Abstract
Heart failure (HF) remains a major cause of mortality and morbidity worldwide. Understanding the genetic basis of HF allows for the development of disease-modifying therapies, more appropriate risk stratification, and personalised management of patients. The advent of next-generation sequencing has enabled genome-wide association studies; moving beyond rare variants identified in a Mendelian fashion and detecting common DNA variants associated with disease. We summarise the latest GWAS and rare variant data on mixed and refined HF aetiologies, and cardiomyopathies. We describe the recent understanding of the functional impact of titin variants and highlight FHOD3 as a novel cardiomyopathy-associated gene. We describe future directions of research in this field and how genetic data can be leveraged to improve the care of patients with HF.
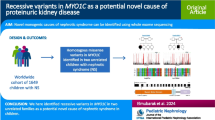
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Heart Failure, Cardiomyopathies, and Genetic Analyses
Heart failure (HF) is a heterogeneous cardiac condition arising from functional or structural abnormalities of the heart, resulting in impaired ventricular filling and cardiac output [1]. It is highly prevalent, affecting over 64 million individuals worldwide [1]. Despite therapeutic advances, the risk of HF-related morbidity and mortality remains high, with an average 5-year survival rate of approximately 50% [2]. The estimated heritability (h2) of HF, the amount of variation in HF due to genetic factors, is substantial (h2 ~ 18%-26% [3]), and elicited studies to identify disease-associated genomic loci to inform novel therapeutic strategies [4,5,6].
Cardiomyopathies are structural or functional myocardial conditions that are an established cause of HF. They present in the absence of secondary causes of HF such as hypertension, valvular disease, coronary artery disease, or congenital heart disease. Patients with cardiomyopathy may present with symptoms of HF with reduced ejection fraction (HFrEF) or preserved ejection fraction (HFpEF).
Many of the proteins transcribed from genes that are curated to have definitive evidence of causing cardiomyopathies are found in the sarcomere of cardiomyocytes. The sarcomere is the basic contractile unit of the cardiomyocyte [7]. It is composed of thin actin filaments and thick myosin filaments (Fig. 1) [8, 9]. The sliding filament theory describes cardiac contraction occurring through the motion of actin filaments sliding past myosin filaments and their interaction [10]. The tropomyosin and troponin complex are fundamental components of the sarcomere, which function as regulatory proteins and control the interaction of actin and myosin, respectively. [11] Variants in sarcomeric genes, such as myosin binding protein (MYBPC3), myosin heavy chain (MYH7), and titin (TTN), are major genetic determinants of cardiomyopathies [12], with ~ 30% of patients heterozygous for a sarcomere mutation [13, 14].
Dilated cardiomyopathy (DCM) is characterised by the dilation of the left or both ventricles of the heart, which reduces myocardial contractility leading to systolic dysfunction [15]. It is regarded as one of the primary contributors to HFrEF and is the leading indication for heart transplantation globally [16, 17]. Hypertrophic cardiomyopathy (HCM) is characterised by left ventricular wall thickness [18]. The concentric hypertrophy accompanied by fibrosis and myocardial disarray leads to impaired myocardial relaxation and diastolic dysfunction. HF is prevalent in most patients with obstructive HCM (those with left ventricular outflow tract obstruction due to septal hypertrophy) and ~ 10% of patients with non-obstructive HCM [16]. HFpEF is the most common HF phenotype amongst HCM patients as a result of decreased left ventricular compliance secondary to increased wall thickness. [19]
Genetic research on cardiomyopathies has aided the determination of the mechanisms underlying abnormal cardiac function leading to HF. Historically, linkage analyses of familial cardiomyopathies identified causal DNA variants inherited in a Mendelian fashion [20]. Linkage analysis refers to statistical methods used to map a gene to the region of the chromosome in which the gene is located [21]. Improved genome-wide sequencing technologies have allowed for unbiased assessments of the genome; and genome-wide association studies (GWASs) of common DNA variants [22, 23]. Genoty** microarray data is used as input for GWAS and measures common variants sporadically across the genome. GWASs map the polygenic architecture of HF by comparing the alleles of single nucleotide polymorphisms (SNPs) present in patients with HF to those of non-HF or reference populations [24]. Identification of the common variants with alleles that are significantly increased or decreased in patients with HF has implicated polygenicity and identified modifying genetic factors, in disease [25]. The heterogeneous presentation of HF suggests a diverse genomic landscape and we discuss some examples in this review [26,27,28].
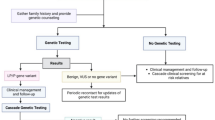
The recent European Society of Cardiology guidelines (2023) for the management of cardiomyopathies recommend genetic testing in individuals with cardiomyopathies to inform prognosis, treatment selection, reproductive advice, and psychological benefit [29]. There are different methods available to sequence the genome depending on genome coverage and cost. The use of next-generation sequencing (NGS) has revolutionised genomic research, allowing for the human genome to be sequenced within 20 minutes cost-effectively [30, 31]. Whole-genome sequencing (WGS) determines the entire human genome, encompassing the non-protein coding (denoted “non-coding”, but codes for some RNA transcription and other regulators) and protein-coding regions. In contrast, whole-exome sequencing (WES) determines the exome, encompassing only the protein-coding exons [32]. Although WES only determines the coding regions, the rationale for its utility is that genetic variants within the coding region account for the most significant effect variants related to diseases [33]. WGS and WES improve the yield of a cardiomyopathy genetic diagnosis when compared to genetic testing using targeted panels (i.e., selected gene panels that only sequence disease-associated genes). While panel sequencing is more rapid, WGS and WES allow for revisiting the genetic data upon identification of novel cardiomyopathy-associated genes from a once-off effort (e.g., the recent identification of disease-causing filamin C [FLNC]) but at an increased expense, computational time, bioinformatics, and computational requirement [34].
WES and WGS allow for the discovery of novel disease-causing variants [33] but in a clinical setting, the identification of genetic variants with insufficient evidence of pathogenicity (variants of uncertain significance [VUSs]) can confuse patients and are less useful to the clinician and healthcare programs. The American College of Medical Genetics and Genomics created guidelines for the interpretation of sequence variants based on variant evidence (e.g., population data, computational data, functional data, and segregation data; results reported as (likely) benign, VUS, or (likely) pathogenic). The ClinGen Consortium Gene-Disease Clinical Validity curation process allows experts to evaluate the strength of evidence supporting or refuting a claim that variation in a particular gene causes a particular monogenic disease (results reported as definitive, strong, moderate, limited or weak evidence for causing disease) [35, 36].
This review explores the common and rare variants associated with mixed aetiology HF. We highlight the common variants associated with HCM and DCM from recent large GWAS before exploring the implications of rare variants and the function of pathogenic variants that have a causal relationship with cardiomyopathies (Graphical Abstract). We describe truncating variants in the titin gene, the most common genetic cause of DCM, and recent mechanistic insights into how they influence cardiac function in DCM, and describe a recent HCM-associated gene, FHOD3, before highlighting future directions in the field and how genetic data may be leveraged to improve the care of patients with HF.
Common DNA Variants Associated with Heart Failure
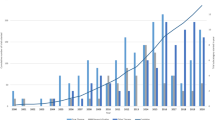
Cappola et al. (2010) conducted an early HF GWAS-like study, profiling 30,000 SNPs in 2,000 genes thought to be associated with cardiovascular disease [37]. They compared the genotypes of patients with advanced HF to controls without HF, and SNPs that reached statistical significance were tested in a replication cohort (statistical significance is usually a Bonferroni Correction for the number of tests (SNPs), e.g., standard GWAS threshold is P = 5 × 10–8; a P-value of 0.05/1 million independent SNPs). Two significant SNPs were identified; one near HSPB7 encoding a heat shock protein and one near FRMD4B (FERM domain containing protein B).
It was postulated that carrying these variants individually only translated to a small, clinically insignificant, increased risk of HF. Variants observed enough times for statistical power to identify a difference in the population have alleles that are common and usually found in > 1% of the population. HF prevalence is ~ 1% and so such common variants individually cannot have a large effect in causing HF [38]. Genome-wide rare variant association studies (RVAS) of rare genetic variants (i.e., found in one patient) with predicted large effects on disease are usually grouped by a certain category to allow for statistical testing (e.g., by gene and variant consequence to the protein for a specific gene; any rare MYBPC3 missense variants).
Shah et al. (2020) conducted a meta-analysis of HF GWAS using data from 29 studies encompassing 47,309 cases and 930,014 controls [42]). Many of the loci identified have strong associations with cardiovascular disease risk factors such as FTO (fat mass and obesity-associated; associated with BMI), PITX2 (the PITX2 transcription factor; associated with atrial fibrillation [AF]), and LPA (lipoprotein(a); associated with coronary artery disease [CAD]). To determine whether these variants were associated with HF independent of other risk factors, the authors undertook a multi-trait conditional and joint analysis. Conditioning for AF, the authors found that there was a > 50% attenuation in HF risk for PITX2 and other AF-associated loci (SYNPOL2, KLHL3, and AGAP5) remained independently associated with HF. Similarly, conditioning for CAD fully attenuated the HF risk for LPA.
Levin et al. (2022) conducted a large multi-ancestry GWAS including 115,150 HF cases and 1,550,331 controls, leveraging data from various biobanks (HERMES, Penn Medicine Biobank, eMERGE, Mount Sinai BioMe, Geisinger DiscovEHR, FinnGen, and the Global Biobank Meta-Analysis Initiative) [40]. They identified 47 disease-associated loci (Table 1) of which 39 were validated in an independent replication cohort. The authors also evaluated the genetic correlations (the genetic similarity of two traits) between cardiac imaging phenotypes (left ventricular end-systolic volume, end-diastolic volume, and ejection fraction) and HF. They found a substantial genetic correlation between HF and left ventricular end-systolic volume (correlation coefficient R = 0.36; P = 3.73 × 10−16).
Both GWAS meta-analyses identified the PITX2 locus to have the strongest association with HF. The PITX2 transcription factor plays an important role during embryonic development of the heart [43]. Loss of function variants (e.g., stop gained, frameshift, and essential splice variants) in PITX2 have been associated with atrial structural and functional remodelling leading to an increased risk of arrhythmogenesis [44].
Joseph et al. (2022) conducted a GWAS using the US Million Veteran Program (MVP) to assess the separate genetic architecture of HFrEF and HFpEF [41]. They identified 13 genetic loci associated with HFrEF, compared to only one locus for HFpEF (near the FTO gene). The estimated heritability of the HF subgroups was lower for HFpEF than HFrEF (h2 = 1.9% and 3.1%, respectively). There is a need for sub-phenoty** of HFpEF patients as the current classification encompasses the final manifestation of multiple diverse aetiologies. More refined phenotypic definitions of HFpEF may improve the statistical power for genetic discovery in future studies or identify modifying environmental and non-genetic factors.
Henry et al. (2023) reported a GWAS meta-analysis on a cohort of 1.9 million ancestrally diverse people, including 153,174 cases of HF [42]. They identified 66 genetic susceptibility loci across HF subtypes (Table 1). The IGFBP7 gene was identified to have a significant association with non-ischaemic HFpEF. IGFBP7 encodes an anti-angiogenic factor and has been implicated in cardiomyocyte senescence and cardiac remodelling [45]. Its association with HFpEF raises the possibility of altered tissue homeostasis and renewal contributing to the development of this phenotype. The estimated heritability of HF explained by common variants in this study was 5.4% for unclassified HF. Again, the heritability of non-ischaemic HFrEF was substantially greater than that of non-ischaemic HFpEF (h2 = 11.8% and 1.8%, respectively). The authors assessed the genetic correlation between HF subtypes; HFrEF and HFpEF had a substantial genetic correlation (rg = 0.42; SE = 0.18).
