemia using a novel imaging marker of early blood–brain barrier disruption. Stroke; J Cereb Circ. 2004;35(11):2659–61. doi:10.1161/01.str.0000144051.32131.09.
Topakian R, Barrick TR, Howe FA, Markus HS. Blood–brain barrier permeability is increased in normal-appearing white matter in patients with lacunar stroke and leucoaraiosis. J Neurol Neurosurg Psychiatry. 2010;81(2):192–7. doi:10.1136/jnnp.2009.172072.
Chen B, Friedman B, Cheng Q, Tsai P, Schim E, Kleinfeld D, et al. Severe blood–brain barrier disruption and surrounding tissue injury. Stroke; J Cereb Circ. 2009;40(12):e666–74. doi:10.1161/STROKEAHA.109.551341.
Tuladhar AM, Reid AT, Shumskaya E, de Laat KF, van Norden AG, van Dijk EJ, et al. Relationship between white matter hyperintensities, cortical thickness, and cognition. Stroke; J Cereb Circ. 2015. doi:10.1161/STROKEAHA.114.007146.
Kim JT, Park MS, Yoon GJ, Jung HJ, Choi KH, Nam TS, et al. White matter hyperintensity as a factor associated with delayed mood disorders in patients with acute ischemic stroke. Eur Neurol. 2011;66(6):343–9. doi:10.1159/000332585.
Yamawaki M, Wada-Isoe K, Yamamoto M, Nakashita S, Uemura Y, Takahashi Y et al. Association of cerebral white matter lesions with cognitive function and mood in Japanese elderly people: a population-based study. Brain and Behavior. 2015;5(3). doi:10.1002/brb3.315.
Senda J, Ito K, Kotake T, Kanamori M, Kishimoto H, Kadono I, et al. Association of leukoaraiosis with convalescent rehabilitation outcome in patients with ischemic stroke. Stroke; J Cereb Circ. 2015. doi:10.1161/STROKEAHA.115.010682.
Zhang C, Wang Y, Zhao X, Wang C, Liu L, Pu Y, et al. Factors associated with severity of leukoaraiosis in first-ever lacunar stroke and atherosclerotic ischemic stroke patients. J Stroke Cerebrovasc Dis : Off J Nat Stroke Assoc. 2014;23(10):2862–8. doi:10.1016/j.jstrokecerebrovasdis.2014.07.021.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Compliance with Ethics Requirements
The study procedures were in accordance with the Helsinki Declaration of 1975. Informed consent was obtained from all individual participants included in the study. The protocol of this study had been approved by the human ethics committee of a local hospital.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Zhong, G., Yan, S., Zhang, S. et al. Association between Leukoaraiosis and Poor Outcome is not due to Reperfusion Inefficiency after Intravenous Thrombolysis. Transl. Stroke Res. 7, 439–445 (2016). https://doi.org/10.1007/s12975-016-0473-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-016-0473-7