Abstract
Background
Loneliness is a growing public health concern associated with substantial negative mental and physical health outcomes. Loneliness is especially relevant for individuals with a chronic illness, perhaps more so if their illness is rare. Little is known about the psychosocial experience of individuals with a rare chronic illness, and whether and how it may differ from the experience of individuals with common chronic illnesses. We compared the magnitude of loneliness in persons with a rare or common chronic illness and examined theoretically guided predictors of loneliness as follows: stigma, illness intrusiveness, social comparison, social support, support from healthcare providers, and self-efficacy.
Method
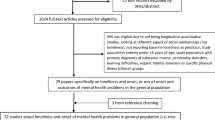
Individuals with a chronic illness (common or rare) completed an anonymous online survey (N = 952).
Results
Individuals with common chronic illnesses were as lonely as those with a rare chronic illness. Loneliness in both groups was higher than that in population norms. Regression analyses reveal that independent of other predictors, loneliness was especially high among people who feel stigmatized by others, those who have less social support available, and people whose functioning is more disrupted by their illness (all p values < 0.01).
Conclusion
The similarity of loneliness in these groups reinforces the value of further systematic research to identify the needs of individuals with any type of chronic illness. Study findings highlight the importance of examining internalized stigma and social support as possible targets of intervention to reduce loneliness among individuals with a chronic illness, recognizing some of the unique features and challenges of their disorders, whether common or rare.
Similar content being viewed by others
Data Availability
Data is available upon written request to the corresponding author.
References
Cacioppo JT, Cacioppo S. The growing problem of loneliness. The Lancet. 2018;391.
Wilson C, Moulton B. Loneliness among older adults: a national survey of adults 45+. AARP The Magazine. 2010.
Musich S, Wang SS, Hawkins K, Yeh CS. The impact of loneliness on quality of life and patient satisfaction among older, sicker adults. Gerontol Geriatr Med. 2015. https://doi.org/10.1177/2333721415582119.
Donovan NJ, Blazer D. Social isolation and loneliness in older adults: review and commentary of a national academies report. Am J Geriatr Psychiatry. 2020;28. https://doi.org/10.1016/j.jagp.2020.08.005.
Cacioppo JT, Hughes ME, Waite LJ, et al. Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychol Aging. 2006;21. https://doi.org/10.1037/0882-7974.21.1.140.
Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychol Aging. 2010;25. https://doi.org/10.1037/a0017216.
Bower JE, Shiao SL, Sullivan P, et al. Prometastatic molecular profiles in breast tumors from socially isolated women. JNCI Cancer Spectr. 2018;2. https://doi.org/10.1093/jncics/pky029.
Lutgendorf SK, Penedo F, Goodheart MJ, et al. Epithelial-mesenchymal transition polarization in ovarian carcinomas from patients with high social isolation. Cancer. 2020;126. https://doi.org/10.1002/cncr.33060.
Lutgendorf SK, Andersen BL. Biobehavioral approaches to cancer progression and survival: mechanisms and interventions. Am Psychol. 2015;70. https://doi.org/10.1037/a0035730.
Cacioppo JT, Hawkley LC. Perceived social isolation and cognition. Trends Cogn Sci. 2009;13.
Holt-Lunstad J, Smith TB, Baker M, et al. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10. https://doi.org/10.1177/1745691614568352.
Cole SW, Hawkley LC, Arevalo JM, et al. Social regulation of gene expression in human leukocytes. Genome Biol. 2007;8. https://doi.org/10.1186/gb-2007-8-9-r189.
Cole SW, Capitanio JP, Chun K, et al. Myeloid differentiation architecture of leukocyte transcriptome dynamics in perceived social isolation. Proc Natl Acad Sci USA. 2015;112. https://doi.org/10.1073/pnas.1514249112.
Cole SW, Hawkley LC, Arevalo JMG, Cacioppo JT. Transcript origin analysis identifies antigen-presenting cells as primary targets of socially regulated gene expression in leukocytes. Proc Natl Acad Sci USA. 2011;108. https://doi.org/10.1073/pnas.1014218108.
Robles TF, Kiecolt-Glaser JK. The physiology of marriage: pathways to health. In: Physiol Behav. 2003.
Uchino BN. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J Behav Med. 2006;29.
Moieni M, Irwin MR, Jevtic I et al. Trait sensitivity to social disconnection enhances pro-inflammatory responses to a randomized controlled trial of endotoxin. Psychoneuroendocrinology. 2015;62. https://doi.org/10.1016/j.psyneuen.2015.08.020.
DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol. 2004;23.
DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42.
Shankar A, Hamer M, McMunn A, Steptoe A. Social isolation and loneliness: relationships with cognitive function during 4 years of follow-up in the English longitudinal study of ageing. Psychosom Med. 2013;75. https://doi.org/10.1097/PSY.0b013e31827f09cd.
Centers for Disease Control and Prevention National Center for Chronic Disease Prevention and Health Promotion. Chronic diseases in America. 2022. https://www.cdc.gov/chronicdisease/resources/infographic/chronic-diseases.htm. Accessed 2 Apr 2023.
