Abstract
Introduction
This study evaluated 7-year effectiveness and safety of second-generation trabecular micro-bypass implantation (iStent inject) either in combination with cataract surgery or as a standalone procedure (Combined or Standalone subgroups, respectively) in eyes with open-angle glaucoma.
Methods
This prospective, non-randomized, unmasked, longitudinal study included 125 consecutive iStent inject cases of a single surgeon at a large German academic hospital. Patients had considerable preoperative disease burden, with mean intraocular pressure (IOP) of 23.5 mmHg, 84.8% of eyes on ≥ 2 medications, and 38.4% of eyes with prior glaucoma surgery. IOP, medications, adverse events, and secondary surgeries were assessed through 7 years in the Overall cohort and in Combined (n = 81) and Standalone (n = 44) subgroups.
Results
Over 7-year follow-up, mean IOP decreased by 36.2–40.0% in Overall eyes, 34.1–38.9% in Combined eyes, and 39.5–43.5% in Standalone eyes (p < 0.001 at all timepoints for all groups). Meanwhile, mean medications decreased by 59.3–71.3% in Overall eyes, 57.9–69.0% in Combined eyes, and 62.1–76.2% in Standalone eyes (p < 0.001 at all timepoints in all groups). At last follow-up (mean 77.4 months; 92.8% of patients with last visit at 6 or 7 years), 83.7% of Overall eyes, 82.3% of Combined eyes, and 86.4% of Standalone eyes had achieved ≥ 20% IOP reduction vs preoperative. At last follow-up vs preoperative, 100% of eyes in all groups had the same or lower IOP and 100% had the same or lower medication regimen. Safety outcomes were favorable, with no filtration surgeries and only 4.84% of eyes experiencing clinically significant visual field loss over 7 years of follow-up.
Conclusion
iStent inject implantation with or without phacoemulsification produced significant and durable 7-year reductions in IOP (~ 34–44% reduction) and medications (~ 58–76% reduction) while preventing filtering surgery in this cohort of patients with relatively high preoperative disease burden. Combined and Standalone cases had similarly favorable effectiveness and safety.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Safe and efficacious long-term surgical treatments are needed to prevent or minimize vision loss from glaucoma, a major cause of global blindness. |
This prospective study assessed real-world 7-year outcomes following implantation of two second-generation trabecular micro-bypass stents either with or without cataract surgery in eyes with mild to severe open-angle glaucoma. |
The study hypothesized that this surgical intervention could effectively and safely reduce intraocular pressure (IOP) and medication burden over the long term in these glaucomatous eyes, with favorable safety outcomes (including low incidence of clinically significant visual field loss). |
What was learned from the study? |
The data demonstrated substantial 7-year reductions in IOP and medications, along with favorable safety and visual field outcomes, in eyes with a considerable preoperative medication burden and glaucoma surgical history. Results were similarly favorable in combined and standalone usage. |
Drawing upon long-term, clinically heterogeneous, real-world patient data, this study provides directly relevant information for clinicians and patients evaluating glaucoma treatment options. |
Introduction
Over the past 2 decades, glaucoma has increasingly become a surgical disease. As more minimally invasive, lower-risk procedures have proliferated, the question of a surgical versus topical medical intervention has shifted to earlier in the overall treatment algorithm. Studies like the LIGHT trial [1] have placed selective laser trabeculoplasty (SLT) as a recommended initial treatment option for newly diagnosed glaucoma; micro-invasive glaucoma surgeries (MIGS) are also increasingly being considered as alternatives to topical medications [2, 3] because of the well-known limitations of topical medications (e.g., poor compliance, ocular and systemic reactions, intraocular pressure (IOP) fluctuations, increased risk of filtering surgery failure, and diminished quality of life) [3,4,5,6,7,8]. This shift to a more proactive, rather than reactive, approach has been referred to as “interventional glaucoma” [9].
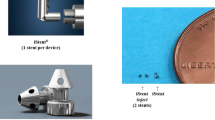
Among implantable MIGS devices, the longest term and broadest evidence base appears to come from the first-generation iStent and second-generation iStent inject trabecular micro-bypass devices (Glaukos Corp., Aliso Viejo, CA) [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48], with publications extending through 8 years and 5 years, respectively. Studies have evaluated the stents in a variety of glaucoma subtypes, severities, races, and countries. The present real-world 125-patient cohort was previously evaluated at 3 years [11, 12] and 5 years [13] following iStent inject implantation with or without phacoemulsification. At 5 years postoperatively, significant IOP and medication reductions were observed (40% and 71%, respectively), with favorable safety including no secondary filtration surgeries and documented stability of structural parameters [13].
In the present report, we provide effectiveness and safety data through 7 years postoperatively in this single prospective group of patients. To our knowledge, this is the longest term iStent inject study in the published literature to date. It includes cases completed in combination with cataract surgery or as a sole procedure, allowing us to isolate the impact of the stents alone, and it draws from the surgeon’s actual clinical population, including various glaucoma subtypes and a range of surgical histories (from surgery-naïve to failed trabeculectomy). These attributes, along with the prospective design and relatively high 7-year accountability, help make the dataset broadly relevant to practicing surgeons today.