Many of the genetic loci identified in mixed aetiology HF GWAS to date are those associated with HF risk factors such as AF and CAD. Importantly, the myriad of conditions which lead to HF (and some which may be genetically opposing, e.g., HCM and DCM) limit the statistical power to detect common variants associated with the disease. There is a need for better sub-grou** of patients with HF, perhaps based on aetiology (e.g. ischaemia or valvular disease leading to HF), to better investigate genetic associations, alongside the analysis of larger biobanks.
Common DNA Variants Associated with Hypertrophic Cardiomyopathy
It is well-accepted that the initial monogenic sarcomere mutation hypothesis alone for HCM is outdated [46,47,48]. This is especially true considering that ~ 60% of HCM cases detected at the onset of disease are genotype negative and many without family history [49]. Sarcomere-negative HCM is a complex, likely polygenic trait. A GWAS by Harper et al. (2021) confirmed a markedly greater common variant genetic contribution to sarcomere-negative HCM than sarcomere-positive/Mendelian HCM (h2 = 34% and 16%, respectively) [27]. This supports the hypothesis that common variants in combination may have a causal role in HCM.
A genetic risk score (GRS) was leveraged to predict the odds of HCM from 27 HCM-associated SNPs. To increase statistical power, the GRS was estimated from a meta-analysis of three independent HCM populations of European descent with 1,769 cases and 39,828 controls. A protective effect against HCM was observed for individuals in the lowest quintile. HCM risk more than doubled for individuals in the highest quintile (i.e., participants with risk alleles) compared to the central 60% of the cohort analysed [27].
Variants in the cyclic-dependent kinase inhibitor 1A (CDKN1A) locus have been significantly associated with HCM (rs3176326) [27, 50]. The protein is involved in cell cycle arrest. A recent GWAS meta-analysis concluded that this kinase holds a direct phenotypic effect in the heart, causing reduced left ventricular systolic function and cardiomyocyte cell cycle arrest [39]. An in-vivo model of CDKN1A knockout mice developed cardiac hypertrophy and HF [51]. A phenome-wide association study (PheWAS; comparing a trait in individuals with or without a reported clinical outcome) further identified the CDKN1A locus as significantly associated with HCM and ECG traits (PR interval and QRS duration) [52].
Tadros et al. (2023) conducted a GWAS of over 5,000 HCM cases and over 30,000 UK Biobank participants with cardiac magnetic resonance imaging available for analyses [53]. 33 loci and 35 novel loci were associated with HCM. When stratified by sarcomere-positive and sarcomere-negative HCM, an additional 1 locus and 4 loci were identified, respectively. A locus on chromosome 11 (near MYBPC3, a definitive-evidence HCM gene) associated with HCM and sarcomeric HCM, but not sarcomere-negative HCM, suggesting the locus is in linkage disequilibrium with founder MYBPC3 variants. Higher heritability was estimated for genotype-negative HCM compared to genotype-positive HCM (h2 = 29% and 16%, respectively), reflecting the complex genetic influence underlying HCM [27].
Common DNA Variants Associated with Dilated Cardiomyopathy
Pirruccello et al. (2020) undertook a GWAS of cardiac imaging traits in the UK Biobank cohort to identify genetic loci influencing DCM risk [54]. Utilising the cardiac magnetic resonance imaging (MRI)-derived left ventricular measurements of end-diastolic and systolic function from 36,000 participants, 45 previously unreported genome-wide significant loci were identified. Common variants at 18 loci were identified near Mendelian cardiomyopathy genes; 12 were newly discovered. GRS based on the cardiac MRI parameters demonstrated that common genetic variation influenced cardiac function and structure. Notably, the GRS for indexed left ventricular end-systolic volume (LVESVi), comprising 28 SNPs, robustly predicted DCM. However, the findings were limited to individuals of European ancestry.
Garnier et al. (2021) conducted a GWAS evaluating over 2,700 sporadic DCM cases [55]. The findings identified robust replication of two out of three novel genome-wide significant loci found to increase the risk of sporadic DCM by a third. This includes SLC6A6 which encodes a taurine transporter, a nonessential amino acid which maintains cellular integrity and is found in very high concentrations in the heart and muscle [56,57,58,59]. A recent article in Science has identified anti-aging effects of this amino acid but a clinical trial is needed to investigate whether supplementation improves the symptoms of patients with DCM [60].
Zheng et al. (2023) conducted the largest DCM GWAS to date comprising over 14,255 DCM cases from the HERMES consortium [61]. Through gene prioritisation strategies such as pathway enrichment analysis and utilisation of genetically correlated CMR traits from UK biobank, 80 loci associated with DCM were discovered. Genes involved in cell-to-cell adhesion and cell-to-matrix interaction were found to play a role in DCM pathogenesis, alongside established biological pathways such as contractile and cytoskeletal functions. An example novel gene is SSPN, encoding sarcospan, a core component of the tetrameric dystrophin-glycoprotein complex (DGC) typically associated with muscular dystrophies. A preclinical study by Parvatiyar et al. (2019) in mice demonstrated that SSPN overexpression alleviated cardiomyopathy associated with Duchenne muscular dystrophy [62]. In the early 2000s, variants in another component of the DGC, δ-sarcoglycan (SGCD), were characterised in patients with familial and sporadic cases of DCM without any skeletal muscle disease [63].
The role of common variants causing DCM is supported by the generation of a GRS in over 300,000 participants with DCM. The GRS associated with CMR traits (reduced LVEF, increased LVEDV and LVESV). The penetrance of rare DCM-associated variants, the proportion of individuals with a variant that have DCM, is influenced by additional genetic and environmental influences. In this study, rare variant penetrance was modulated by common variants in the general population with a four-fold increased risk compared to the median [56]. In rare variant carriers, the GRS associated with a two-fold increase in DCM compared to the median. PheWAS of the GRS identified associations with cardiovascular phenotypes and obesity and portrayed an inverse relationship with HCM.
Rare Variants Associated with Hypertrophic Cardiomyopathy
In general, rare variants (with a minor allele frequency < 0.1%) have larger effects on disease than their common variant counterparts [64, 65] (Graphical Abstract). Pathogenic, rare variants in twelve sarcomere-encoding genes are reported with definitive evidence for HCM (MYBPC3, MYH7, MYL2, MYL3, TNNI3, TNNT2, TPM1, ACTC1) in addition to four that have been newly upgraded by the ClinGen consortium (CSRP3, TNNC1, ALPK3, PRKAG2) but are not yet standard (Table 2) [18, 20, 35, 66]. The gene-disease associations were evaluated from published clinical genetic and experimental evidence. Genetic evidence included case-level data and variant analysis, while experimental evidence encompasses categories such as expression data and functional alterations. A gene was classified as "definitive" if it received a strong evidence score with consistent publications over at least three years and no contradictory evidence [8, 35].
Identifying rare variants enables precise patient risk stratification in family members. Sarcomeric variants are associated with an increased risk of mortality or experiencing major adverse cardiac events, primarily attributed to outcomes such as HF or arrhythmias. Individuals diagnosed with HCM who carry rare variants exhibit a notably heightened risk compared to those with HCM who do not have these variants [67].
Pathogenic variants in MYBPC3 and MYH7 account for most genotype-positive HCM cases [31], whereas the other genes account for < 10% of cases [68, 69]. MYBPC3 encodes cardiac myosin-binding protein C (cMyBP-C), a key sarcomere protein that binds both actin and myosin [70]. MYH7 is a sarcomeric gene encoding myosin heavy chain beta (MHC-β) and plays a crucial role in the contraction of muscle fibres [71, 72]. It is responsible for the ATP-dependent sliding movement of actin and myosin filaments which results in contraction [73].
The consequences of variants on the protein structure are important: protein-altering variants (denoted here as truncating [loss of function] plus non-truncating [e.g., missense variants]) in MYBPC3 and non-truncating variants in the other seven genes are associated with HCM [74]. The most common variants in MYBPC3 are frameshift, nonsense (stop gained), and essential splice-site variants, which result in premature termination codons [75]. Non-truncating variants (e.g., missense, inframe indels, start lost, and stop lost variants) account for roughly 15% of MYBPC3 HCM, with clinical outcomes being similar in patients with truncating or non-truncating variants [76].
MYL2 and MYL3 encode myosin regulatory and essential light chains, respectively. [76] Compared to MYH7 and MYBPC3, pathogenic variants in MYL2 and MYL3 as a cause of HCM are relatively rare [77, 78]. They present with variability in clinical manifestation and disease severity [79, 80]. TNNT2 and TNNI3 encode proteins belonging to the troponin complex. TNNT2 encodes for troponin T within the cardiac muscle, which helps anchor the troponin complex on the actin-tropomyosin thin filaments and has a central role in the regulation of muscle contraction and relaxation [81]. TNNI3 encodes the cardiac isoform of troponin I, the inhibitory subunit of the troponin complex, which prevents muscle contraction by inhibiting the actomyosin activity of the myosin-heavy chain [82, 83]. TPM1 (tropomyosin 1) regulates the contraction of the sarcomere by controlling interactions between actin and myosin [84]. ACTC1 encodes cardiac alpha-actin, which is a major component of the thin filaments and is responsible for the alignment and stability of thin filaments within the sarcomere [85].
Variants in other genes can cause rare syndromic disorders with isolated hypertrophy. Examples include variants in PRKAG2, GLA, ALPK3, CACNA1C, DES, FHL1, FLNC, GLA, LAMP2, PRKAG2, PTPN11, RAF1, RIT1, and TTR. Pathogenic variants in PRKAG2, encoding the gamma-2 regulatory subunit of adenosine monophosphate (AMP)-activated protein kinase (AMPK) [86], cause severe ventricular hypertrophy, electrocardiographic pre-excitation and conduction system disease [87]. These variants cause glycogen accumulation within cardiomyocytes, a disease of cardiac glycogen metabolism [87]. Lopez-Sainz et al. (2020) demonstrated an increased risk of adverse cardiovascular events such as atrial fibrillation, advanced HF, life-threatening arrhythmias, and sudden cardiac death in carriers with incomplete penetrance [88, 89]. A worsening prognosis was observed in those with abhorrent glycogen metabolism compared to disease caused by a sarcomeric variant [88]. Fabry disease is caused by recessive variants in the GLA gene resulting in reduced or absent activity of the enzyme alpha-galactosidase [90]. The altered enzyme activity results in glycophospholipid metabolism leading to the deposition of globotriasylceramide within the myocardium causing HCM as the main cardiac manifestation [90, 91]. However, unlike PRKAG2 variants, Fabry disease is treatable with enzyme replacement therapy [88], and hence early recognition of its diagnosis is imperative to improve prognosis.
Rare variants associated with HCM are increasingly recognised with other phenotypes, such as restrictive cardiomyopathy. Restrictive cardiomyopathy presents with restrictive left ventricular filling due to impaired relaxation and compliance [92]. The genes with variants associated with restrictive cardiomyopathy include TNNT2, ACTC1, MYBPC3, MYL2 and MYL3; all of which are associated with HCM [93]. Although uncommon, HCM can present similarly to primary restrictive cardiomyopathy, whereby patients have mild hypertrophy but severe diastolic dysfunction; coined HCM with ‘restrictive phenotype’. Notably, a missense variant in MYL2 was found to increase the incidence of the restrictive phenotype by over one-third [94].
