Abstract
Purpose
General anesthesia for Cesarean delivery affects maternal and neonatal outcomes. We aimed to evaluate temporal trends in anesthesia management for Cesarean deliveries over 16 years and analyze interinstitutional variations in general anesthesia use in Japan.
Methods
In this retrospective cohort study, we obtained patient data from the nationwide health insurance claims database containing data for ten million individuals. We included patients who underwent Cesarean delivery between 1 January 2005 and 31 August 2021. The primary outcome was the use of general anesthesia. We evaluated institutional variations in general anesthesia use in medical facilities using two-level hierarchical logistic regression analyses with median odds ratios and intraclass correlation coefficients.
Results
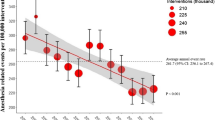
The cohort included 86,793 patients who underwent 102,617 Cesarean deliveries at 2,496 institutions. General anesthesia was used in 3.7% (95% confidence interval [CI], 3.6 to 3.9) of all Cesarean deliveries. The temporal trend in the use of general anesthesia decreased gradually from 10.8% in 2005 to 2.9% in 2021 (P for trend < 0.001). The adjusted median odds ratio for medical facilities was 6.1 (95% CI, 5.9 to 6.7), and the intraclass correlation coefficient was 0.52 (95% CI, 0.51 to 0.55).
Conclusion
Although the rate of general anesthesia use for Cesarean delivery in Japan decreased gradually from 2005 to 2021, general anesthesia was used in 3.7% of all Cesarean deliveries. The use of general anesthesia varied significantly across institutions, and 52% of the overall variations in general anesthesia practice can be explained by differences between facilities.
Résumé
Objectif
L’anesthésie générale pour l’accouchement par césarienne affecte les issues maternelles et néonatales. Notre objectif était d’évaluer les tendances temporelles de la prise en charge anesthésique pour les accouchements par césarienne sur 16 ans et d’analyser les variations interinstitutionnelles dans l’utilisation de l’anesthésie générale au Japon.
Méthode
Dans cette étude de cohorte rétrospective, nous avons obtenu des données sur les patient·es à partir de la base de données nationale des réclamations d’assurance maladie contenant des données pour dix millions de personnes. Nous avons inclus les personnes ayant bénéficié d’un accouchement par césarienne entre le 1er janvier 2005 et le 31 août 2021. Le critère d’évaluation principal était le taux d’utilisation de l’anesthésie générale. Nous avons évalué les variations institutionnelles dans l’utilisation de l’anesthésie générale dans les établissements médicaux à l’aide d’analyses de régression logistique hiérarchique à deux niveaux avec des rapports de cotes médians et des coefficients de corrélation intraclasse.
Résultats
La cohorte comprenait 86 793 patient·es ayant bénéficié de 102 617 accouchements par césarienne dans 2496 établissements. L’anesthésie générale a été utilisée dans 3,7 % (intervalle de confiance [IC] à 95 %, 3,6 à 3,9) de tous les accouchements par césarienne. La tendance temporelle de l’utilisation de l’anesthésie générale a diminué graduellement, passant de 10,8 % en 2005 à 2,9 % en 2021 (P pour la tendance < 0,001). Le rapport de cotes médian ajusté pour les établissements médicaux était de 6,1 (IC 95 %, 5,9 à 6,7), et le coefficient de corrélation intraclasse était de 0,52 (IC 95 %, 0,51 à 0,55).




Similar content being viewed by others
References
Boerma T, Ronsmans C, Melesse DY, et al. Global epidemiology of use of and disparities in Caesarean sections. Lancet 2018; 392: 1341–8. https://doi.org/10.1016/s0140-6736(18)31928-7
Maeda E, Ishihara O, Tomio J, et al. Cesarean section rates and local resources for perinatal care in Japan: a nationwide ecological study using the national database of health insurance claims. J Obstet Gynaecol Res 2018; 44: 208–16. https://doi.org/10.1111/jog.13518
Maeda E, Ishihara O, Tomio J, et al. Cesarean delivery rates for overall and multiple pregnancies in Japan: a descriptive study using nationwide health insurance claims data. J Obstet Gynaecol Res 2021; 47: 2099–109. https://doi.org/10.1111/jog.14772
Ministry of Health, Labour and Welfare. Survey of medical institutions [Japanese]. Available from URL: https://www.mhlw.go.jp/toukei/saikin/hw/iryosd/20/dl/02sisetu02.pdf (accessed July 2023).
American Society of Anesthesiologists Task Force on Obstetric Anesthesia and the Society for Obstetric Anesthesia and Perinatology. Practice guidelines for obstetric anesthesia: an updated report by the American Society of Anesthesiologists Task Force on Obstetric Anesthesia and the Society for Obstetric Anesthesia and Perinatology. Anesthesiology 2016; 124: 270–300. https://doi.org/10.1097/aln.0000000000000935
Ring L, Landau R, Delgado C. The current role of general anesthesia for Cesarean delivery. Curr Anesthesiol Rep 2021; 11: 18–27. https://doi.org/10.1007/s40140-021-00437-6
Evans E. Information for mothers about analgesia and anaesthesia during delivery. In: Lucas N (Ed.). Raising the Standards: Royal College of Anaesthetists Quality Improvement Compendium, 4th edition. London: The Royal College of Anaesthetists; 2020: 241–68.
Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Epidemiology 2007; 18: 805–35. https://doi.org/10.1097/ede.0b013e3181577511
Kimura S, Sato T, Ikeda S, Noda M, Nakayama T. Development of a database of health insurance claims: standardization of disease classifications and anonymous record linkage. J Epidemiol 2010; 20: 413–9. https://doi.org/10.2188/jea.je20090066
Yonekura H, Ide K, Seto K, et al. Preoperative pulmonary function tests before low-risk surgery in Japan: a retrospective cohort study using a claims database. J Anesth 2018; 32: 23–32. https://doi.org/10.1007/s00540-017-2423-2
Yonekura H, Seto K, Ide K, et al. Preoperative blood tests conducted before low-risk surgery in Japan: a retrospective observational study using a nationwide insurance claims database. Anesth Analg 2018; 126: 1633–40. https://doi.org/10.1213/ane.0000000000002734
Yonekura H, Ide K, Kanazawa Y, et al. Use of preoperative haemostasis and ABO blood ty** tests in children: a retrospective observational study using a nationwide claims database in Japan. BMJ Open 2019; 9: e032306. https://doi.org/10.1136/bmjopen-2019-032306
Abe H, Sumitani M, Uchida K, et al. Association between mode of anaesthesia and severe maternal morbidity during admission for scheduled Caesarean delivery: a nationwide population-based study in Japan, 2010–2013. Br J Anaesth 2018; 120: 779–89. https://doi.org/10.1016/j.bja.2017.11.101
Guglielminotti J, Landau R, Li G. Adverse events and factors associated with potentially avoidable use of general anesthesia in Cesarean deliveries. Anesthesiology 2019; 130: 912–22. https://doi.org/10.1097/aln.0000000000002629
Bateman BT, Mhyre JM, Hernandez-Diaz S, et al. Development of a comorbidity index for use in obstetric patients. Obstet Gynecol 2013; 122: 957–65. https://doi.org/10.1097/aog.0b013e3182a603bb
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005; 43: 1130–9. https://doi.org/10.1097/01.mlr.0000182534.19832.83
Aoyama K, D'Souza R, Inada E, Lapinsky SE, Fowler RA. Measurement properties of comorbidity indices in maternal health research: a systematic review. BMC Pregnancy Childbirth 2017; 17: 372. https://doi.org/10.1186/s12884-017-1558-3
Metcalfe A, Lix LM, Johnson JA, et al. Validation of an obstetric comorbidity index in an external population. BJOG 2015; 122: 1748–55. https://doi.org/10.1111/1471-0528.13254
Singh S, Farber MK, Bateman BT, et al. Obstetric comorbidity index and the odds of general vs. neuraxial anesthesia in women undergoing Cesarean delivery: a retrospective cohort study. Int J Obstet Anesth 2022; 51: 103546. https://doi.org/10.1016/j.ijoa.2022.103546
Yonekura H, Mazda Y, Noguchi S, Tsunobuchi H, Shimaoka M. Current epidemiology of the general anesthesia practice for Cesarean delivery using a nationwide claims database in Japan: a descriptive study. J Clin Med 2022; 11: 4808. https://doi.org/10.3390/jcm11164808
Odor PM, Bampoe S, Moonesinghe SR, et al. General anaesthetic and airway management practice for obstetric surgery in England: a prospective, multicentre observational study. Anaesthesia 2021; 76: 460–71. https://doi.org/10.1111/anae.15250
Ooba N, Setoguchi S, Ando T, et al. Claims-based definition of death in Japanese claims database: validity and implications. PLoS One 2013; 8: e66116. https://doi.org/10.1371/journal.pone.0066116
Guglielminotti J, Wong CA, Landau R, Li G. Temporal trends in anesthesia-related adverse events in Cesarean deliveries, New York State, 2003–2012. Anesthesiology 2015; 123: 1013–23. https://doi.org/10.1097/aln.0000000000000846
Butwick AJ, Bentley J, Wong CA, Snowden JM, Sun E, Guo N. United States state-level variation in the use of neuraxial analgesia during labor for pregnant women. JAMA Netw Open 2018; 1: e186567. https://doi.org/10.1001/jamanetworkopen.2018.6567
Merlo J, Chaix B, Ohlsson H, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health 2006; 60: 290–7. https://doi.org/10.1136/jech.2004.029454
Guasch E, Brogly N, Mercier FJ, et al. European minimum standards for obstetric analgesia and anaesthesia departments: an experts’ consensus. Eur J Anaesthesiol 2020; 37: 1115–25. https://doi.org/10.1097/eja.0000000000001362
Gelb AW, Morriss WW, Johnson W, Merry AF, International Standards for a Safe Practice of Anesthesia Workgroup. World Health Organization-World Federation of Societies of Anaesthesiologists (WHO-WFSA) international standards for a safe practice of anesthesia. Can J Anesth 2018; 65: 698–708. https://doi.org/10.1007/s12630-018-1111-5