Methods
Study Design and Participants
This was a prospective, consecutive, single-site study of patients who received iStent inject trabecular micro-bypass with or without cataract surgery and were followed for up to 7 years postoperatively. Surgeries were performed by one glaucoma specialist from May 2013 to February 2016 at a large academic eye hospital. Inclusion criteria consisted of a diagnosis of glaucoma [including primary open-angle glaucoma (POAG), pseudoexfoliative glaucoma (PXG), combined-mechanism glaucoma (CMG), pigmentary glaucoma (PG), or secondary (neovascular) glaucoma]; treatment with glaucoma medication(s) and/or prior glaucoma surgeries; eligibility for cataract surgery (for the Combined subgroup); and a documented need for further IOP and/or medication reduction. Patients were excluded if they were < 18 years of age or pregnant, or if they had angle-closure glaucoma, congenital glaucoma, ocular inflammation, or corneal opacities impacting gonioscopy. No formal sample size calculation was completed in this real-world consecutive clinical study. Study visits were completed at the following timepoints: preoperative, Day 1, Week 1, and Months 1, 3, 6, 12, 24, 26, 48, 60, 72, and 84. Ethics approval was obtained from the institutional review board (IRB) of the University of Heidelberg (IRB reference #S-482/2012). The study abided by the tenets of the Declaration of Helsinki, and all participants provided informed consent for surgery and participation.
Study Outcomes and Data Analysis
Efficacy outcomes consisted of mean IOP (measured by Goldmann applanation) and medication burden; proportion of eyes achieving a ≥ 20% IOP reduction from preoperative; IOP of ≤ 18 mmHg and ≤ 15 mmHg; same or lower IOP and medication burden vs preoperative; and treatment with 0 or ≥ 3 medications. Preoperative IOP was based on readings at two or more preoperative visits, while postoperative IOP was based on three IOP readings completed at each visit. Safety was characterized in terms of intraoperative complications, secondary glaucoma procedures (laser or incisional), and proportion of eyes with filtering surgery specifically (e.g., trabeculectomy or tube shunt). In addition, the percentage of eyes with clinically significant visual field mean deviation (VF MD) progression at 7 years versus preoperative was calculated. This was defined as VF MD loss ≥ 2.5 dB, as this is a standard adverse event threshold utilized in trabecular bypass MIGS pivotal trials [14, 49, 50].
Outcomes were analyzed via paired t tests (for continuous variables such as mean IOP and medications) or chi-square test (for categorical variables such as proportional outcomes of IOP threshold and medication burden). For mean IOP and medications over time, data from all available eyes at each timepoint were presented. For proportional outcomes, a last follow-up analysis (LFU) was completed for all patients with ≥ 1 month follow-up, with the final visit occurring at 6 or 7 years postoperatively for 93% (116/125) of patients. Results were calculated for the Overall cohort as well as for the Combined and Standalone subgroups.
iStent inject Device and Surgical Technique
As was described in the pivotal trial publication by Samuelson et al. [14], iStent inject trabecular micro-bypass consists of two titanium stents on a single injector, with each stent having 230 µm diameter, 360 µm height, and 80 µm central lumen diameter. Despite the micro-scale dimensions (approximately the size of the period on this page), each stent is known to be able to handle the entire aqueous outflow production of the human eye (up to 2.5 µl/min on average) [15]. In the present study, the iStent inject stents were implanted either after cataract surgery or as a standalone procedure. In either case, the stents were inserted ab internally 2–3 clock-hours apart through the trabecular meshwork into Schlemm’s canal, which facilitates up to 6 total clock-hours of outflow [16]. After implantation, stent positioning was confirmed gonioscopically, viscoelastic was removed, and the clear corneal incision was confirmed to be closed. In the weeks after surgery, patients instilled topical ciprofloxacin (Floxal®, Bausch&Lomb, Berlin, Germany, × 1 week) and topical anti-inflammatory medication (Dexamethasone, Bausch&Lomb, Berlin, Germany, × 4-week taper).
Results
Subject Accountability, Demographics, and Preoperative Parameters
A total of 125 eyes were included in this prospective consecutive cohort, including 81 Combined and 44 Standalone cases. Table 1 contains the demographic and preoperative ocular parameters of the cohort. In the Overall cohort (All Eyes), mean preoperative IOP was 23.5 ± 6.2 mmHg on 2.68 ± 1.02 mean medications. Nearly all eyes (124/125 or > 99%) were on preoperative medication(s); 38.4% had a history of one or more previous glaucoma surgeries (including incisional and/or laser procedures). Between the subgroups, the Combined subgroup had lower preoperative IOP and medications, lower prevalence of prior glaucoma procedures, and fewer eyes on 3 + glaucoma medications than the Standalone subgroup. Mean duration of follow-up was 77.4 months (6.4 years), with 92.8% of eyes reaching the 6- or 7-year visits.