Understanding the estimated penetrance of variants is of utmost importance to inform risk stratification. Penetrance is the probability of disease given a risk variant. In patients, the penetrance of pathogenic variants in HCM was estimated in a recent meta-analysis from Topriceanu et al. (2024) as ~ 55% for MYBPC3, 65% for MYH7, 65% for MYL2, 32% for MYL3, and 60% for TNNT2 and TNNI3 [95]. With large datasets now available, the population penetrance of specific variants in cardiomyopathy-associated genes is now being estimated and is lower than that observed in the clinic [96].
Rare Variants Associated with Dilated Cardiomyopathy
Rare variants have been identified that are associated with DCM (Table 3). [36, 97, 98] Jordan et al. (2021) used published results from genetic testing and experimental evidence to classify variants [36]. 12 genes including LMNA, BAG3, TTN, MYH7 and TNNT2, have definitive evidence for causing DCM.
LMNA encoding lamin, a component of the nuclear envelope, is one of the most common genes associated with DCM [99, 100]. This gene also has high population penetrance [99]. Both heterozygous and homozygous variants have been reported to result in DCM, with homozygous variants resulting in a fatal phenotype and a high rate of sudden cardiac death due to arrhythmias [100]. Typically, LMNA-related DCM has early onset arrhythmias followed by conduction abnormalities which can result in sudden cardiac death [101].
BAG3, encoding B-cell lymphoma-associated athanogene 3 or BAG cochaperone 3, has many crucial roles within cardiomyocytes; it maintains sarcomere integrity, regulates macroautophagy, promotes the expression of BLC2 to maintain antiapoptotic properties, boosts mitochondrial quality, and regulates beta-adrenergic/L-type calcium channels [102]. Truncating variants in BAG3 have been observed in DCM patients [97]. The loss of function likely causes destabilization of the Z-disc, impaired protein homeostasis leading to proteotoxicity, and increased susceptibility to apoptosis [66]. Pathogenic variants in BAG3 present with variability in clinical manifestation and age of onset [102]. Male sex, decreased left ventricular ejection fraction, and large ventricular end-diastolic diameter, are associated with adverse outcomes in those with pathogenic variants in BAG3 [103].
A particular common missense variant within BAG3, characterized by the substitution of cysteine with arginine at position 151 of the BAG3 protein (C151R; rs2234962) [104], demonstrates a potential cardioprotective function in GWAS of DCM, HF, and ejection fraction [108] with risk for HCM [52]. The variant is associated with proteins involved in the maintenance of myofibrillar integrity and causes improved response to proteotoxic stress [105]. Comprehending the functional alteration in BAG3 associated with this cardioprotective effect holds promise for devising therapeutic interventions aimed at targeting the C151R variant specifically. Such insights into genetic modifiers could pave the way for the development of tailored treatments, including the overexpression of this BAG3:p.C151R variant to leverage its potential benefits.
TNNT2 is associated with an early, relatively aggressive form of DCM [106]. Likewise, MYH7 is associated with an early age of onset, and HF is observed more commonly than ventricular arrhythmias in these patients [100]. Truncating variants in FLNC have been recently associated with DCM [107]. FLNC codes for the cytoskeleton protein filamin C, which functions as an actin crosslinking protein and anchors sarcolemma proteins to the cytoplasm to maintain the structural integrity of the sarcomere [108]. Studies of FLNC in DCM have been limited by a small number of participants due to the use of targeted sequencing methods that excluded analysis of the gene [109, 110]. Ader et al. (2019) found that among 300 patients with known DCM, 10 carried a mutation in FLNC (3%) [119]. Patients carrying a pathogenic variant in FLNC have been reported to have a high risk of sudden cardiac death and a more malignant clinical course [109, 110]. Pathogenic variants in FLNC and LMNA are associated with a significant increase in myocardial fibrosis [100, 107] and result in a worse prognosis regarding mortality and life-threatening arrhythmia compared to other genetic variants [51, 110,111,112,113,114]. The 2023 European Society of Cardiology guidelines also highlight variants in DSP (encoding desmoplakin) [115], RBM20 (encoding RNA-binding motif protein 20) [116], PLN (encoding phospholamban) [117] and TMEM43 (transmembrane protein 43), with a substantially higher risk of arrhythmias. Variants in TMEM43 are more strongly associated with arrhythmogenic cardiomyopathy (ARVC or ACM) [118,119,120,121].
Overlap** and Opposing Genetic Factors of HCM and DCM
Genes with rare variants that have definitive or moderate evidence curated by experts for both HCM and DCM have been identified (e.g., TNNC1, TNNI3, TNNT2, MYH7, TPM1, ACTC1, JPH2, PLN). PLN is associated with “intrinsic cardiomyopathy” as while most variants reported are associated with DCM, HCM has also been reported [67]. Missense variants in MYH7 are a common pathogenic cause of DCM and HCM, with the current understanding that an individual missense variant in MYH7 can convey risk for DCM or HCM, but not both [122].
Pathogenic MYH7 variants cause cardiomyopathies primarily due to decreased (DCM) or increased (HCM) sarcomere force generation [66]. Variants in MYH7 causing HCM produce an abnormally activated protein that incorporates into the sarcomere as a ‘poison peptide’. Such dominant-negative variants associated with HCM are concentrated in the myosin head domain (amino acid residues 181–937 [66]; including the motor domain) of the MYH7 gene, whereas those associated with DCM may occur across the gene. DCM-associated MYH7 missense variants likely reduce the passive stiffness of myofibrils and are deficient in force generation and force-holding capacity [66, 68]. Variants in the globular head can affect the formation of binding sites for actin and cross-bridges for contraction [123]. Variants can either directly affect motor function or can impact on myosin "interacting head motif" and impair kinetics [66]. A study by Ujfalusi et al. (2018) focused on pathogenic variants within the myosin head domain of MYH7, selecting five DCM-linked and two HCM-linked variants [124]. The authors concluded that pathogenic variants of MYH7 caused discrepancies by altering individual steps in the ATPase cycle. Compared to wild-type or HCM variants, myosin with DCM-associated variants had a lower duty ratio; the motor domain remained bound to actin for a decreased proportion of the ATPase cycle. As a result, less force was generated and there was reduced force-holding capacity in DCM mutants, while HCM mutants had greater force-holding capacity. However, the results relied on the mechanisms of a fully activated cross-bridge, while cardiac sarcomeres operate at submaximal activation.
Recent HCM and DCM genome-wide association studies (GWAS) of common DNA variants (with individually small effects on disease) have identified overlap** loci for cardiomyopathies. Tadros, Francis, Xu, Vermeer, et al. (2021) [155] showed an opposing relationship between HCM- and DCM-associated common DNA variants and left ventricular measures of structure and function through analyses of the common variants [155]. Genetic correlation between the left ventricular measures of structure and function had divergent relationships with HCM and DCM (most strikingly with end-systolic volume [LVESV; DCM+, HCM-], ejection fraction [LVEF; HCM+, DCM-], and measures of strain [HCM+, DCM-]). They identified variants associated with both cardiomyopathies that showed opposite directions of effect in HCM versus DCM [23]. The authors concluded that this indicates that genetic loci underlying the variability of left ventricular function in the general population may be differentially involved in susceptibility to HCM and DCM. An assessment of cumulative variation in cardiomyopathy-associated genes also identified oppositions between HCM and DCM [125] and a pheWAS of HCM-derived GRS identified a protective relationship for HF [126].
Further to the described opposing relationships between HCM and DCM with variants in BAG3 and MYH7, an example of an opposing common variant is a SNP (rs3176326) in CDKN1A [23]. The protein is involved in cell death and cell cycle arrest, and knockout mice can regenerate damaged or missing tissue. The minor A allele of the variant is associated with decreased muscle expression (GTEx browser); decreased cell death and thus more cell growth. This increase in cell cycling increases HCM risk and decreases DCM and HF risk. This opposing relationship provides potential support for a protection theory, where variants influencing non-obstructive HCM may provide some protective effect against DCM and HF risk at the cellular level.
FHOD3: A Reoccurring Hypertrophic Cardiomyopathy-Associated Gene
The FHOD3 (formin homology 2 domain containing 3) protein regulates sarcomere organisation and myofibrillogenesis and maintains the contractile apparatus in cardiomyocytes [128, 129]. The burden of protein-altering variants in FHOD3 is significantly increased in patients with HCM compared to controls [130]. In 2020, Ocha et al. discovered copy number variants (CNVs; copies of a segment of DNA that vary in number) in FHOD3 in patients with HCM that were not identified in controls [131]. A GWAS by Wooten et al. (2013) identified an FHOD3 intronic variant found to more than double the risk of HCM (rs516514, P = 1.25 × 10–7) [49, 132] that was in linkage disequilibrium with the sentinel missense SNP FHOD3-V1151l (rs2303510; P = 1.76 × 10–9). FHOD3-V1151l was also associated with HCM two further cohort analyses [132]. A genetic analysis of FHOD3 variants in a Chinese population identified FHOD3 candidate variants as independent predictors for cardiovascular death and all-cause death in HCM (adjusted HR, 3.02; 95% CI, 1.09–6.85; P = 0.035) [131]. A more common, intermediate effect variant in FHOD3 (p.Arg637Gln; gnomAD NFE AF 0.03%) has been associated with a clinically aggressive course and an earlier presentation in homozygous carriers, consolidating the association between FHOD3 and the development of HCM [133].
TTN: Recent Evidence for a Major Cause of DCM
Titin is the largest human protein spanning from the M-line to the Z-disc of the cardiac sarcomere (Fig. 1). Truncating variants in the TTN gene (TTNtvs) have been implicated in numerous cardiomyopathies, including DCM and other environment-influenced cardiomyopathies such as peripartum, alcohol-induced, and chemotherapy-induced, cardiomyopathy [134,135,136,137,138]. Heterozygous TTNtvs are the most common genetic cause of DCM (15%-20% of all patients with DCM) and are found in about 2% of the general population [137, 139, 140]. Due to the size of the gene, analyses of TTNtvs are complicated by the rarity of individual- and family-specific variants so effects are usually assessed in aggregate.
Roberts et al. (2015) used data from over 5,000 patients to establish that TTNtvs in constitutive exons expressed in the heart were the most pathogenic [138]. Importantly, if the TTNtvs can be ‘bypassed’ by alternate splicing, its effect on the cardiac phenotype is limited [141]. Thus, TTNtvs in the A-band have a higher odds ratio for DCM than those in parts of the highly spliced I-band [137, 142]. Notably, the position of the TTNtvs did not correlate with the patient’s age at the time of transplant or the pretransplant left ventricular function in a study of DCM hearts removed at transplantation [143]. Studies identifying modifiers of TTNtvs are needed.
The mechanisms by which TTNtvs cause cardiomyopathy has been difficult to decipher largely due to the size of the gene. Suggested pathomechanisms included nonsense-mediated decay of TTNtvs mRNA and haploinsufficiency (the remaining functional copy of the gene is not adequate for normal function) [143,144,145]. The ‘poison-peptide’ theory, which states that truncated titin (tr-titin) hampers sarcomeric function, was considered a less likely explanation as tr-titin was not shown to be present in adult DCM hearts [146]. However, this was recently shown by McAfee et al. (2022) [143] who also observed lower amounts of wildtype titin in mutant hearts, indicating haploinsufficiency occurring in parallel.