Stanton AL, Revenson TA, Tennen H. Health psychology: psychological adjustment to chronic disease. Annu Rev Psychol. 2007;58. https://doi.org/10.1146/annurev.psych.58.110405.085615.
von der Lippe C, Diesen PS, Feragen KB. Living with a rare disorder: a systematic review of the qualitative literature. Mol Genet Genomic Med. 2017;5.
Alsheikh M, Shukla V, Seoane-Vazquez E. Trends in approval of advanced therapy medicinal products approved by the US Food and Drug Administration. Value in Health. 2018;21. https://doi.org/10.1016/j.jval.2018.04.1739.
Graf von der Schulenburg JM, Frank M. Rare is frequent and frequent is costly: rare diseases as a challenge for health care systems. Eur J Health Econ. 2015;16.
Åsbring P, Närvänen A-L. Women’s experiences of stigma in relation to chronic fatigue syndrome and fibromyalgia. Qual Health Res. 2002;12:148–60. https://doi.org/10.1177/104973230201200202.
Looper KJ, Kirmayer LJ. Perceived stigma in functional somatic syndromes and comparable medical conditions. J Psychosom Res. 2004;57:373–8. https://doi.org/10.1016/j.jpsychores.2004.03.005.
Jacoby A, Austin JK. Social stigma for adults and children with epilepsy. Epilepsia. 2007;48:6–9. https://doi.org/10.1111/j.1528-1167.2007.01391.x.
Chapple A, Ziebland S, McPherson A. Stigma, shame, and blame experienced by patients with lung cancer: qualitative study. BMJ. 2004;328:1470. https://doi.org/10.1136/bmj.38111.639734.7C.
Earnshaw VA, Quinn DM, Park CL. Anticipated stigma and quality of life among people living with chronic illnesses. Chronic Illn. 2012;8. https://doi.org/10.1177/1742395311429393.
Cohen S. Social relationships and health. Am Psychol. 2004;59.
Baumeister RF, Leary MR. The need to belong: desire for interpersonal attachments as a fundamental human motivation. Psychol Bull. 1995;117. https://doi.org/10.1037/0033-2909.117.3.497.
Taylor SE, Brown JD. Illusion and well-being: a social psychological perspective on mental health. Psychol Bull. 1988;103. https://doi.org/10.1037/0033-2909.103.2.193.
Levy RL. Social support and compliance: a selective review and critique of treatment integrity and outcome measurement. Soc Sci Med. 1983;17. https://doi.org/10.1016/0277-9536(83)90192-2.
Mitchell RE, Billings AG, Moos RH. Social support and well-being: implications for prevention programs. J Prim Prev. 1982;3. https://doi.org/10.1007/BF01324668.
Holt-Lunstad J, Robles TF, Sbarra DA. Advancing social connection as a public health priority in the United States. Am Psychol. 2017;72. https://doi.org/10.1037/amp0000103.
Robles TF, Slatcher RB, Trombello JM, McGinn MM. Marital quality and health: a meta-analytic review. Psychol Bull. 2014;140. https://doi.org/10.1037/a0031859.
Walter S, Hrabal V, Kahle J, et al. Partnership and emotional support in the doctor-patient relationship. Dtsch Arztebl Int. 2021. https://doi.org/10.3238/arztebl.m2021.0173.
Taylor SE, Lobel M. Social comparison activity under threat: downward evaluation and upward contacts. Psychol Rev. 1989;96. https://doi.org/10.1037/0033-295X.96.4.569.
Festinger L. A theory of social comparison processes. Hum Relat. 1954;7. https://doi.org/10.1177/001872675400700202.
Arigo D, Suls JM, Smyth JM. Social comparisons and chronic illness: research synthesis and clinical implications. Health Psychol Rev. 2014;8. https://doi.org/10.1080/17437199.2011.634572.
Wills TA. Downward comparison principles in social psychology. Psychol Bull. 1981;90. https://doi.org/10.1037/0033-2909.90.2.245.
Bandura A. Self-efficacy: the exercise of control. New York: W.H. Freeman and Company. Am Psychol Assoc. 1997;23.
Bandura A, Watts RE. Self-efficacy in changing societies. J Cogn Psychother. 1996;10. https://doi.org/10.1891/0889-8391.10.4.313.
Fry PS, Debats DL. Self-efficacy beliefs as predictors of loneliness and psychological distress in older adults. Int J Aging Hum Dev. 2002;55. https://doi.org/10.2190/KBVP-L2TE-2ERY-BH26.
Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40. https://doi.org/10.1007/s12160-010-9210-8.
Edwards R, Telfair J, Cecil H, Lenoci J. Self-efficacy as a predictor of adult adjustment to sickle cell disease: one-year outcomes. Psychosom Med. 2001;63. https://doi.org/10.1097/00006842-200109000-00020.
Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. J Am Med Assoc. 2002;288
Kohler CL, Fish L, Greene PG. The relationship of perceived self-efficacy to quality of life in chronic obstructive pulmonary disease. Health Psychol. 2002;21. https://doi.org/10.1037/0278-6133.21.6.610.