Intraocular Pressure
Mean IOP from preoperative through the 7-year postoperative visit is shown in Fig. 1 for the Overall cohort (n = 125). Over the 7-year follow-up, mean IOP ranged from 14.1 to 15.0 mmHg, equating to a 36.2–40.0% reduction at all annual study timepoints in the Overall cohort (p < 0.001 throughout) (Fig. 1a). At the last follow-up (mean 77.4 months; 93% of patients with last visit at 6 or 7 years), 83.7% of eyes had achieved ≥ 20% IOP reduction vs preoperative, and no eyes had higher IOP vs preoperative. At LFU there was also a notable increase in the proportion of Overall eyes with IOP ≤ 18 mmHg and ≤ 15 mmHg (97.6% and 78.9% of eyes, respectively) compared to preoperative (20.8% and 1.6% of eyes, respectively) (Fig. 2a).
a Mean IOP and proportional analysis in All Eyes: preoperative visit vs last follow-up (LFU) visit*. *Last follow-up occurred at 6–7 years in 93% of All Eyes. Mean follow-up duration = 6.4 years. n in LFU calculations = eyes with ≥ 1 month follow-up. Vertical bars represent standard deviation. Preop preoperative; IOP intraocular pressure; LFU last follow-up. b Mean IOP and proportional analysis in Combined eyes: preoperative visit vs last follow-up (LFU) visit*. *Last follow-up occurred at 6–7 years in 94% of Combined eyes. Mean follow-up duration = 6.4 years. n in LFU calculations = eyes with ≥ 1 month follow-up. Vertical bars represent standard deviation. Preop preoperative, IOP intraocular pressure, LFU last follow-up. c Mean IOP and proportional analysis in Standalone eyes: preoperative visit vs last follow-up (LFU) visit*. *Last follow-up occurred at 6–7 years in 91% of Standalone eyes. Mean follow-up duration = 6.5 years. n in LFU calculations = eyes with ≥ 1 month follow-up. Vertical bars represent standard deviation. Preop preoperative, IOP intraocular pressure, LFU last follow-up
Mean IOP from preoperative through the 7-year postoperative visit is provided in Fig. 1 for the Combined and Standalone subgroups. Over the follow-up duration, mean IOP ranged from 13.8 to 14.9 mmHg in the Combined subgroup, equating to a 34.1–38.9% reduction (p < 0.001 at all annual timepoints). In the Standalone subgroup, mean IOP ranged from 14.3 to 15.3 mmHg, equating to a 39.5–43.5% reduction (p < 0.001 at all annual timepoints). At LFU, 82.3% of Combined eyes and 86.4% of Standalone eyes had achieved ≥ 20% IOP reduction vs preoperative, and all eyes in both groups had the same or lower IOP vs preoperative. There was also an increase in the proportion of eyes with IOP ≤ 18 mmHg and ≤ 15 mmHg (97.5% and 82.3% of Combined eyes, respectively; 97.7% and 72.7% of Standalone eyes, respectively) compared to the preoperative visit (27.2% and 1.2% of Combined eyes, respectively; 9.1% and 2.3% of Standalone eyes, respectively) (Fig. 2b, c).
Medication Use
Mean number of medications from preoperative to the 7-year visit is shown in Fig. 3 for the Overall cohort, Combined subgroup, and Standalone subgroup. Over the follow-up duration, mean number of medications decreased by 59.3–71.3% in the Overall cohort (p < 0.001 at all timepoints); by 57.9–69.0% in the Combined subgroup (p < 0.001 at all timepoints); and by 62.1–76.2% in the Standalone subgroup (p < 0.001 at all timepoints). At LFU, 55.3% of eyes in the Overall cohort were medication-free (vs 1 eye or < 1% preoperatively, p < 0.001), while 1 eye (< 1%) was using ≥ 3 medications (vs 61.6% preoperatively; p < 0.001). The breakdown of medication burden is provided in Fig. 4a–c for the Overall cohort, Combined subgroup, and Standalone subgroup, respectively. All eyes maintained or reduced their medication regimen vs preoperative.