Fomin et al. (2022) further revealed that the tr-titin proteins are sequestered in intracellular aggregates that dysregulate protein quality control pathways (PQCs), mainly the ubiquitin pathway [145]. There was increased ubiquitin degradation of wild-type titin in mutant hearts, which may cause the associated poor contractility. Inhibition of PQCs using proteasome inhibitors increased levels of both tr-titin and wild-type titin, resulting in increased contractility of human induced pluripotent stem cell-derived cardiomyocytes (hiPSC-CMs) derived from patients with TTNtvs.
Evidence from these studies suggests that TTNtvs cause DCM through both haploinsufficiency and the ‘poison peptide’ theory. The two functional studies analysed samples from patients with end-stage HF and future research with samples from patients at different stages of disease may provide greater insight into which mechanisms require treatment prioritisation and which TTNtvs have highest penetrance. As the penetrance of TTNtvs is incomplete, even in pathogenic locations, many individuals do not develop cardiomyopathy [138] and our understanding of this is required for TTNtvs to become more clinically actionable.
In aggregate, missense variants in TTN are not enriched in DCM patients even when predicted to be deleterious [147]. However, there is evidence of segregation (where variant carriers present with disease in affected families) for specific TTN missense variants in DCM (c.2926 T > C (p.Trp976Arg); c.533C > A (p.Ala178Asp); and c.11674 T > A (p.Cys3892Ser)) [66, 148]. The molecular mechanisms by which these variants may predispose individuals to DCM requires investigation.
Discussion: Future Directions and Therapeutic Opportunities
Over 100 genetic loci have been identified with common variants associated with HF and tens of genes with protein-altering variants have definitive evidence for causing cardiomyopathy-induced HF. The different HF subgroups have heterogeneous genetic influences; HFpEF has the lowest estimated heritability and associates with few genetic loci compared to HFrEF and less specific HF grou**s. Improved sample size and patient stratification will aid our understanding of this in future studies. With this improved understanding of the genetic factors influencing HF, cardiac and extracardiac (e.g., kidney, vascular, and metabolic) tissue components as well as cellular and risk factor-associated molecular mechanisms are being identified as treatment targets.
Some of the genes with definitive evidence of rare, protein-altering variants causing cardiomyopathies and HF are identifiable at GWAS (e.g., BAG3, TTN, MYBPC3, FLNC, PLN), however, the absence of others is likely due to statistical power. With more whole genome sequencing, a holistic approach to discovering novel, common variant loci with confirmatory assessments of rare variants at the same locus via a burden analysis may provide further confirmation of which loci would be most important for targeted efforts for future HF therapy and would reflect the complex and diverse genetic architecture of cardiomyopathies [149, 150].
The analyses of larger structural variants (such as CNVs in FHOD3) and combinations of variants (oligogenic inheritance) may account for a proportion of cardiomyopathy that is genotype negative [129]. One crucial challenge in treating patients with HCM and DCM is ascertaining an early diagnosis to impose primary prevention of HF. The use of GRS composed of SNPs associated with DCM and HCM at GWAS may have clinical potential as diagnostic biomarkers [151, 152] and may be leveraged clinically for patients who are carriers of known pathogenic variants to predict the severity and prognosis of cardiomyopathies [153]. Notably, controlled diastolic blood pressure reduces the risk of develo** sarcomere-negative HCM, a condition influenced by common variants and challenging to diagnose at an early stage [27]. With our improved understanding of the common and rare genetic influences over HF, treatments targeting the mechanisms of action of the largest effect genetic loci are required.
With increasing knowledge of the genes implicated in cardiomyopathy and subsequent HF, the use of multiomic analyses to decipher the molecular mechanisms by which such genetic variants cause cardiac dysfunction may enable disease-modifying HF therapeutics to be developed. Furthermore, single-cell transcriptomic and proteomic analyses of HF heart samples may help identify potential biomarkers of prognostic significance, enabling appropriate risk stratification and personalised management of patients with HF [154, 155]. The DCM heart atlas is a point of reference here [156].
CRISPR-Cas 9-based gene editing holds the potential to reverse diseases caused by specific genetic variants. It may be instrumental in managing cardiomyopathy-induced HF caused by rare variants and pre-clinical models have shown benefit in reversing TTNtv-induced contractile dysfunction [145]. A recent study using adenine base editors and Cas-9 to inactivate the pathogenic myosin R403Q allele in mice prevented the development of HCM [157, 158]. However, results from more extensive trials with longer follow-up will be keenly awaited as well as pipelines for high throughput production for rare variants found in small numbers of patients.
Pharmacogenetic studies in HF have mainly assessed variants affecting the sympathetic nervous system response [159,160,161]. Improved understanding of how genetic variants influence response to HF therapy could greatly improve outcomes by better prediction of patients unlikely to respond to the therapy. Trial cohorts provide the ideal data source for these studies [162]. Pharmacogenetic studies looking at the effect of common variants in response to SGLT2 inhibitors and angiotensin receptor neprilysin inhibitors may provide clinically valuable information. Similarly, genoty** of CYP2C19 in patients with HCM treated with mavacamten, a novel cardiac myosin inhibitor, would aid dose tailoring and may improve outcomes [163]. Whether HFpEF patients benefit from Mavacamten is currently being evaluated (NCT04766892) and may guide future therapy in HFpEF [164]. The benefit may be most in HFpEF patients with a shared genetic architecture with HCM.
Further studies are needed to assess the impact of the coinheritance of multiple variants on disease development, severity and their subsequent impact on prognosis and response to therapy. Whether there are recurrent combinations of genetic variants in an oligogenic fashion, remains elusive. Allelic imbalance, where allele expression is altered for one allele compared to the other, may also contribute to the incomplete penetrance and variable expressivity observed in cardiomyopathies [165, 166].
Estimates of the prevalence of cardiomyopathies and genetic studies to date are dominated by European participants. Biases aside, the linkage disequilibrium within participants of European ancestry allows for improved statistical power in identifying variants that are associated with disease at GWAS. Large biobanks including patients of more diverse ancestry are required to improve the generalization of genetic results across the globe and for GRS to be applied globally. Importantly, future multi-ancestry biobanks would allow for improved curation of rare variants identified in non-European ancestries as it is likely some variants that are observed rarely in European patients are common in other ancestries and are less pathogenic than previously expected [167].
The genetic association analyses of HF and cardiomyopathies contribute to our understanding of incomplete penetrance. To improve diagnostic yield, our understanding of penetrance for individual variants is required to fully utilize the promises of genetics for cardiovascular disease [168, 169]. Eventually coupling genomics with metabolomics, transcriptomics and proteomics, will facilitate a better understanding of the molecular mechanisms by which variants cause cardiomyopathy and subsequent HF. Incorporation of genetics into multiparametric risk stratification models for cardiomyopathy patients with future penetrance estimates will facilitate more personalised management, better selection of patients for advanced therapies, and improve patient outcomes.
Conclusion
The advent of next-generation sequencing and GWAS has enhanced our understanding of the genes involved in HF. Common and rare genetic variants have been identified that are associated with HF as well as the risk factors and conditions that progress to HF. Recent GWAS and investigations into the biological mechanisms of TTNtvs have aided our understanding of the genetic underpinnings of HF and cardiomyopathy. Future work is required to validate the genes implicated in HF, identify novel therapeutic targets, and link specific variants to clinical outcomes through estimates of penetrance.
References
Lippi G, Sanchis-Gomar F. Global epidemiology and future trends of heart failure. AME Med J. 2020;5. https://doi.org/10.21037/amj.2020.03.03.
Benjamin E, Muntner P, Alonso A, Bittencourt M, Callaway C, Carson A. Heart disease and stroke Statistics—2019 update: A report from the american heart association. Circulation. 2019;139:e56–e528.
Lee DS, Pencina MJ, Benjamin EJ, Wang TJ, Levy D, O’Donnell CJ. Association of parental heart failure with risk of heart failure in offspring. N Engl J Med. 2006;355:138–47.
Lindgren MP, PirouziFard M, Smith JG, Sundquist J, Sundquist K, Zöller B. A swedish nationwide adoption study of the heritability of heart failure. JAMA Cardiol. 2018;3:703–10.
Tayal U, Prasad S, Cook SA. Genetics and genomics of dilated cardiomyopathy and systolic heart failure. Genome Med. 2017;9:20.
Czepluch FS, Wollnik B, Hasenfuß G. Genetic determinants of heart failure: Facts and numbers. ESC Heart Failure. 2018;5:211–7.
Neininger-Castro AC, Hayes JB, Sanchez ZC, Taneja N, Fenix AM, Moparthi S, Vassilopoulos S, Burnette DT. Independent regulation of Z-lines and M-lines during sarcomere assembly in cardiac myocytes revealed by the automatic image analysis software sarcApp. bioRxiv. 2023. https://doi.org/10.1101/2023.01.11.523681.
Burbaum L, Schneider J, Scholze S, Böttcher RT, Baumeister W, Schwille P, Plitzko JM, Jasnin M. Molecular-scale visualization of sarcomere contraction within native cardiomyocytes. Nat Commun. 2021;12:4086.
Takasaki A, Hirono K, Hata Y, Wang C, Takeda M, Yamashita JK, Chang B, Nakaoka H, Okabe M, Miyao N, Saito K, Ibuki K, Ozawa S, Sekine M, Yoshimura N, Nishida N, Bowles NE, Ichida F. Sarcomere gene variants act as a genetic trigger underlying the development of left ventricular noncompaction. Pediatr Res. 2018;84:733–42.
Powers JD, Malingen SA, Regnier M, Daniel TL. The Sliding Filament Theory Since Andrew Huxley: Multiscale and Multidisciplinary Muscle Research. Annu Rev Biophys. 2021;50:373–400.
Kumar S, Kumar V, Kim J-J. Sarcomeric Gene Variants and Their Role with Left Ventricular Dysfunction in Background of Coronary Artery Disease. Biomolecules. 2020;10:442.
Takemura G, Fujiwara H, Yoshida H, Mukoyama M, Saito Y, Nakao K, Fujiwara T, Uegaito T, Imura H, Kawai C. Identification and distribution of atrial natriuretic polypeptide in ventricular myocardium of humans with myocardial infarction. J Pathol. 1990;161:285–92.
Ho CY. Genetic considerations in hypertrophic cardiomyopathy. Prog Cardiovasc Dis. 2012;54:456–60.
McNally EM, Golbus JR, Puckelwartz MJ. Genetic mutations and mechanisms in dilated cardiomyopathy. J Clin Invest. 2013;123:19–26.
Schultheiss H-P, Fairweather D, Caforio ALP, Escher F, Hershberger RE, Lipshultz SE, Liu PP, Matsumori A, Mazzanti A, McMurray J, Priori SG. Dilated cardiomyopathy. Nat Rev Dis Primers. 2019;5:32.
Seferovic PM, Polovina M, Bauersachs J, Arad M, Ben Gal T, Lund LH. Heart failure in cardiomyopathies: A position paper from the heart failure association of the european society of cardiology. Eur J Heart Fail. 2019;21:553–76.
Felker GM, Thompson RE, Hare JM, Hruban RH, Clemetson DE, Howard DL, Baughman KL, Kasper EK. Underlying Causes and Long-Term Survival in Patients with Initially Unexplained Cardiomyopathy. N Engl J Med. 2000;342:1077–84.
de Marvao A, McGurk KA, Zheng SL, Thanaj M, Bai W, Duan J, Biffi C, Mazzarotto F, Statton B, Dawes TJW, Savioli N, Halliday BP, Xu X, Buchan RJ, Baksi AJ, Quinlan M, Tokarczuk P, Tayal U, Francis C, Whiffin N, Theotokis PI, Zhang X, Jang M, Berry A, Pantazis A, Barton PJR, Rueckert D, Prasad SK, Walsh R, Ho CY, Cook SA, Ware JS, O’Regan DP. Phenotypic Expression and Outcomes in Individuals With Rare Genetic Variants of Hypertrophic Cardiomyopathy. J Am Coll Cardiol. 2021;78:1097–110.
