Abstract
Objective
The aim of this study was to determine how gait speed and frontal lobe functionsin community-dwelling older adults in Korea.
Design
This was a cross-sectional study.
Setting
The study used data from the Korean Frailty and Aging Cohort Survey (KFACS), a multi-center longitudinal study addressing 10 centers across urban, rural, and suburban communities in Korea, between 2016 and 2017.
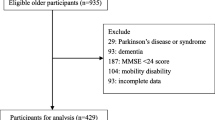
Participants
A total of 1552 older adults who underwent both gait speed tests and cognitive functions tests during the investigation of the KFACS.
Measurements
Gait speed was assessed by asking participants to walk from a starting point to a point 4 meters away at a normal gait. Cognitive functions were evaluated using various standardized cognitive functions tests.
Results
Gait speed was slower when participants were older or less educated The percentage of women, higher BMI, people with lower incomes, singles, smokers, and drinkers was high in the slower gait group. Also, all cognitive function scores were low and depression score was high in the group with slower walking speed. The slower walking speed showed low physical activity score and high prevalence of hypertension, osteoarthritis and osteoporosis. Among the seven cognitive functions (MMSE, memory, TMT, Recall, Recognition, digit span, and Fab), only TMT showed no significant difference between different gait speed groups. The other six cognitive functions showed higher results in the fastest gait speed group (T3), Participants in middle gait speed group (T2) also showed higher results in five of the seven cognitive function scores as well (Memory, Recall, Recognition, digit span, and Fab).
Conclusion
In this study, we found correlation between the slower gait speeds and the decrease in cognitive function, and especially the frontal lobe dysfunction was most prominent of all cognitive dysfunctions.
Similar content being viewed by others
References
Fritz NE, McCarthy CJ, Adamo DE. Handgrip strength as a means of monitoring progression of cognitive decline - A sco** review. Ageing research reviews. 2017;35:112–23.
Buracchio T, Dodge HH, Howieson D, Wasserman D, Kaye J. The trajectory of gait speed preceding mild cognitive impairment. Archives of neurology. 2010;67(8):980–6.
Kikkert LHJ, Vuillerme N, van Campen JP, Hortobagyi T, Lamoth CJ. Walking ability to predict future cognitive decline in old adults: A sco** review. Ageing research reviews. 2016;27:1–14.
Hawkins KA, Fox EJ, Daly JJ, Rose DK, Christou EA, McGuirk TE, et al. Prefrontal over-activation during walking in people with mobility deficits: Interpretation and functional implications. Human movement science. 2018;59:46–55.
Bloem BR, Gussekloo J, Lagaay AM, Remarque EJ, Haan J, Westendorp RGJ. Idiopathic Senile Gait Disorders Are Signs of Subclinical Disease. Journal of the American Geriatrics Society. 2000;48(9):1098–101.
Beurskens R, Helmich I, Rein R, Bock O. Age-related changes in prefrontal activity during walking in dual-task situations: a fNIRS study. International journal of psychophysiology: official journal of the International Organization of Psychophysiology. 2014;92(3):122–8.
Cedervall Y, Halvorsen K, Aberg AC. A longitudinal study of gait function and characteristics of gait disturbance in individuals with Alzheimer’s disease. Gait & posture. 2014;39(4):1022–7.
Kim S, Won CW, Kim BS, Kim S, Yoo J, Byun S, et al. EuroQol Visual Analogue Scale (EQ-VAS) as a Predicting Tool for Frailty in Older Korean Adults: The Korean Frailty and Aging Cohort Study (KFACS). The journal of nutrition, health & aging. 2018;22(10):1275–80.
Verghese J, Robbins M, Holtzer R, Zimmerman M, Wang C, Xue X, et al. Gait dysfunction in mild cognitive impairment syndromes. J Am Geriatr Soc. 2008;56(7):1244–51.
Liu-Ambrose T, Ahamed Y, Graf P, Feldman F, Robinovitch SN. Older fallers with poor working memory overestimate their postural limits. Archives of physical medicine and rehabilitation. 2008;89(7):1335–40.
Mirelman A, Maidan I, Bernad-Elazari H, Nieuwhof F, Reelick M, Giladi N, et al. Increased frontal brain activation during walking while dual tasking: an fNIRS study in healthy young adults. Journal of NeuroEngineering and Rehabilitation. 2014;11(1):85.
Morris R, Lord S, Bunce J, Burn D, Rochester L. Gait and cognition: Map** the global and discrete relationships in ageing and neurodegenerative disease. Neuroscience and biobehavioral reviews. 2016;64:326–45.
Snijders AH, van de Warrenburg BP, Giladi N, Bloem BR. Neurological gait disorders in elderly people: clinical approach and classification. The Lancet Neurology. 2007;6(1):63–74.
Ojagbemi A, D’Este C, Verdes E, Chatterji S, Gureje O. Gait speed and cognitive decline over 2 years in the Ibadan study of aging. Gait & posture. 2015;41(2):736–40.
Stuss DT, Alexander MP. Executive functions and the frontal lobes: a conceptual view. Psychological research. 2000;63(3–4):289–98.
Valkanova V, Ebmeier KP. What can gait tell us about dementia? Review of epidemiological and neuropsychological evidence. Gait & posture. 2017;53:215–23.
Tian Q, Chastan N, Bair WN, Resnick SM, Ferrucci L, Studenski SA. The brain map of gait variability in aging, cognitive impairment and dementia-A systematic review. Neuroscience and biobehavioral reviews. 2017;74(Pt A):149–62.
Silder A, Delp SL, Besier T. Men and women adopt similar walking mechanics and muscle activation patterns during load carriage. Journal of biomechanics. 2013;46(14):2522–8.
Acknowledgement
This research was supported by a grant of the Korea Health Technology R&D Project through the Korean Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare, Republic of Korea (grant number:HI15C3153).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest: Dr. Seo has nothing to disclose
Ethical standards: All parties involved in the act of publishing in The Journal of Nursing Home Research including the author, the journal editor, the peer reviewer and the publisher agree upon standards of expected ethical behavior.
Rights and permissions
About this article
Cite this article
Seo, M., Won, C.W., Kim, S. et al. The Association of Gait Speed and Frontal Lobe among Various Cognitive Domains: The Korean Frailty and Aging Cohort Study (KFACS). J Nutr Health Aging 24, 91–97 (2020). https://doi.org/10.1007/s12603-019-1276-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-019-1276-9