a Mean number of medications and proportional analysis in All Eyes: preoperative visit vs last follow-up (LFU) visit*. *Last follow-up occurred at 6–7 years in 93% of All Eyes. Mean follow-up duration = 6.4 years. n in LFU calculations = eyes with ≥ 1 month follow-up. Vertical bars represent standard deviation. Preop preoperative, Med medication, LFU last follow-up. b Mean number of medications and proportional analysis in Combined eyes: preoperative visit vs last follow-up (LFU) visit*. *Last follow-up occurred at 6–7 years in 94% of Combined eyes. Mean follow-up duration = 6.4 years. n in LFU calculations = eyes with ≥ 1 month follow-up. Vertical bars represent standard deviation. Preop preoperative, Med medication, LFU last follow-up. c Mean number of medications and proportional analysis in Standalone eyes: preoperative visit vs last follow-up (LFU) visit*. *Last follow-up occurred at 6–7 years in 91% of Standalone eyes. Mean follow-up duration = 6.5 years. n in LFU calculations = eyes with ≥ 1 month follow-up. Vertical bars represent standard deviation. Preop preoperative, Med medication, LFU last follow-up
Safety Assessment
Implantation of two iStent inject stents was completed in all patients, with approximately two-thirds of cases in conjunction with cataract surgery and the remaining one-third as standalone surgeries. There was one intraoperative event, consisting of a mild hyphema in a Standalone eye which resolved without treatment or complications by postoperative Week 1. Postoperative adverse events during the first 5 years were described in the prior publications. Generally, events were transient and mild, and they resolved on their own or with minimal conservative treatment [11,12,13]. These events included two Combined eyes with Day 1 corneal edema, which resolved by Day 5; one Combined eye with Day 1 hyphema, which persisted to Month 1 and was accompanied by Month 1 IOP elevation > 10 mmHg vs preoperative [this was managed with a cyclophotocoaulation (CPC) procedure, and subsequent follow-up was uneventful]; one Standalone patient with cataract progression in both eyes at Month 3; one Standalone eye with uveitis at Month 24, which resolved within 3 weeks with topical anti-inflammatory medication; and two eyes with peripheral anterior synechiae (PAS) that did not obstruct stent outflow and required no intervention. A total of 62 eyes had VF MD measurements at both baseline and 7 years; of those eyes, 4.84% (3/62) experienced VF MD progression ≥ 2.5 dB. Throughout follow-up, there were no cases of occlusive PAS, stent obstruction, chronic inflammation, hypotony, endophthalmitis, choroidal detachment, myopic shift, or corneal decompensation.
Over 7 years of follow-up, seven total eyes (3 Combined, 4 Standalone) had a secondary surgical procedure. These included two cyclophotocoagulation (CPC) procedures and 1 XEN placement at 1 month, one CPC and 1 XEN placement at 6 months, and two CPC at 6 years. No filtering surgeries were performed in any eye throughout the 7 years.
Discussion
In the present prospective 7-year study, we report safety and effectiveness data from a longitudinal cohort of patients undergoing iStent inject implantation, either in combination with cataract surgery or as a standalone procedure. The completion of both types of procedures by the same surgeon in the same setting, as well as the longevity of follow-up, enable validation of long-term stent performance independent from cataract extraction. To our knowledge, this 7-year study is the longest term scientific publication to date on iStent inject, including in both real-world and FDA product-approval settings.
Tracking IOP longitudinally is particularly useful in the setting of concomitant cataract surgery, as was the case in approximately two-thirds of eyes in the cohort. In Combined cases, IOP reduced to approximately the same extent during all years of follow-up, including at points well beyond the time when any post-phacoemulsification IOP reduction would be expected to dissipate [51,52,53,54]. Meanwhile, the IOP reductions in Standalone cases were similar in extent and consistency to the Combined outcomes. Together these findings provide a strong indication that the stents (rather than the cataract extraction) are responsible for all or more of the IOP reduction.
Compared to other iStent and iStent inject studies in the literature [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48], the present study revealed similar medication reductions, in terms of both mean reduction and percent reduction. The final postoperative IOP (mean 15.0 mmHg) was also similar to prior studies and to the range typically expected after trabecular MIGS surgery. However, the preoperative starting IOP of this study was higher than in most prior reports, which is the likely reason for the greater postoperative percent and absolute IOP reductions observed in our cohort, as this is a well-recognized phenomenon in MIGS surgery [21].
In particular, the present 7-year study may be compared to the 8-year study by Salimi et al. [19], in which two first-generation iStents were implanted in combination with cataract surgery. In that study, mean postoperative IOP (14.2 mmHg) was similar to the present study, as well as the proportion of eyes with IOP ≤ 18 and ≤ 15 mmHg (91.1% and 69.9%, respectively). The incidence of secondary glaucoma procedures also was comparable (6/62 eyes or 10%), with one patient undergoing filtering surgery (1/62 or < 2%) compared to no patients in our cohort.
The outcomes of the current study were also consistent with two of the largest iStent inject studies yet completed in combined [20] and standalone [17] cases, respectively. In the 3-year, eight-surgeon pooled cohort from Clement et al. [20], mean IOP reduced to 13.9 mmHg and mean medication burden to 0.48 medications, relatively comparable to the 14.3 mmHg IOP and 0.80 mean medications observed in the Combined subgroup of our cohort at 3 years. Meanwhile, the comprehensive 13-study standalone meta-analysis by Healey et al. [17] reported IOP reductions to the range of 13.0–16.5 mmHg up to 5 years postoperatively, similar to the 14.3–15.3 mmHg IOP range seen in the Standalone subgroup through 7 years in our cohort.
In addition to the above consistencies, several other characteristics support the credibility of this study. Postoperatively, the mean IOP and medications are in the same range as the majority of studies in the iStent inject literature. The percent reduction in IOP is greater, but this can be attributed to the higher starting IOP as noted previously. Accountability was relatively high, with 93% of patients reaching 6 or 7 years of follow-up. The study data came from a single site, surgeon, and patient population, which limits the potential for confounders and variability between sites. The dataset also included both combined and standalone usage, allowing for isolation of the stents’ impact apart from cataract surgery. Finally, the mean IOP and medications in later years aligned closely with earlier time points during follow-up, suggesting stability and consistency over time.