Chen Q-F, Hu J, Hu J, Nijjar PS, Xu J, Shi S, Liang D, Liao H, Gao J, Lin W-H, You S, Zhou X-D. Clinical characteristics and prognosis of patients with hypertrophic cardiomyopathy and heart failure with preserved ejection fraction. Clin Res Cardiol. 2024;113:761–69.
Hershberger RE, Parks SB, Kushner JD, Li D, Ludwigsen S, Jakobs P. Coding sequence mutations identified in MYH7, TNNT2, SCN5A, CSRP3, LBD3, and TCAP from 313 patients with familial or idiopathic dilated cardiomyopathy. Clin Transl Sci. 2008;1:21–6.
Bailey-Wilson JE, Wilson AF. Linkage Analysis in the Next-Generation Sequencing Era. Hum Hered. 2011;72:228–36.
Ott J, Wang J, Leal SM. Genetic linkage analysis in the age of whole-genome sequencing. Nat Rev Genet. 2015;16:275–84.
McGurk KA, Qiao M, Zheng SL, Sau A, Henry A, Ribeiro ALP, Ribeiro AH, Ng FS, Lumbers RT, Bai W, Ware JS, O’Regan DP. Genetic and phenotypic architecture of human myocardial trabeculation. medRxiv. 2023. https://doi.org/10.1101/2024.03.26.24304726.
Visscher PM, Brown MA, McCarthy MI, Jian YANG. Five years of GWAS discovery. Am J Hum Genet. 2012;90:7–24.
Wain LV. Rare variants and cardiovascular disease. Brief Funct Genomics. 2014;13:384–91.
Shoaib A, Farag M, Nolan J, Rigby A, Patwala A, Rashid M. Mode of presentation and mortality amongst patients hospitalized with heart failure? A report from the first euro heart failure survey. Clin Res Cardiol. 2019;108:510–9.
Harper AR, Goel A, Grace C, Thomson KL, Petersen SE, Xu X. Common genetic variants and modifiable risk factors underpin hypertrophic cardiomyopathy susceptibility and expressivity. Nat Genet. 2021;53:135–42.
Watkins H, Ashrafian H, Redwood C. Inherited cardiomyopathies. N Engl J Med. 2011;364:1643–56.
Arbelo E, Protonotarios A, Gimeno JR, Arbustini E, Barriales-Villa R, Basso C, Bezzina CR, Biagini E, Blom NA, Boer RA de, De Winter T, Elliott PM, Flather M, Garcia-Pavia P, Haugaa KH, Ingles J, Jurcut RO, Klaassen S, Limongelli G, Loeys B, Mogensen J, Olivotto I, Pantazis A, Sharma S, Van Tintelen JP, Ware JS, Kaski JP, ESC Scientific Document Group. ESC Guidelines for the management of cardiomyopathies. Eur Heart J. 2023;2023(44):3503–626.
Behjati S, Tarpey PS. What is next generation sequencing? Arch Dis Child Educ Pract Ed. 2013;98:236–8.
Smith LD, Willig LK, Kingsmore SF. Whole-Exome Sequencing and Whole-Genome Sequencing in Critically Ill Neonates Suspected to Have Single-Gene Disorders. Cold Spring Harb Perspect Med. 2015;6: a023168.
Bick D, Dimmock D. Whole exome and whole genome sequencing. Curr Opin Pediatr. 2011;23:594–600.
Mazzarotto F, Olivotto I, Walsh R. Advantages and Perils of Clinical Whole-Exome and Whole-Genome Sequencing in Cardiomyopathy. Cardiovasc Drugs Ther. 2020;34:241–53.
Bagnall RD, Ingles J, Dinger ME, Cowley MJ, Ross SB, Minoche AE, Lal S, Turner C, Colley A, Rajagopalan S, Berman Y, Ronan A, Fatkin D, Semsarian C. Whole Genome Sequencing Improves Outcomes of Genetic Testing in Patients With Hypertrophic Cardiomyopathy. J Am Coll Cardiol. 2018;72:419–29.
Ingles J, Goldstein J, Thaxton C, Caleshu C, Corty EW, Crowley SB, Dougherty K, Harrison SM, McGlaughon J, Milko LV, Morales A, Seifert BA, Strande N, Thomson K, Peter van Tintelen J, Wallace K, Walsh R, Wells Q, Whiffin N, Witkowski L, Semsarian C, Ware JS, Hershberger RE, Funke B. Evaluating the Clinical Validity of Hypertrophic Cardiomyopathy Genes. Circ Genom Precis Med. 2019;12:e002460.
Jordan E, Peterson L, Ai T, Asatryan B, Bronicki L, Brown E, Celeghin R, Edwards M, Fan J, Ingles J, James CA, Jarinova O, Johnson R, Judge DP, Lahrouchi N, Lekanne Deprez RH, Lumbers RT, Mazzarotto F, Medeiros Domingo A, Miller RL, Morales A, Murray B, Peters S, Pilichou K, Protonotarios A, Semsarian C, Shah P, Syrris P, Thaxton C, van Tintelen JP, Walsh R, Wang J, Ware J, Hershberger RE. Evidence-Based Assessment of Genes in Dilated Cardiomyopathy. Circulation. 2021;144:7–19.
Cappola TP, Li M, He J, Ky B, Gilmore J, Qu L, Keating B, Reilly M, Kim CE, Glessner J, Frackelton E, Hakonarson H, Syed F, Hindes A, Matkovich SJ, Cresci S, Dorn GW. Common variants in HSPB7 and FRMD4B associated with advanced heart failure. Circ Cardiovasc Genet. 2010;3:147–54.
Whiffin N, Minikel E, Walsh R, O’Donnell-Luria AH, Karczewski K, Ing AY, Barton PJR, Funke B, Cook SA, MacArthur D, Ware JS. Using high-resolution variant frequencies to empower clinical genome interpretation. Genet Med. 2017;19:1151–8.
Shah S, Henry A, Roselli C, Lin H, Sveinbjörnsson G, Fatemifar G, Hedman ÅK, Wilk JB, Morley MP, Chaffin MD, Helgadottir A, Verweij N, Dehghan A, Almgren P, Andersson C, Aragam KG, Ärnlöv J, Backman JD, Biggs ML, Bloom HL, Brandimarto J, Brown MR, Buckbinder L, Carey DJ, Chasman DI, Chen X, Chen X, Chung J, Chutkow W, Cook JP, Delgado GE, Denaxas S, Doney AS, Dörr M, Dudley SC, Dunn ME, Engström G, Esko T, Felix SB, Finan C, Ford I, Ghanbari M, Ghasemi S, Giedraitis V, Giulianini F, Gottdiener JS, Gross S, Guðbjartsson DF, Gutmann R, Haggerty CM, van der Harst P, Hyde CL, Ingelsson E, Jukema JW, Kavousi M, Khaw K-T, Kleber ME, Køber L, Koekemoer A, Langenberg C, Lind L, Lindgren CM, London B, Lotta LA, Lovering RC, Luan J, Magnusson P, Mahajan A, Margulies KB, März W, Melander O, Mordi IR, Morgan T, Morris AD, Morris AP, Morrison AC, Nagle MW, Nelson CP, Niessner A, Niiranen T, O’Donoghue ML, Owens AT, Palmer CNA, Parry HM, Perola M, Portilla-Fernandez E, Psaty BM, Rice KM, Ridker PM, Romaine SPR, Rotter JI, Salo P, Salomaa V, van Setten J, Shalaby AA, Smelser DT, Smith NL, Stender S, Stott DJ, Svensson P, Tammesoo M-L, Taylor KD, Teder-Laving M, Teumer A, Thorgeirsson G, Thorsteinsdottir U, Torp-Pedersen C, Trompet S, Tyl B, Uitterlinden AG, Veluchamy A, Völker U, Voors AA, Wang X, Wareham NJ, Waterworth D, Weeke PE, Weiss R, Wiggins KL, **ng H, Yerges-Armstrong LM, Yu B, Zannad F, Zhao JH, Hemingway H, Samani NJ, McMurray JJV, Yang J, Visscher PM, Newton-Cheh C, Malarstig A, Holm H, Lubitz SA, Sattar N, Holmes MV, Cappola TP, Asselbergs FW, Hingorani AD, Kuchenbaecker K, Ellinor PT, Lang CC, Stefansson K, Smith JG, Vasan RS, Swerdlow DI, Lumbers RT. Genome-wide association and Mendelian randomisation analysis provide insights into the pathogenesis of heart failure. Nat Commun. 2020;11:163.
Levin MG, Tsao NL, Singhal P, Liu C, Vy HMT, Paranjpe I, Backman JD, Bellomo TR, Bone WP, Biddinger KJ, Hui Q, Dikilitas O, Satterfield BA, Yang Y, Morley MP, Bradford Y, Burke M, Reza N, Charest B, Center Regeneron Genetics, Judy RL, Puckelwartz MJ, Hakonarson H, Khan A, Kottyan LC, Kullo I, Luo Y, McNally EM, Rasmussen-Torvik LJ, Day SM, Do R, Phillips LS, Ellinor PT, Nadkarni GN, Ritchie MD, Arany Z, Cappola TP, Margulies KB, Aragam KG, Haggerty CM, Joseph J, Sun YV, Voight BF, Damrauer SM. Genome-wide association and multi-trait analyses characterize the common genetic architecture of heart failure. Nat Commun. 2022;13:6914.
Joseph J, Liu C, Hui Q, Aragam K, Wang Z, Charest B, Huffman JE, Keaton JM, Edwards TL, Demissie S, Djousse L, Casas JP, Gaziano JM, Cho K, Wilson PWF, Phillips LS, O’Donnell CJ, Sun YV. Genetic architecture of heart failure with preserved versus reduced ejection fraction. Nat Commun. 2022;13:7753.
Henry A, Mo X, Finan C, Chaffin MD, Speed D, Issa H et al. HERMES Consortium. Map** the aetiological foundations of the heart failure spectrum using human genetics. medRxiv. 2023. https://doi.org/10.1101/2023.10.01.23296379
Franco D, Sedmera D, Lozano-Velasco E. Multiple Roles of Pitx2 in Cardiac Development and Disease. J Cardiovasc Dev Dis. 2017;4:16.
Chinchilla A, Daimi H, Lozano-Velasco E, Dominguez JN, Caballero R, Delpón E, Tamargo J, Cinca J, Hove-Madsen L, Aranega AE, Franco D. PITX2 insufficiency leads to atrial electrical and structural remodeling linked to arrhythmogenesis. Circ Cardiovasc Genet. 2011;4:269–79.
Zhang L, Smyth D, Al-Khalaf M, Blet A, Du Q, Bernick J, Gong M, Chi X, Oh Y, Roba-Oshin M, Coletta E, Feletou M, Gramolini AO, Kim K-H, Coutinho T, Januzzi JL, Tyl B, Ziegler A, Liu PP. Insulin-like growth factor-binding protein-7 (IGFBP7) links senescence to heart failure. Nat Cardiovasc Res. 2022;1:1195–214.
