Abstract
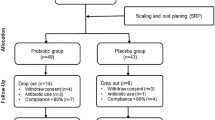
A specific strain of naturally occurring oral lactobacilli was isolated and identified based on morphological, biochemical, and 16S rRNA gene sequencing. The phylogenetic affiliation of the isolate confirmed that the NK02 strain had close association with the Lactobacillus salivarius. An effective mouthwash was developed for treatment of periodontitis and suppression of the indicator bacterium Aggregatibacter actinomycetemcomitans which is an obvious pathogen of periodontal disease. The mouthwash containing L. salivarius NK02 was tested at a dose level of 108 (colony forming units (CFU) ml−1), monitoring over a period of 4 weeks. The study was a randomized double-blind placebo control trial, and the patients were treated in two groups of control and test by using scaling and root planing (SRP) + placebo and scaling and root planing (SRP) + probiotic, respectively. It appeared that the probiotic mouthwash was able to inhibit the bacterial growth on both saliva and sub-gingival crevice and exhibited antibacterial activity against A. actinomycetemcomitans. The results also showed that SRP+ probiotic treatment led to a significant decrease of gingival index (GI) and bleeding on probing (BOP) compared with that of SRP + placebo for the probiotic group. The rate of decrease in pocket depth was displayed in the group with SRP + probiotic treatment equal to 1/2 mm, and probing pocket depth (PPD) value was decreased in the probiotic bacteria treatment group that can explain the decrease in inflammation in gingiva. Our findings suggest that probiotic mouthwash is healthy for daily use as an alternative for maintaining dental and periodontal health.



Similar content being viewed by others
References
Castiblanco GA, Yucel-Lindberg T, Roos S, Twetman S (2016) Effect of Lactobacillus reuteri on cell viability and PGE2 production in human gingival fibroblasts. Probiotics Antimicro Prot. doi:10.1007/s12602-016-9246-6
Sharif MR, Haddad-Kashani H, Taghavi-Ardakani A, Kheirkhah D, Tabatabaei F, Sharif A (2016) The effect of a yeast probiotic on acute diarrhea in children. Probiotics Antimicro Prot 8:211–214
Gillian H, Lee M, McGrath C, Yiu CKY (2016) Evaluating the impact of caries prevention and management by caries risk assessment guidelines on clinical practice in a dental teaching hospital. BMC Oral Health 16:58
Meurman JH (2005) Probiotics: do they have a role in oral medicine and dentistry? Eur J Oral Sci 113:188–196
Newman MG, Takei H, Klokkevold PR, Carranza F (2015) Carranza clinical periodontology. 12th edition, Elsevier
Kumar SK, Leys EJ, Bryk JM, Martinez FJ, Moeschberger ML, Griffen AL (2006) Changes in periodontal health status are associated with bacterial community shifts as assessed by quantitative 16S cloning and sequencing. J Clin Microbiol 44:3665–3673
Rylev M, Kilian M (2008) Prevalence and distribution of principal periodontal pathogens worldwide. J Clin Periodontol 35:346–361
Reddy MS, Babu MN (2011) How beneficial is bacterial prophylaxis to periodontal health? J Investig Clin Dent 2:95–101
Henderson B, Ward JM, Ready D (2010) Aggregatibacter (Actinobacillus) actinomycetemcomitans: a triple A* periodontopathogen. Periodontol 54:78–105
Haukioja JH, Stamatova I (2007) Probiotics: contributions to oral health. Oral dis 13:443–451
Koll-Klais P, Mandar R, Leibur E, Mikelsaar M (2005) Oral microbial ecology in chronic periodontitis and periodontal health. Microbial Ecol Health Dis 17:146–155
Sookhee S, Chulasiri M, Prachyabrued W (2001) Lactic acid bacteria from healthy oral cavity of Thai volunteers: inhibition of oral pathogens. J Appl Microbiol 90:172–179
Tsuzukibashi O, Takada K, Saito M, Kimura C, Yoshikawa T, Makimura M, Hirasawa M (2008) A novel selective medium for isolation of Aggregatibacter (Actinobacillus) actinomycetemcomitans. J Periodontal Res 43:544–548
Heilig HGHJ, Zoetendal EG, Vaughan EE, Marteau P, Akkermans ADL, de Vos WM (2002) Molecular diversity of Lactobacillus spp. and other lactic acid bacteria in the human intestine as determined by specific amplification of 16S ribosomal DNA. Appl Environ Microbiol 68:114–123
Tamura K, Stecher G, Peterson D, Filipski A, Kumar S (2013) MEGA6: molecular evolutionary genetics analysis version 6.0. Mol Biol Evol 30:2725–2729
Singhal K, Joshi H, Chaudhary BL (2010) Bile and acid tolerance ability of probiotic Lactobacillus strains. J Global Pharma Tech 2:17–25
Vinderola CG, Reinheimer JA (2000) Enumeration of Lactobacillus casei in the presence of L. acidophilus, bifidobacteria and lactic starter bacteria in fermented dairy products. Int Dairy J 4:271–275
Dashkevicz MP, Feighner SD (1989) Development of a differential medium for bile salt hydrolase-active Lactobacillus spp. Appl Environ Microbiol 55:11–16