Of note, the postoperative percentage IOP reduction was greater in the Standalone subgroup than in the Combined subgroup, which at first seemed counterintuitive. However, this likely can be attributed to the higher starting IOP of the Standalone subgroup, since the postoperative mean IOP for the Combined and Standalone subgroups both fell within a similar range (13.8–14.9 mmHg in the Combined subgroup and 14.3–15.3 mmHg in the Standalone subgroup). This greater percentage reduction with higher baseline IOP is a well-known pattern in glaucoma studies [21].
Alongside efficacy, safety outcomes in this study were favorable. A low rate of secondary glaucoma procedures was observed, and no eyes underwent filtration surgery. Preoperatively, these patients had carried a relatively substantial treatment burden, with a mean of 2.68 medications and over one-third of patients having a history of prior procedure(s). It is not unreasonable to expect that such patients might have needed a filtration procedure at some point during 7-year follow-up if they had not undergone iStent inject implantation. Additionally, the 4.84% cumulative incidence of significant visual field progression at 7 years compared favorably with other trabecular bypass MIGS pivotal trials of shorter duration. The closest comparator would be the 5-year follow-up study of the Hydrus Microstent (Alcon, Geneva, SZ) [50]. That trial reported VF MD worsening ≥ 2.5 dB in 8.4% of eyes, higher than the rate seen in our 7-year study. Two other trials, though less comparable to the current study, reported rates of 6.9% (iStent infinite, Glaukos Corp.) [49] and 1.0% (iStent inject) [14]. This study has several limitations. Given its real-world nature, the study was non-randomized and unmasked. The cohort included consecutive patients, which increases generalizability but also may introduce confounders when calculating outcomes; the 125-patient sample size helps mitigate against this. No washouts were completed, given this would not have been ethical in a real-life clinical practice. All patients were non-Hispanic white and of German nationality, so results may need to be considered cautiously in other populations. As with any population undergoing concomitant phacoemulsification, in the Combined subgroup of our study, the effect of the stents could not be isolated from that of the cataract extraction. However, post-phacoemulsification IOP reduction is known to diminish after the first few years postoperatively [51,52,53,54] and of course would not be expected in standalone cases. Thus, the consistent 7-year IOP reduction in our cohort, as well as the similar reductions observed in the Combined and Standalone subgroups, suggests it is the stents (not the phacoemulsification) that are producing the effect. Given the real-world nature of the data, not all data were available at every visit, and not all patients were able to attend all follow-ups. Future research could encompass a more in-depth annualized investigation of visual field and retinal nerve fiber layer outcomes; subgroup stratifications by glaucoma subtypes, severities, or surgical histories; or inclusion of the iStent inject W (wide-flanged) model or iStent infinite (3-stent) model.
Conclusions
In this 7-year prospective cohort of patients undergoing iStent inject implantation with or without cataract surgery, significant IOP and medication reductions were recorded through 7 years postoperative. Outcomes were similar in the overall cohort and in the Combined and Standalone subgroups, with the majority of patients attaining the endpoints of ≥ 20% IOP reduction, IOP ≤ 18 mmHg, and IOP ≤ 15 mmHg. Safety was favorable, with no sight-threatening events or filtering surgery over 7 years. Results were recorded from consecutive patients in the surgeon’s actual clinical practice, including different glaucoma subtypes and severities, as well as in both combined and standalone usage. This real-world heterogeneity helps increase the applicability and relevance to other practicing surgeons and their patients.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Gazzard G, Konstantakopoulou E, Garway-Heath D, Adeleke M, Vickerstaff V, Ambler G, Hunter R, Bunce C, Nathwani N, Barton K, LiGHT Trial Study Group. Laser in glaucoma and ocular hypertension (LiGHT) trial: six-year results of primary selective laser trabeculoplasty versus eye drops for the treatment of glaucoma and ocular hypertension. Ophthalmology. 2023;130(2):139–51.
Boland MV, Corcoran KJ, Lee AY. Changes in performance of glaucoma surgeries 1994 through 2017 based on claims and payment data for United States medicare beneficiaries. Ophthalmol Glaucoma. 2021;S2589–4196(21):00032–6. https://doi.org/10.1016/j.ogla.2021.01.004.
Radcliffe NM, Shah M, Samuelson TW. Challenging the ‘Topical Medications-First’ approach to glaucoma: a treatment paradigm in evolution. Ophthalmol Ther. 2023;12:2823–39.
Skalicky SE, Goldberg I, McCluskey P. Ocular surface disease and quality of life in patients with glaucoma. Am J Ophthalmol. 2012;153:1-9.e2.
Nordmann JP, Auzanneau N, Ricard S, Berdeaux G. Vision related quality of life and topical glaucoma treatment side effects. Health Qual Life Outcomes. 2003;1:75.
Broadway DC, Grierson I, O’Brien C, Hitchings RA. Adverse effects of topical antiglaucoma medication. II. The outcome of filtration surgery. Arch Ophthalmol. 1994;112(11):1446–54.