Bonaventura J, Rowin EJ, Maron MS, Maron BJ. Is Hypertrophic Cardiomyopathy Always a Familial and Inherited Disease? J Am Heart Assoc. 2023;12: e028974.
Maron BA, Wang R-S, Carnethon MR, Rowin EJ, Loscalzo J, Maron BJ, Maron MS. What Causes Hypertrophic Cardiomyopathy? Am J Cardiol. 2022;179:74–82.
Chou C, Chin MT. Pathogenic Mechanisms of Hypertrophic Cardiomyopathy beyond Sarcomere Dysfunction. Int J Mol Sci. 2021;22:8933.
Marian A, Braunwald E. Hypertrophic cardiomyopathy: Genetics, pathogenesis, clinical manifestations, diagnosis, and therapy. Circ Res. 2017;121:749–70.
Gyftopoulos A, Chen Y, Wang L, Williams CH, Chun YW, Perry JA, Hong CC. Abstract 460: cyclin dependent kinase inhibitor A1 identified as a potential risk locus for hypertrophic cardiomyopathy. Cir Res. 2020;127. https://doi.org/10.1161/res.127.suppl_1.460.
Meulen MH van der, Herkert JC, Boer SL den, Marchie Sarvaas GJ du, Blom NA, Ten Harkel ADJ, Breur HMPJ, Rammeloo LAJ, Tanke RB, Marcelis C, Laar IMBH van de, Verhagen JMA, Lekanne Dit Deprez RH, Barge-Schaapveld DQCM, Baas AF, Sammani A, Christiaans I, Tintelen JP van, Dalinghaus M. Genetic evaluation of a nation-wide dutch pediatric DCM cohort: the use of genetic testing in risk stratification. Circ Genom Precis Med. 2022;15:e002981.
Aung N, Lopes LR, van Duijvenboden S, Harper AR, Goel A, Grace C, Ho CY, Weintraub WS, Kramer CM, Neubauer S, Watkins HC, Petersen SE, Munroe PB. Genome-Wide Analysis of Left Ventricular Maximum Wall Thickness in the UK Biobank Cohort Reveals a Shared Genetic Background With Hypertrophic Cardiomyopathy. Circ Genom Precis Med. 2023;16: e003716.
Tadros R, Zheng SL, Grace C, Jorda P, Francis C, Jurgens SJ, Thomson KL, Harper AR, Wilde AA, Olivotto I, Adler A, Goel A, Ware JS, Bezzina CR, Watkins H. Large scale genome-wide association analyses identify novel genetic loci and mechanisms in hypertrophic cardiomyopathy. Eur Heart J. 2023;44. https://doi.org/10.1093/eurheartj/ehad655.3197.
Pirruccello JP, Bick A, Wang M, Chaffin M, Friedman S, Yao J. Analysis of cardiac magnetic resonance imaging in 36,000 individuals yields genetic insights into dilated cardiomyopathy. Nature Communications 2020;11. https://doi.org/10.1038/s41467-020-15823-7.
Garnier S, Harakalova M, Weiss S, Mokry M, Regitz-Zagrosek V, Hengstenberg C. Genome-wide association analysis in dilated cardiomyopathy reveals two new players in systolic heart failure on chromosomes 3p25.1 and 22q11.23. Eur Heart J. 2021;42:2000–11.
Ripps H, Shen W. Review: Taurine: A ‘very essential’ amino acid. Mol Vis. 2012;18:2673–86.
Ansar M, Ranza E, Shetty M, Paracha SA, Azam M, Kern I. Taurine treatment of retinal degeneration and cardiomyopathy in a consanguineous family with SLC6A6 taurine transporter deficiency. Hum Mol Genet. 2020;29:618–23.
McGurk KA, Kasapi M, Ware JS. Effect of taurine administration on symptoms, severity, or clinical outcome of dilated cardiomyopathy and heart failure in humans: A systematic review. Wellcome Open Research 2022;7. https://doi.org/10.12688/wellcomeopenres.17505.1.
Schaffer SW, Jong CJ, Ramila KC, Azuma J. Physiological roles of taurine in heart and muscle. J Biomed Sci. 2010;17(Suppl 1):S2.
Singh P, Gollapalli K, Mangiola S, Schranner D, Yusuf MA, Chamoli M. Taurine deficiency as a driver of aging. Science 2023. https://doi.org/10.1126/science.abn9257.
Zheng S, Henry A, Cannie D, Lee M, Miller D, McGurk K et al. Genome-wide association analysis reveals insights into the molecular aetiology underlying dilated cardiomyopathy. medRxiv. 2023. https://doi.org/10.1101/2023.09.28.23295408.
Parvatiyar MS, Brownstein AJ, Kanashiro-Takeuchi RM, Collado DJ JR, KM G, J H, KG M, JL F, A B, AM C, JS RP, J C, R.H. Stabilization of the cardiac sarcolemma by sarcospan rescues DMD-associated cardiomyopathy. JCI Insight 2019;5. https://doi.org/10.1172/jci.insight.123855.
Tsubata S, Bowles KR, Vatta M, Zintz C, Titus J, Muhonen L, Bowles NE, Towbin JA. Mutations in the human δ-sarcoglycan gene in familial and sporadic dilated cardiomyopathy. J Clin Investig. 2000;106:655–62.
Povysil G, Chazara O, Carss KJ, Deevi SVV, Wang Q, Armisen J. Assessing the role of rare genetic variation in patients with heart failure. JAMA cardiology. 2021;6:379–86.
Panoutsopoulou K, Tachmazidou I, Zeggini E. In search of low-frequency and rare variants affecting complex traits. Hum Mol Genet. 2013;22:R16–21.
Lopes LR, Barbosa P, Torrado M, Quinn E, Merino A, Ochoa JP. Cryptic splice-altering variants in MYBPC3 are a prevalent cause of hypertrophic cardiomyopathy. Circulation Genomic Precision Med. 2020;13: e002905.
Josephs KS, Roberts AM, Theotokis P, Walsh R, Ostrowski PJ, Edwards M. Beyond gene-disease validity: capturing structured data on inheritance, allelic requirement, disease-relevant variant classes, and disease mechanism for inherited cardiac conditions. Genome Med. 2023;15:1–86.
Walsh R, Thomson KL, Ware JS, Funke BH, Woodley J, McGuire KJ. Reassessment of mendelian gene pathogenicity using 7,855 cardiomyopathy cases and 60,706 reference samples. Genet Med. 2017;19:192–203.
Burke MA, Cook SA, Seidman JG, Seidman CE. Clinical and mechanistic insights into the genetics of cardiomyopathy. J Am Coll Cardiol. 2016;68:2871–86.
Toepfer CN, Wakimoto H, Garfinkel AC, McDonough B, Liao D, Jiang J, Tai AC, Gorham JM, Lunde IG, Lun M, Lynch TL, McNamara JW, Sadayappan S, Redwood CS, Watkins HC, Seidman JG, Seidman CE. Hypertrophic cardiomyopathy mutations in MYBPC3 dysregulate myosin. Sci Transl Med. 2019;11:eaat1199.
Hesaraki M, Bora U, Pahlavan S, Salehi N, Mousavi SA, Barekat M, Rasouli SJ, Baharvand H, Ozhan G, Totonchi M. A Novel Missense Variant in Actin Binding Domain of MYH7 Is Associated With Left Ventricular Noncompaction. Front Cardiovasc Med. 2022;9: 839862.
Gao Y, Peng L, Zhao C. MYH7 in cardiomyopathy and skeletal muscle myopathy. Mol Cell Biochem 2023. https://doi.org/10.1007/s11010-023-04735-x.
McNally EM. Beta-myosin heavy chain gene mutations in familial hypertrophic cardiomyopathy: the usual suspect? Circ Res. 2002;90:246–7.
Park J, Packard EA, Levin MG, Judy RL, Damrauer SM, Day SM. A genome-first approach to rare variants in hypertrophic cardiomyopathy genes MYBPC3 and MYH7 in a medical biobank. Hum Mol Genet. 2022;31:827–37.
As H, Ad T, Aa G, N H, S K, J R, Jm Y, H W, F M, Nk L, Sg W, Ac P, Dl J, Sd C, Ea A, S S, Js W, J I, C S, M M, I O, Cy H, Sm D. Spatial and Functional Distribution of MYBPC3 Pathogenic Variants and Clinical Outcomes in Patients With Hypertrophic Cardiomyopathy. Circulation Genom Precision Med. 2020;13. https://doi.org/10.1161/CIRCGEN.120.002929.
Yousaf M, Khan WA, Shahzad K, Khan HN, Ali B, Hussain M, Awan FR, Mustafa H, Sheikh FN. Genetic Association of Beta-Myosin Heavy-Chain Gene (MYH7) with Cardiac Dysfunction. Genes (Basel). 2022;13:1554.
Yadav S, Sitbon YH, Kazmierczak K, Szczesna-Cordary D. Hereditary heart disease: pathophysiology, clinical presentation, and animal models of HCM, RCM, and DCM associated with mutations in cardiac myosin light chains. Pflugers Arch. 2019;471:683–99.
Kabaeva ZT, Perrot A, Wolter B, Dietz R, Cardim N, Correia JM, Schulte HD, Aldashev AA, Mirrakhimov MM, Osterziel KJ. Systematic analysis of the regulatory and essential myosin light chain genes: genetic variants and mutations in hypertrophic cardiomyopathy. Eur J Hum Genet. 2002;10:741–8.
Osborn DPS, Emrahi L, Clayton J, Tabrizi MT, Wan AYB, Maroofian R, Yazdchi M, Garcia MLE, Galehdari H, Hesse C, Shariati G, Mazaheri N, Sedaghat A, Goullée H, Laing N, Jamshidi Y, Tajsharghi H. Autosomal recessive cardiomyopathy and sudden cardiac death associated with variants in MYL3. Genet Med. 2021;23:787–92.
Claes GRF, van Tienen FHJ, Lindsey P, Krapels IPC, Helderman-van den Enden ATJM, Hoos MB, Barrois YEG, Janssen JWH, Paulussen ADC, Sels J-WEM, Kuijpers SHH, van Tintelen JP, van den Berg MP, Heesen WF, Garcia-Pavia P, Perrot A, Christiaans I, Salemink S, Marcelis CLM, Smeets HJM, Brunner HG, Volders PGA, van den Wijngaard A. Hypertrophic remodelling in cardiac regulatory myosin light chain (MYL2) founder mutation carriers. Eur Heart J. 2016;37:1815–22.
Wei B, ** J-P. TNNT1, TNNT2, and TNNT3: Isoform genes, regulation, and structure-function relationships. Gene. 2016;582:1–13.
Jj S, Jp J. TNNI1, TNNI2 and TNNI3: Evolution, regulation, and protein structure-function relationships. Gene. 2016;576. https://doi.org/10.1016/j.gene.2015.10.052.
van den Wijngaard A, Volders P, Van Tintelen JP, Jongbloed JDH, van den Berg MP, Lekanne Deprez RH, Mannens MMAM, Hofmann N, Slegtenhorst M, Dooijes D, Michels M, Arens Y, Jongbloed R, Smeets BJM. Recurrent and founder mutations in the Netherlands: cardiac Troponin I (TNNI3) gene mutations as a cause of severe forms of hypertrophic and restrictive cardiomyopathy. Neth Heart J. 2011;19:344–51.
England J, Granados-Riveron J, Polo-Parada L, Kuriakose D, Moore C, Brook JD. Tropomyosin 1: Multiple roles in the develo** heart and in the formation of congenital heart defects. J Mol Cell Cardiol. 2017. https://doi.org/10.1016/j.yjmcc.2017.03.006.