Blanquet S, Zeijdner E, Beyssac E, Meunier JP, Denis S, Havenaar R, Alric M (2004) A dynamic artificial gastrointestinal system for studying the behavior of orally administered drug dosage forms under various physiological conditions. Pharm res 21:585–591
Vizoso-Pinto MG, Franz CM, Schillinger U, Holzapfel WH (2006) Lactobacillus spp. with in vitro probiotic properties from human faeces and traditional fermented products. Int J Food Microbiol 109:205–214
Clinical and Laboratory Standard Institute (CLSI) (2010). Performance Standards for Antimicrobial Susceptibility testing; 20th Informational Supplement CLSI document M100-S20-U. Wayne, PA
Loe H, Silness J (1963) Periodontal disease in pregnancy I. Prevalence and severity. Acta Odontol Scand 21:533–551
Ainamo J, Bay I (1975) Problems and proposals for recording gingivitis and plaque. Int Dent J 25:229–235
Corzo G, Gilliland SE (1999) Bile salt hydrolase activity of three strains of Lactobacillus acidophilus. J Dairy Sci 82:472–480
Candela M, Perna F, Carnevali P, Vitali B, Ciati R, Giochetti P, Rizzello F, Campieri MP (2008) Interaction of probiotic Lactobacillus and Bifidobacterium strains with human intestinal epithelial cells: adhesion properties, competition against enteropathogens and modulation of IL-8 production. Int J Food Microbiol 125:286–292
De Smet I, Hoorde LV, Woestyne MV, Christiaens H, Verstraete W (1995) Significance of bile salt hydrolytic activities of lactobacilli. J Appl Bacteriol 29:292–301
Mathara JM, Schillinger U, Kutima PM, Mbugua SK, Guigas C, Franz C, Holzapfel WH (2008) Functional properties of Lactobacillus plantarum strains isolated from Maasai traditional fermented milk products in Kenya. Curr Microbiol 56:315–321
Marteau P, Minekus M, Havenaar R, Huis In’t Veld JH (1997) Survival of lactic acid bacteria in a dynamic model of the stomach and small intestine: validation and the effects of bile. J Dairy Sci 80:1031–1037
Krass P, Carlsson B, Dahl C, Paulsson A, Nilsson A, Sinkiewicz G (2006) Decreased gum bleeding and reduced gingivitis by probiotic Lactobacillus reuteri. Swed Dent J 30:55–60
Vivekananda MR, Vandana KL, Bhat KG (2010) Effect of probiotic Lactobacillus reuteri (Prodentis) in the management of periodontal disease: a preliminary randomized clinical trial. J Oral Microbiol 2:5344. doi:10.3402/jom.v2i0.5344
Twetman S, Derawi B, Keller M, Ekstrand K, Yucel-Lindberg T, Stecksen-Blicks C (2009) Short–term effect of chewing gums containing Lactobacillus reuteri on the level of inflammatory mediators in gingival crevicular fluid. Acta Odontol Scand 67:19–24
Shimauchi H, Mayanagi G, Nakaya S (2008) Improvement of periodontal condition by probiotics with Lactobacillus salivarius WB21: a randomized double blind placebo controlled study. J Clin Periodontol 10:897–905
Amornchat C, Rassameemasmaung S, Sirpairojthikoon W, Swasdison S (2003) Invasion of Porphyromonas gingivalis into human gingival fibroblasts in vitro. J Int Acad Periodontol 5:98–105
Socransky SS, Haffajee AD, Cuqini MA, Smith C, Kent RL Jr (1998) Microbial complexes in subgingival plaque. J Clinc Periodontol 25:134–144
Mousques T, Listgarten MA, Philips RW (1980) Effect of scaling and root planing on the composition of the human subgingival microbial flora. J Periodontol res 15:144–151
Ishikawa H, Aiba Y, Nakanishi M, Oh-hashi Y, Koga Y (2003) Suppression of periodontal pathogenic bacteria in the saliva of humans by the adminstration of Lactobacillus salivarius TI2711. J Jpn Soc Periodontol 45:105–112
Matsouka T, Sugano N, Takigawa S, Takane M, Yoshimura N, Ito K (2006) Effect of oral Lactobacillus salivarius TI 2711 (LS1) administration on periodontal pathogenic bacteria in subgingival plaque. J Jpn Soc Periodontol 48:315–324
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
The study was autonomously reviewed and approved by the ethics committee of Tehran University of Medical Sciences, the review board. Our clinical trial was registered in IRCT and allocated a unique code as follows: IRCT201201258825N1.
Funding
The current work was supported by the National Institute of Genetic Engineering and Biotechnology (NIGEB), affiliated to the Ministry of Science, Research & Technology (IMSRT), Iran.
Competing Interests
The authors declare that they have no competing interests.
Informed Consent
The present study was conducted in full accordance with the World Medical Association Declaration of Helsinki and a written consent form signed by all the subjects or the parents in case the participants were under 18.
Rights and permissions
About this article
Cite this article
Sajedinejad, N., Paknejad, M., Houshmand, B. et al. Lactobacillus salivarius NK02: a Potent Probiotic for Clinical Application in Mouthwash. Probiotics & Antimicro. Prot. 10, 485–495 (2018). https://doi.org/10.1007/s12602-017-9296-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12602-017-9296-4