Muniesa MJ, Ezpeleta J, Benítez I. Fluctuations of the intraocular pressure in medically versus surgically treated glaucoma patients by a contact lens sensor. Am J Ophthalmol. 2019;203:1–11.
Nordstrom BL, Friedman DS, Mozaffari E, Quigley HA, Walker AM. Persistence and adherence with topical glaucoma therapy. Am J Ophthalmol. 2005;140(4):598–606.
Ahmed IIK, Sarkisian SR, Gallardo MJ, Brubaker JW, Grover DS. Prospective Pivotal Trial: Standalone Multiple Trabecular Micro-Bypass Stents (iStent infinite) for Uncontrolled Glaucoma. Platform Presentation at Annual Meeting of the American Society of Cataract and Refractive Surgery (ASCRS), San Diego, CA: May 5, 2023.
Businesswire.com Press Release August 23, 2021. “Glaukos Announces Market-Leading Clinical Milestone of 200 Peer-Reviewed Publications on iStent Technologies.” https://www.businesswire.com/news/home/20210823005049/en/Glaukos-Announces-Market-Leading-Clinical-Milestone-of-200-Peer-Reviewed-Publications-on-iStent%C2%AE-Technologies. Accessed 15 June 2023.
Hengerer FH, Auffarth GU, Riffel C, Conrad-Hengerer I. Prospective, non-randomized, 36-month study of second-generation trabecular micro-bypass stents with phacoemulsification in various types of glaucoma. Ophthalmol Ther. 2018;7(2):405–15.
Hengerer FH, Auffarth GU, Riffel C, Conrad-Hengerer I. Second-generation trabecular micro-bypass stents as standalone treatment for glaucoma: a 36-month prospective study. Adv Ther. 2019;36(7):1606–17.
Hengerer FH, Auffarth GU, Conrad-Hengerer I. iStent inject trabecular micro-bypass with or without cataract surgery yields sustained 5-year glaucoma control. Adv Ther. 2022;39(3):1417–31.
Samuelson TW, Sarkisian SR Jr, Lubeck DM, Stiles MC, Duh Y-J, Romo EA, Giamporcaro JE, Hornbeak DM, Katz LJ. For the iStent inject Study Group, prospective, randomized, controlled pivotal trial of iStent inject trabecular micro-bypass in primary open-angle glaucoma and cataract: two-year results. Ophthalmology. 2019;126(6):811–21.
Hunter K, Fjield T, Heitzmann H, Shandas R, Kahook M. Characterization of micro- invasive trabecular bypass stents by ex vivo perfusion and computational flow modeling. Clin Ophthalmol. 2014;8:499–506.
Huang AS, Penteado RC, Papoyan V, Voskanyan L, Weinreb RN. Aqueous angiographic outflow improvement after trabecular micro-bypass in glaucoma patients. Ophthalmol Glaucoma. 2019;2:11–21.
Healey PR, Clement CI, Kerr NM, Tilden D, Aghajanian L. Standalone iStent trabecular micro-bypass glaucoma surgery: a systematic review and meta-analysis. J Glaucoma. 2021;30(7):606–20.
Kahale F, Chanbour W, El Zein L, Brenner J, You JY, Melki S. Phacoemulsification with and without iStent: a systematic review and meta-analysis of comparative studies. Ophthalmic Res. 2023. https://doi.org/10.1159/000531077.
Salimi A, Watt H, Harasymowycz P. Long-term outcomes of two first-generation trabecular micro-bypass stents (iStent) with phacoemulsification in primary open-angle glaucoma: eight-year results. Eye Vis (Lond). 2021;8(1):43.
Clement C, Howes F, Ioannidis A, Shiu M, Manning D, Lusthaus JA, Skalicky SE, Goodwin TW. Multicenter effectiveness and disease stability through 3 years after iStent trabecular micro-bypass with phacoemulsification in glaucoma and ocular hypertension. Clin Ophthalmol. 2022;16:2955–68.
Ferguson TJ, Mechels KB, Dockter Z, et al. iStent trabecular microbypass stent implantation with phacoemulsification in patients with open-angle glaucoma: 6-year outcomes. Clin Ophthalmol. 2020;14:1859–66.
Fechtner RD, Voskanyan L, Vold SD, Tetz M, Auffarth G, Masood I, Au L, Khouri AS, Ahmed IIK, Saheb H. Five-year, prospective, randomized, multi-surgeon trial of two trabecular bypass stents versus prostaglandin for newly-diagnosed open-angle glaucoma. Ophthalmol Glaucoma. 2019;2(3):156–66.
Ferguson TJ, Dockter Z, Bleeker A, Karpuk KK, Schweitzer J, Ibach MJ, Berdahl JP. iStent inject trabecular microbypass stent implantation with cataract extraction in open-angle glaucoma: early clinical experience. Eye Vis (Lond). 2020;7:28.
Holmes DP, Clement CI, Nguyen V, Healey PR, Lim R, White A, Yuen J, Lawlor M. Comparative study of 2-year outcomes for Hydrus or iStent inject microinvasive glaucoma surgery implants with cataract surgery. Clin Exp Ophthalmol. 2022;50(3):303–11.