Molina Y, Choi SW, Cella D, Rao D. The Stigma Scale for Chronic Illnesses 8-item version (SSCI-8): development, validation and use across neurological conditions. Int J Behav Med. 2013;20. https://doi.org/10.1007/s12529-012-9243-4.
Corrigan PW, Penn DL. Lessons from social psychology on discrediting psychiatric stigma. Am Psychol. 1999;54. https://doi.org/10.1037/0003-066X.54.9.765.
Corrigan PW, Watson AC, Barr L. The self-stigma of mental illness: implications for self-esteem and self-efficacy. J Soc Clin Psychol. 2006;25. https://doi.org/10.1521/jscp.2006.25.8.875.
Rao D, Desmond M, Andrasik M, et al. Feasibility, acceptability, and preliminary efficacy of the unity workshop: an internalized stigma reduction intervention for African American women living with HIV. AIDS Patient Care STDS. 2012;26. https://doi.org/10.1089/apc.2012.0106.
Devins GM. Illness intrusiveness and the psychosocial impact of lifestyle disruptions in chronic life-threatening disease. Adv Ren Replace Ther. 1994;1. https://doi.org/10.1016/S1073-4449(12)80007-0.
Devins GM, Binik YM, Hutchinson TA, et al. The emotional impact of end-stage renal disease: importance of patients’ perceptions of intrusiveness and control. Int J Psychiatry Med. 1983;13. https://doi.org/10.2190/5dcp-25bv-u1g9-9g7c.
Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32. https://doi.org/10.1016/0277-9536(91)90150-B.
Lorig KR, Sobel DS, Ritter PL, et al. Effect of a self-management program on patients with chronic disease. Eff Clin Pract. 2001;4.
Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys. Res Aging. 2004;26. https://doi.org/10.1177/0164027504268574.
Russell D, Peplau LA, Cutrona CE. The revised UCLA Loneliness Scale: concurrent and discriminant validity evidence. J Pers Soc Psychol. 1980;39. https://doi.org/10.1037/0022-3514.39.3.472.
Pinquart M, Sörensen S. Influences on loneliness in older adults: a meta-analysis. Basic Appl Soc Psych. 2001;23. https://doi.org/10.1207/S15324834BASP2304_2.
Earnshaw VA, Watson RJ, Eaton LA, et al. Integrating time into stigma and health research. Nat Rev Psychol. 2022;1. https://doi.org/10.1038/s44159-022-00034-2.
Bandura A. Perceived self-efficacy in cognitive development and functioning. Educ Psychol. 1993;28. https://doi.org/10.1207/s15326985ep2802_3.
Meichenbaum D. A clinical handbook/practical therapist manual for assessing and treating adults with post-traumatic stress disorder (PTSD). Institute Press. 1994.
Masi CM, Chen HY, Hawkley LC, Cacioppo JT. A meta-analysis of interventions to reduce loneliness. Pers Soc Psychol Rev. 2011;15.
O’Rourke HM, Collins L, Sidani S. Interventions to address social connectedness and loneliness for older adults: a sco** review. BMC Geriatr. 2018;18.
Barrera M, Prelow. H Interventions to promote social support in children and adolescents. In: D CJRISRPW (ed) The promotion of wellness in children and adolescents. Child Welfare League of America. 309–339.
Gottlieb BH. Selecting and planning support interventions. In: Social support measurement and intervention. Oxford University Press. 2000;195–220.
Heller K, Price RH, Hogg JR. The role of social support in community and clinical interventions. In: Sarason BR, Sarason IG, Pierce GR, editors. Social support: an interactional view. John Wiley & Sons; 1990. p. 482–507.
Vaux A. Social support: theory, research, and intervention. Praeger Publishers; 1988.
Madara E. The mutual-aid self-help online revolution. Soc Policy. 1997;27.
Weinberg N, Schmale JD, Uken J, Wessel K. Computer-mediated support groups Soc Work Groups. 1995;17:43–54. https://doi.org/10.1300/J009v17n04_04.
Bogat G, Sullivan L, Grober J. Applications of social support to preventive interventions. In: D. S. Glenwick, L. A. Jason (eds) Promoting health and mental health in children, youth, and families. 1993. p. 205–232.
Mak WWS, Mo PKH, Ma GYK, Lam MYY. Meta-analysis and systematic review of studies on the effectiveness of HIV stigma reduction programs. Soc Sci Med. 2017;188.
Heijnders M, Van Der Meij S. The fight against stigma: an overview of stigma-reduction strategies and interventions. Psychol Health Med. 2006;11.
Acknowledgements
Jennifer Nicoloro-SantaBarbara received support from Harvard Medical School’s Kaplen Fellowship in Depression during preparation of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval and Consent to Participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nicoloro-SantaBarbara, J., Lobel, M. Loneliness and Its Predictors in Rare Versus Common Chronic Illnesses. Int.J. Behav. Med. 31, 422–432 (2024). https://doi.org/10.1007/s12529-023-10231-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-023-10231-9