Frank D, Yusuf Rangrez A, Friedrich C, Dittmann S, Stallmeyer B, Yadav P, Bernt A, Schulze-Bahr E, Borlepawar A, Zimmermann W-H, Peischard S, Seebohm G, Linke WA, Baba HA, Krüger M, Unger A, Usinger P, Frey N, Schulze-Bahr E. Cardiac α-Actin (ACTC1) Gene Mutation Causes Atrial-Septal Defects Associated With Late-Onset Dilated Cardiomyopathy. Circ Genom Precis Med. 2019;12: e002491.
Aggarwal V, Dobrolet N, Fishberger S, Zablah J, Jayakar P, Ammous Z. PRKAG2 mutation: An easily missed cardiac specific non-lysosomal glycogenosis. Ann Pediatr Cardiol. 2015;8:153–6.
Porto AG, Brun F, Severini GM, Losurdo P, Fabris E, Taylor MRG, Mestroni L, Sinagra G. Clinical Spectrum of PRKAG2 Syndrome. Circ Arrhythm Electrophysiol. 2016;9: e003121.
Lopez-Sainz A, Dominguez F, Lopes LR, Ochoa JP, Barriales-Villa R, Climent V, Linschoten M, Tiron C, Chiriatti C, Marques N, Rasmussen TB, Espinosa MÁ, Beinart R, Quarta G, Cesar S, Field E, Garcia-Pinilla JM, Bilinska Z, Muir AR, Roberts AM, Santas E, Zorio E, Peña-Peña ML, Navarro M, Fernandez A, Palomino-Doza J, Azevedo O, Lorenzini M, García-Álvarez MI, Bento D, Jensen MK, Méndez I, Pezzoli L, Sarquella-Brugada G, Campuzano O, Gonzalez-Lopez E, Mogensen J, Kaski JP, Arad M, Brugada R, Asselbergs FW, Monserrat L, Olivotto I, Elliott PM, Garcia-Pavia P. European Genetic Cardiomyopathies Initiative Investigators. Clinical Features and Natural History of PRKAG2 Variant Cardiac Glycogenosis. J Am Coll Cardiol. 2020;76:186–97.
Maron BJ, Maron MS. PRKAG2 Glycogen Storage Disease Cardiomyopathy: Out of the Darkness and Into the Light. J Am Coll Cardiol. 2020;76:198–200.
Stankowski K, Figliozzi S, Battaglia V, Catapano F, Francone M, Monti L. Fabry Disease: More than a Phenocopy of Hypertrophic Cardiomyopathy. J Clin Med. 2023;12:7061.
Azevedo O, Marques N, Reis L, Cruz I, Craveiro N, Antunes H, Lourenço C, Gomes R, Guerreiro RA, Faria R, Sá F, Lima R, Gaspar P, Faria R, Miltenberger-Miltenyi G, Sousa N, Cunha D, group of investigators. Predictors of Fabry disease in patients with hypertrophic cardiomyopathy: How to guide the diagnostic strategy? Am Heart J. 2020;226:114–26.
Thiene G, Corrado D, Basso C. Cardiomyopathies: is it time for a molecular classification? Eur Heart J. 2004;25:1772–5.
Vio R, Angelini A, Basso C, Cipriani A, Zorzi A, Melacini P, Thiene G, Rampazzo A, Corrado D, Calore C. Hypertrophic Cardiomyopathy and Primary Restrictive Cardiomyopathy: Similarities Differences and Phenocopies. J Clin Med. 2021;10:1954.
Biagini E, Spirito P, Rocchi G, Ferlito M, Rosmini S, Lai F, Lorenzini M, Terzi F, Bacchi-Reggiani L, Boriani G, Branzi A, Boni L, Rapezzi C. Prognostic implications of the Doppler restrictive filling pattern in hypertrophic cardiomyopathy. Am J Cardiol. 2009;104:1727–31.
Topriceanu C, Pereira AC, Moon JC, Captur G, Ho CY. Meta-analysis of penetrance and systematic review on transition to disease in genetic hypertrophic cardiomyopathy. Circulation. 2024;149:107–23.
McGurk KA, Zhang X, Theotokis P, Thomson K, Harper A, Buchan RJ, Mazaika E, Ormondroyd E, Wright WT, Macaya D, Pua CJ, Funke B, MacArthur DG, Prasad S, Cook SA, Allouba M, Aguib Y, Yacoub MH, O’Regan DP, Barton PJR, Watkins H, Bottolo L, Ware JS. The penetrance of rare variants in cardiomyopathy-associated genes: a cross-sectional approach to estimate penetrance for secondary findings. Am J Hum Genet. 2023;110:1482–95.
Mazzarotto F, Tayal U, Buchan RJ, Midwinter W, Wilk A, Whiffin N, Govind R, Mazaika E, de Marvao A, Dawes TJW, Felkin LE, Ahmad M, Theotokis PI, Edwards E, Ing AY, Thomson KL, Chan LLH, Sim D, Baksi AJ, Pantazis A, Roberts AM, Watkins H, Funke B, O’Regan DP, Olivotto I, Barton PJR, Prasad SK, Cook SA, Ware JS, Walsh R. Reevaluating the Genetic Contribution of Monogenic Dilated Cardiomyopathy. Circulation. 2020;141:387–98.
Seidel F, Holtgrewe M, Al-Wakeel-Marquard N, Opgen-Rhein B, Dartsch J, Herbst C, Beule D, Pickardt T, Klingel K, Messroghli D, Berger F, Schubert S, Kühnisch J, Klaassen S. Pathogenic Variants Associated With Dilated Cardiomyopathy Predict Outcome in Pediatric Myocarditis. Circulation Genomic and Precision Medicine. 2021;14:e003250.
Genschel J, Schmidt HH. Mutations in the LMNA gene encoding lamin A/C. Hum Mutat. 2000;16:451–9.
Wang Y, Dobreva G. Epigenetics in LMNA-Related Cardiomyopathy Cells. 2023;12:783.
Wang S, Peng D. Case series: LMNA-related dilated cardiomyopathy presents with reginal wall akinesis and transmural late gadolinium enhancement. ESC Heart Fail. 2020;7:3179–83.
Qu H-Q, Feldman AM, Hakonarson H. Genetics of BAG3: A Paradigm for Develo** Precision Therapies for Dilated Cardiomyopathies. J Am Heart Assoc. 2022;11: e027373.
Domínguez F, Cuenca S, Bilińska Z, Toro R, Villard E, Barriales-Villa R, Ochoa JP, Asselbergs F, Sammani A, Franaszczyk M, Akhtar M, Coronado-Albi MJ, Rangel-Sousa D, Rodriguez-Palomares JF, Jiménez-Jáimez J, Garcia-Pinilla JM, Ripoll-Vera T, Mogollón-Jiménez MV, Fontalba-Romero A, Garcia-Medina D, Palomino-Doza J, de Gonzalo-Calvo D, Cicerchia M, Salazar-Mendiguchia J, Salas C, Pankuweit S, Hey TM, Mogensen J, Barton PJ, Charron P, Elliott P, Garcia-Pavia P. J Am Coll Cardiol. 2018;72:2471–81.
Villard E, Perret C, Dubourg O, Tavazzi L, Aumont M, Degroote P. A genome-wide association study identifies two loci associated with heart failure due to dilated cardiomyopathy. Eur Heart J. 2011;32:1065–76.
Perez-Bermejo JA, Judge LM, Jensen CL, Wu K, Watry HL, Truong A. Functional analysis of a common BAG3 allele associated with protection from heart failure. Nature Cardiovascular Research. 2023;2:615–28.
Perea-Gil I, Seeger T, Bruyneel AAN, Termglinchan V, Monte E, Lim EW, Vadgama N, Furihata T, Gavidia AA, Arthur Ataam J, Bharucha N, Martinez-Amador N, Ameen M, Nair P, Serrano R, Kaur B, Feyen DAM, Diecke S, Snyder MP, Metallo CM, Mercola M, Karakikes I. Serine biosynthesis as a novel therapeutic target for dilated cardiomyopathy. Eur Heart J. 2022;43:3477–89.
Ortiz-Genga MF, Cuenca S, Dal Ferro M, Zorio E, Salgado-Aranda R, Climent V, Padrón-Barthe L, Duro-Aguado I, Jiménez-Jáimez J, Hidalgo-Olivares VM, García-Campo E, Lanzillo C, Suárez-Mier MP, Yonath H, Marcos-Alonso S, Ochoa JP, Santomé JL, García-Giustiniani D, Rodríguez-Garrido JL, Domínguez F, Merlo M, Palomino J, Peña ML, Trujillo JP, Martín-Vila A, Stolfo D, Molina P, Lara-Pezzi E, Calvo-Iglesias FE, Nof E, Calò L, Barriales-Villa R, Gimeno-Blanes JR, Arad M, García-Pavía P, Monserrat L. Truncating FLNC Mutations Are Associated With High-Risk Dilated and Arrhythmogenic Cardiomyopathies. J Am Coll Cardiol. 2016;68:2440–51.
Verdonschot JAJ, Vanhoutte EK, Claes GRF, Helderman-van den Enden ATJM, Hoeijmakers JGJ, Hellebrekers DMEI, de Haan A, Christiaans I, Lekanne Deprez RH, Boen HM, van Craenenbroeck EM, Loeys BL, Hoedemaekers YM, Marcelis C, Kempers M, Brusse E, van Waning JI, Baas AF, Dooijes D, Asselbergs FW, Barge-Schaapveld DQCM, Koopman P, van den Wijngaard A, Heymans SRB, Krapels IPC, Brunner HG. A mutation update for the FLNC gene in myopathies and cardiomyopathies. Hum Mutat. 2020;41:1091–111.
Reinstein E, Gutierrez-Fernandez A, Tzur S, Bormans C, Marcu S, Tayeb-Fligelman E. Congenital dilated cardiomyopathy caused by biallelic mutations in filamin C. Eur J Human Gen : EJHG. 2016;24:1792–6.
Begay RL, Graw SL, Sinagra G, Asimaki A, Rowland TJ, Slavov DB. Filamin C truncation mutations are associated with arrhythmogenic Dilated Cardiomyopathy and changes in the Cell-Cell adhesion structures. JACC Clin Electrophysiol. 2018;4:504–14.
Ader F, De Groote P, Réant P, Rooryck-Thambo C, Dupin-Deguine D, Rambaud C, Khraiche D, Perret C, Pruny JF, Mathieu-Dramard M, Gérard M, Troadec Y, Gouya L, Jeunemaitre X, Van Maldergem L, Hagège A, Villard E, Charron P, Richard P. FLNC pathogenic variants in patients with cardiomyopathies: Prevalence and genotype-phenotype correlations. Clin Genet. 2019;96:317–29.
Pasotti M, Klersy C, Pilotto A, Rapezzi C, Serio A. Long-Term Outcome and Risk Stratification in Dilated Cardiolaminopathies. J Am College Cardiol. 2008;52:1250–60.
Bondue A, Arbustini E, Bianco A, Ciccarelli M, Dawson D, Rosa M. Complex roads from genotype to phenotype in dilated cardiomyopathy: scientific update from the Working Group of Myocardial Function of the European Society of Cardiology. Cardiovasc Res. 2018;114:1287–303.
Halliday B, Cleland J, Goldberger J, Prasad S. Personalizing risk stratification for sudden death in dilated cardiomyopathy: The past, present, and future. Circulation. 2017;136:215–31.