Ferguson T, Swan R, Ibach M, Schweitzer J, Sudhagoni R, Berdahl JP. Evaluation of a trabecular microbypass stent with cataract extraction in severe primary open-angle glaucoma. J Glaucoma. 2018;27(1):71–6.
Ferguson TJ, Ibach M, Schweitzer J, Karpuk K, Stephens JD, Sudhagoni R, Berdahl JP. Trabecular microbypass stent implantation in pseudophakic eyes with open-angle glaucoma: Long-term results. J Cataract Refract Surg. 2019;45(4):414–20.
Salimi A, Watt H, Harasymowycz P. Three-year outcomes of second-generation trabecular micro-bypass stents (iStent inject) with phacoemulsification in various glaucoma subtypes and severities. J Glaucoma. 2021;30(3):266–75.
Ferguson TJ, Swan RJ, Bleeker A, et al. Trabecular microbypass stent implantation in pseudoexfoliative glaucoma: long-term results. J Cataract Refract Surg. 2020;46(9):1284–9.
Ferguson TJ, Ibach M, Schweitzer J, Karpuk KL, Stephens JD, Berdahl JP. Trabecular microbypass stent implantation with cataract extraction in pigmentary glaucoma. Clin Exp Ophthalmol. 2020;48(1):37–43.
Guedes RAP, Gravina DM, Paletta Guedes VM, Chaoubah A. Two-year comparative outcomes of first- and second-generation trabecular micro-bypass stents with cataract surgery. Clin Ophthalmol. 2021;15:1861–73.
Neuhann R, Neuhann T. Second-generation trabecular micro-bypass stent implantation: retrospective analysis after 12- and 24-month follow-up. Eye Vis (Lond). 2020;7:1.
Salimi A, Abu-Nada M, Harasymowycz P. Matched cohort study of cataract surgery with and without trabecular microbypass stent implantation in primary angle-closure glaucoma. Am J Ophthalmol. 2021;224:310–20.
Salimi A, Clement C, Shiu M, Harasymowycz P. Second-generation trabecular micro-bypass (iStent inject) with cataract surgery in eyes with normal-tension glaucoma: one-year outcomes of a multi-centre study. Ophthalmol Ther. 2020;9(3):585–96.
Berdahl J, Voskanyan L, Myers JS, Katz LJ, Samuelson TW. iStent inject trabecular micro-bypass stents with topical prostaglandin as standalone treatment for open-angle glaucoma: 4-year outcomes. Clin Exp Ophthalmol. 2020;48(6):767–74.
Lindstrom R, Sarkisian SR, Lewis R, Hovanesian J, Voskanyan L. Four-year outcomes of two second-generation trabecular micro-bypass stents in patients with open-angle glaucoma on one medication. Clin Ophthalmol. 2020;14:71–80.
Ang BCH, Chiew W, Yip VCH, Chua CH, Han WS, Tecson IOC, Ogle JJ, Lim BA, Hee OK, Tay ELY, Yong VKY, Wong HT, Yip LWL. Prospective 12-month outcomes of combined iStent inject implantation and phacoemulsification in Asian eyes with normal tension glaucoma. Eye Vis (Lond). 2022;9(1):27.
Paletta Guedes RA, Gravina DM, Paletta Guedes VM, Chaoubah A. Standalone Implantation of 2–3 trabecular micro-bypass stents (iStent inject ± iStent) as an alternative to trabeculectomy for moderate-to-severe glaucoma. Ophthalmol Ther. 2022;11(1):271–92.
Silveira Seixas RC, Balbino M, Basile Neto A, de Alcantara Almeida Costa A, Jordão MLS, Russ HHA. Mid-term evaluation of iStent Inject® trabecular micro-bypass stent implantation with or without phacoemulsification: a retrospective study. Clin Ophthalmol. 2020;14:4403–13.
Al Habash A, Otaif W. Surgical outcomes of combined 2nd-generation trabecular microbypass (iStent Inject) and cataract surgery for the treatment of primary open-angle glaucoma in the Saudi Population. Ophthalmol Ther. 2021;10(4):923–33.
Ioannidis AS, Toteberg-Harms M, Hamann T, Hodge C. Refractive outcomes after trabecular micro-bypass stents (iStent Inject) with cataract extraction in open-angle glaucoma. Clin Ophthalmol. 2020;14:517–24.
Manning D. Real-world case series of iStent or iStent Inject trabecular micro-bypass stents combined with cataract surgery. Ophthalmol Ther. 2019;8(4):549–61.
Singh IP, Sarkisian S, Hornbeak D, Katz LJ, Samuelson T, iStent inject Study Group. Treatment success across different levels of preoperative disease burden: stratified 2-year outcomes from the pivotal trial of iStent inject® trabecular micro-bypass in primary open-angle glaucoma and cataract. Clin Ophthalmol. 2021;15:3231–40.
Voskanyan L, Garcia-Feijoo J, Belda J, Fea A, Jünemann A, Baudouin C, Synergy Study Group. Prospective, unmasked evaluation of the iStent inject system for open-angle glaucoma: synergy trial. Adv Ther. 2014;31(2):189–201.