Juang J, Gabriel RA, Dutton RP, Palanisamy A, Urman RD. Choice of anesthesia for Cesarean delivery: an analysis of the National Anesthesia Clinical Outcomes Registry. Anesth Analg 2017; 124: 1914–7. https://doi.org/10.1213/ane.0000000000001677
Palanisamy A, Mitani AA, Tsen LC. General anesthesia for Cesarean delivery at a tertiary care hospital from 2000 to 2005: a retrospective analysis and 10-year update. Int J Obstet Anesth 2011; 20: 10–6. https://doi.org/10.1016/j.ijoa.2010.07.002
Sumikura H. Keep our guard up against general anesthesia for Cesarean section. J Anesth 2012; 26: 324–5. https://doi.org/10.1007/s00540-012-1403-9
Sumikura H. When was the last time you induced general anesthesia for Cesarean section. J Anesth 2015; 29: 819–20. https://doi.org/10.1007/s00540-015-1985-0
Traynor AJ, Aragon M, Ghosh D, et al. Obstetric anesthesia workforce survey: a 30-year update. Anesth Analg 2016; 122: 1939–46. https://doi.org/10.1213/ane.0000000000001204
Yonekura H, Mazda Y, Noguchi S, Tsunobuchi H, Shimaoka M. Trend in neuraxial morphine use and postoperative analgesia after Cesarean delivery in Japan from 2005 to 2020. Sci Rep 2022; 12: 17234. https://doi.org/10.1038/s41598-022-22165-5
Naik BI, Kuck K, Saager L, et al. Practice patterns and variability in intraoperative opioid utilization: a report from the multicenter perioperative outcomes group. Anesth Analg 2022; 134: 8–17. https://doi.org/10.1213/ane.0000000000005663
Reed SE, Tan HS, Fuller ME, et al. Analgesia after Cesarean delivery in the United States 2008–2018: a retrospective cohort study. Anesth Analg 2021; 133: 1550–8. https://doi.org/10.1213/ane.0000000000005587
Butwick AJ, Palanisamy A. Mode of anaesthesia for Caesarean delivery and maternal morbidity: can we overcome confounding by indication. Br J Anaesth 2018; 120: 621–3. https://doi.org/10.1016/j.bja.2018.01.002
Japan Maternal Death Exploratory Committee. Annual report of JMDEC; recommendations for saving mothers [Japanese]. Available from URL: https://www.jaog.or.jp/wp/wp-content/uploads/2022/06/botai_2021.pdf (accessed July 2023).
Nagai K, Tanaka T, Kodaira N, Kimura S, Takahashi Y, Nakayama T. Data resource profile: JMDC claims database sourced from health insurance societies. J Gen Fam Med 2021; 22: 118–27. https://doi.org/10.1002/jgf2.422
Ikegami N, Yoo BK, Hashimoto H, et al. Japanese universal health coverage: evolution, achievements, and challenges. Lancet 2011; 378: 1106–15. https://doi.org/10.1016/s0140-6736(11)60828-3
Author contributions
Hiroshi Yonekura conceived and designed the study, analyzed the data, and wrote the manuscript. Yusuke Mazda and Shohei Noguchi contributed to the study design, data interpretation, and manuscript drafting. Hironaka Tsunobuchi and Koji Kawakami wrote and critically revised the manuscript.
Acknowledgements
This work was supported by JSPS KAKENHI (grant number: JP20K17834) and the Research Institute of Healthcare Data Science. The authors thank the staff at JMDC Co., Ltd, Tokyo, Japan, for assistance with data preparation. The authors also thank Editage (www.editage.jp) for English language editing.
Disclosures
Koji Kawakami received advisory fees from Shin Nippon Biomedical Laboratories, Ltd., Japan, JMDC Inc., Japan, LEBER Inc., and CICS, Japan; research funds from Eisai, Kyowa Kirin, and Real World Data, Co, Ltd, Japan; and held stock of Real World Data, Co., Ltd, Japan. Other authors have no direct or indirect conflicts of interest.
Funding statement
This study was funded by the Japan Society for the Promotion of Science and Grants-in-Aid for Scientific Research (grant number JP20K17834) and the Research Institute of Healthcare Data Science.
Prior conference presentations
This study was presented in part at the 69th Annual meeting of the Japanese Society of Anesthesiologists (16–18 June 2022, Kobe, Hyogo, Japan).
Data availability
Data are not publicly available. The data sets analyzed in this study are available from the corresponding author (HY) upon reasonable request.
Editorial responsibility
This submission was handled by Dr. Philip M. Jones, Deputy Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is accompanied by an Editorial. Please see Can J Anesth 2024; https://doi.org/10.1007/s12630-023-02634-9.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yonekura, H., Mazda, Y., Noguchi, S. et al. Anesthesia practice for Cesarean delivery in Japan: a retrospective cohort study. Can J Anesth/J Can Anesth 71, 175–186 (2024). https://doi.org/10.1007/s12630-023-02633-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-023-02633-w