Samuelson TW, Singh IP, Williamson BK, Falvey H, Lee WC, Odom D, McSorley D, Katz LJ. Quality of life in primary open-angle glaucoma and cataract: an analysis of VFQ-25 and OSDI from the iStent inject® pivotal trial. Am J Ophthalmol. 2021;229:220–9.
Schweitzer JA, Hauser WH, Ibach M, et al. Prospective interventional cohort study of ocular surface disease changes in eyes after trabecular micro-bypass Stent(s) implantation (iStent or iStent inject) with phacoemulsification. Ophthalmol Ther. 2020;9(4):941–53.
Konopińska J, Kozera M, Kraśnicki P, Mariak Z, Rekas M. The effectiveness of first-generation iStent microbypass implantation depends on initial intraocular pressure: 24-month follow-up—prospective clinical trial. J Ophthalmol. 2020;23(2020):8164703.
Kozera M, Konopińska J, Rękas M. Mid-term evaluation of the safety and efficacy of the iStent trabecular micro-bypass system combined with phacoemulsification. Adv Clin Exp Med. 2021;30(1):49–54.
Kozera M, Konopińska J, Mariak Z, Rękas M. Treatment of open-angle glaucoma with iStent implantation combined with phacoemulsification in polish caucasian population. Clin Ophthalmol. 2021;10(15):473–80.
Sarkisian SR Jr, Grover DS, Gallardo MJ, Brubaker JW, Giamporcaro JE, Hornbeak DM, Katz LJ, Navratil T, iStent infinite Study Group. Effectiveness and safety of iStent infinite trabecular micro-bypass for uncontrolled glaucoma. J Glaucoma. 2023;32(1):9–18.
Ahmed IIK, De Francesco T, Rhee D, McCabe C, Flowers B, Gazzard G, Samuelson TW, Singh K. Long-term outcomes from the HORIZON randomized trial for a Schlemm’s canal microstent in combination cataract and glaucoma surgery. Ophthalmology. 2022;129(7):742–51.
Poley BJ, Lindstrom RL, Samuelson TW. Long-term effects of phacoemulsification with intraocular lens implantation in normotensive and ocular hypertensive eyes. J Cataract Refract Surg. 2008;34(5):735–42.
Shingleton BJ, Pasternack JJ, Hung JW, O’Donoghue MW. Three and five year changes in intraocular pressures after clear corneal phacoemulsification in open angle glaucoma patients, glaucoma suspects, and normal patients. J Glaucoma. 2006;15(6):494–8.
Mansberger SL, Gordon MO, Jampel H, et al. Reduction in intraocular pressure after cataract extraction: the ocular hypertension treatment study. Ophthalmology. 2012;119:1826–31.
Kim DD, Doyle JW, Smith MF. Intraocular pressure reduction following phacoemulsification cataract extraction with posterior chamber lens implantation in glaucoma patients. Ophthalmic Surg Lasers. 1999;30(1):37–40.
Medical Writing/Editorial Assistance.
Editorial assistance in the preparation of this article was provided by Dr. Dana M. Hornbeak, MD, MPH, of Glaukos Corp.
Authorship.
All authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Funding
An unrestricted research grant, publication fees (i.e., Rapid Service and Open Access Fees), and editorial assistance were provided by Glaukos Corporation. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Author information
Authors and Affiliations
Contributions
Fritz Hengerer: concept and design, completion of surgeries, preoperative/postoperative management, data collection, statistical analysis, manuscript drafting. Gerd Auffarth: concept and design, preoperative/postoperative management, data collection, manuscript drafting. Ina Conrad-Hengerer: concept and design, preoperative/postoperative management, statistical analysis, manuscript drafting.
Corresponding author
Ethics declarations
Conflict of Interest
Fritz Hengerer: Research grant and lecture fees from Glaukos Corp (unrelated to study/publication). Ina Conrad-Hengerer: No disclosures. Gerd U. Auffarth: (1 = Research Grants; 2 = Travel Expenses; 3 = Lecture Fees; 4 = Consulting). Acufocus3. Alcon (1, 2, 3, 4). AMO/Johnson&Johnson (1,2,3,4). Biotech (1,3). Carl Zeiss Meditec (1,2,3,4). Contamac (1). Cristalens (1,3,4). Croma (1). Eyebright (3). EyeYon (1,2,4). Hanita (1). Hoya (1,2,3). Kowa (1,2,3). Teleon (1,2,3). Oculus (1,3). Physiol (1). Presbia (4). Rayner (1,2,3,4). Rheacell (1). SIFI (1,2,3,4). Ursapharmc (1,2,3). VSY (1,3,4).
Ethical Approval
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee (the Institutional Review Board of the University of Heidelberg [reference #S-482/2012]), and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hengerer, F.H., Auffarth, G.U. & Conrad-Hengerer, I. 7-Year Efficacy and Safety of iStent inject Trabecular Micro-Bypass in Combined and Standalone Usage. Adv Ther 41, 1481–1495 (2024). https://doi.org/10.1007/s12325-024-02788-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-024-02788-y