Brandão M, Bariani R, Rigato I, Bauce B. Desmoplakin Cardiomyopathy: Comprehensive Review of an Increasingly Recognized Entity. J Clin Med. 2023;12:2660.
Gregorich ZR, Zhang Y, Kamp TJ, Granzier HL, Guo W. Mechanisms of RBM20 Cardiomyopathy: Insights From Model Systems. Circ Genom Precis Med. 2024;17: e004355.
Eijgenraam TR, Boogerd CJ, Stege NM, Oliveira Nunes Teixeira V, Dokter MM, Schmidt LE, Yin X, Theofilatos K, Mayr M, van der Meer P, van Rooij E, van der Velden J, Silljé HHW, de Boer RA. Protein Aggregation Is an Early Manifestation of Phospholamban p. (Arg14del)-Related Cardiomyopathy: Development of PLN-R14del-Related Cardiomyopathy. Circ Heart Fail. 2021;14:e008532.
Vasireddi SK, Sattayaprasert P, Yang D, Dennis AT, Bektik E, Fu J-D, Mackall JA, Laurita KR. Adipogenic Signaling Promotes Arrhythmia Substrates before Structural Abnormalities in TMEM43 ARVC. J Pers Med. 2022;12:1680.
Baskin B, Skinner JR, Sanatani S, Terespolsky D, Krahn AD, Ray PN, Scherer SW, Hamilton RM. TMEM43 mutations associated with arrhythmogenic right ventricular cardiomyopathy in non-Newfoundland populations. Hum Genet. 2013;132:1245–52.
Milting H, Klauke B, Christensen AH, Müsebeck J, Walhorn V, Grannemann S, Münnich T, Šarić T, Rasmussen TB, Jensen HK, Mogensen J, Baecker C, Romaker E, Laser KT, Knyphausen zu E, Kassner A, Gummert J, Judge DP, Connors S, Hodgkinson K, Young T-L, Zwaag van der PA, Tintelen van JP, Anselmetti D. The TMEM43 Newfoundland mutation p. S358L causing ARVC-5 was imported from Europe and increases the stiffness of the cell nucleus. Eur Heart J. 2015;36:872–81.
Padrón-Barthe L, Villalba-Orero M, Gómez-Salinero JM, Domínguez F, Román M, Larrasa-Alonso J, Ortiz-Sánchez P, Martínez F, López-Olañeta M, Bonzón-Kulichenko E, Vázquez J, Martí-Gómez C, Santiago DJ, Prados B, Giovinazzo G, Gómez-Gaviro MV, Priori S, Garcia-Pavia P, Lara-Pezzi E. Severe Cardiac Dysfunction and Death Caused by Arrhythmogenic Right Ventricular Cardiomyopathy Type 5 Are Improved by Inhibition of Glycogen Synthase Kinase-3β. Circulation. 2019;140:1188–204.
de Frutos F, Ochoa JP, Navarro-Peñalver M, Baas A, Bjerre JV, Zorio E, Méndez I, Lorca R, Verdonschot JAJ, García-Granja PE, Bilinska Z, Fatkin D, Fuentes-Cañamero ME, García-Pinilla JM, García-Álvarez MI, Girolami F, Barriales-Villa R, Díez-López C, Lopes LR, Wahbi K, García-Álvarez A, Rodríguez-Sánchez I, Rekondo-Olaetxea J, Rodríguez-Palomares JF, Gallego-Delgado M, Meder B, Kubanek M, Hansen FG, Restrepo-Córdoba MA, Palomino-Doza J, Ruiz-Guerrero L, Sarquella-Brugada G, Perez-Perez AJ, Bermúdez-Jiménez FJ, Ripoll-Vera T, Rasmussen TB, Jansen M, Sabater-Molina M, Elliot PM, Garcia-Pavia P. European Genetic Cardiomyopathies Initiative Investigators. Natural History of MYH7-Related Dilated Cardiomyopathy. J Am Coll Cardiol. 2022;80:1447–61.
Tajsharghi H, Oldfors A. Myosinopathies: pathology and mechanisms. Acta Neuropathol. 2013;125:3–18.
Ujfalusi Z, Vera CD, Mijailovich SM, Svicevic M, Yu EC, Kawana M, Ruppel KM, Spudich JA, Geeves MA, Leinwand LA. Dilated cardiomyopathy myosin mutants have reduced force-generating capacity. J Biol Chem. 2018;293:9017–29.
Puckelwartz MJ, Pesce LL, Dellefave-Castillo LM, Wheeler MT, Pottinger TD, Robinson AC, Kearns SD, Gacita AM, Schoppen ZJ, Pan W, Kim G, Wilcox JE, Anderson AS, Ashley EA, Day SM, Cappola T, Dorn GW, McNally EM. Genomic Context Differs Between Human Dilated Cardiomyopathy and Hypertrophic Cardiomyopathy. J Am Heart Assoc. 2021;10: e019944.
Zheng SL, Jurgens SJ, McGurk KA, Xu X, Grace C, Theotokis PI et al. Evaluation of polygenic score for hypertrophic cardiomyopathy in the general population and across clinical settings. medRxiv. 2023. https://doi.org/10.1101/2023.03.14.23286621.
Desai MY, Owens A, Geske JB, Wolski K, Naidu SS, Smedira NG, Cremer PC, Schaff H, McErlean E, Sewell C, Li W, Sterling L, Lampl K, Edelberg JM, Sehnert AJ, Nissen SE. Myosin Inhibition in Patients With Obstructive Hypertrophic Cardiomyopathy Referred for Septal Reduction Therapy. J Am Coll Cardiol. 2022;80:95–108.
Taniguchi K, Takeya R, Suetsugu S, Kan-o M, Narusawa M, Shiose A. Mammalian formin Fhod3 regulates actin assembly and sarcomere organization in striated muscles. J Biol Chem. 2009;284:29873–81.
Ushijima T, Fujimoto N, Matsuyama S, Kan-o M, Kiyonari H, Shioi G. The actin-organizing formin protein Fhod3 is required for postnatal development and functional maintenance of the adult heart in mice. J Biol Chem. 2018;293:148–62.
Ochoa JP, Sabater-Molina M, García-Pinilla JM, Mogensen J, Restrepo-Córdoba A, Palomino-Doza J. Formin homology 2 domain containing 3 (FHOD3) is a genetic basis for hypertrophic cardiomyopathy. J Am Coll Cardiol. 2018;72:2457–67.
Ochoa JP, Lopes LR, Perez-Barbeito M, Cazón-Varela L, Torre-Carpente MM, Sonicheva-Paterson N. Deletions of specific exons of FHOD3 detected by next-generation sequencing are associated with hypertrophic cardiomyopathy. Clin Genet. 2020;98:86–90.
Wooten E, Hebl V, Wolf M, Greytak S, Orr N, Draper I. Formin homology 2 domain containing 3 variants associated with hypertrophic cardiomyopathy. Circ Cardiovasc Genet. 2013;6:10–8.
Piqueras-Flores J, Villacorta-Argüelles E, Galvin J, Climent-Payá V, Escobar-López LE, Amor-Salamanca A, Garcia-Hernandez S, Esmonde S, Martínez-Del Río J, Soto-Pérez M, Garcia-Pavia P, Ochoa JP. Intermediate-effect size p.Arg637Gln in FHOD3 increases risk of HCM and is associated with an aggressive phenotype in homozygous carriers. J Med Genet. 2024;61:423–27.
Ware JS, Li J, Mazaika E, Yasso CM, DeSouza T, Cappola TP, Tsai EJ, Hilfiker-Kleiner D, Kamiya CA, Mazzarotto F, Cook SA, Halder I, Prasad SK, Pisarcik J, Hanley-Yanez K, Alharethi R, Damp J, Hsich E, Elkayam U, Sheppard R, Kealey A, Alexis J, Ramani G, Safirstein J, Boehmer J, Pauly DF, Wittstein IS, Thohan V, Zucker MJ, Liu P, Gorcsan J, McNamara DM, Seidman CE, Seidman JG, Arany Z. Shared Genetic Predisposition in Peripartum and Dilated Cardiomyopathies. N Engl J Med. 2016;374:233–41.
Ware JS, Amor-Salamanca A, Tayal U, Govind R, Serrano I, Salazar-Mendiguchía J, García-Pinilla JM, Pascual-Figal DA, Nuñez J, Guzzo-Merello G, Gonzalez-Vioque E, Bardaji A, Manito N, López-Garrido MA, Padron-Barthe L, Edwards E, Whiffin N, Walsh R, Buchan RJ, Midwinter W, Wilk A, Prasad S, Pantazis A, Baski J, O’Regan DP, Alonso-Pulpon L, Cook SA, Lara-Pezzi E, Barton PJ, Garcia-Pavia P. Genetic Etiology for Alcohol-Induced Cardiac Toxicity. J Am Coll Cardiol. 2018;71:2293–302.
Garcia-Pavia P, Kim Y, Restrepo-Cordoba MA, Lunde IG, Wakimoto H, Smith AM, Toepfer CN, Getz K, Gorham J, Patel P, Ito K, Willcox JA, Arany Z, Li J, Owens AT, Govind R, Nuñez B, Mazaika E, Bayes-Genis A, Walsh R, Finkelman B, Lupon J, Whiffin N, Serrano I, Midwinter W, Wilk A, Bardaji A, Ingold N, Buchan R, Tayal U, Pascual-Figal DA, de Marvao A, Ahmad M, Garcia-Pinilla JM, Pantazis A, Dominguez F, John Baksi A, O’Regan DP, Rosen SD, Prasad SK, Lara-Pezzi E, Provencio M, Lyon AR, Alonso-Pulpon L, Cook SA, DePalma SR, Barton PJR, Aplenc R, Seidman JG, Ky B, Ware JS, Seidman CE. Genetic Variants Associated With Cancer Therapy-Induced Cardiomyopathy. Circulation. 2019;140:31–41.
Herman DS, Lam L, Taylor MRG, Wang L, Teekakirikul P, Christodoulou D, Conner L, DePalma SR, McDonough B, Sparks E, Teodorescu DL, Cirino AL, Banner NR, Pennell DJ, Graw S, Merlo M, Di Lenarda A, Sinagra G, Bos JM, Ackerman MJ, Mitchell RN, Murry CE, Lakdawala NK, Ho CY, Barton PJR, Cook SA, Mestroni L, Seidman JG, Seidman CE. Truncations of Titin Causing Dilated Cardiomyopathy. N Engl J Med. 2012;366:619–28.
Roberts AM, Ware JS, Herman DS, Schafer S, Baksi J, Bick AG, Buchan RJ, Walsh R, John S, Wilkinson S, Mazzarotto F, Felkin LE, Gong S, MacArthur LJA, Cunningham F, Flannick J, Gabriel SB, Altshuler DM, Macdonald PS, Heinig M, Keogh AM, Hayward CS, Banner NR, Pennell DJ, O’Regan DP, San TR, de Marvao A, Dawes WTJ, Gulati A, Birks EJ, Yacoub MH, Radke M, Gotthardt M, Wilson JG, O’Donnell CJ, Prasad SK, Barton RPJ, Fatkin D, Hubner N, Seidman JG, Seidman CE, Cook SA. Integrated allelic, transcriptional, and phenomic dissection of the cardiac effects of titin truncations in health and disease. Sci Translational Med. 2015;7:270ra6-270ra6.
Golbus JR, Puckelwartz MJ, Fahrenbach JP, Dellefave-Castillo LM, Wolfgeher D, McNally EM. Population-Based Variation in Cardiomyopathy Genes. Circulation: Cardiovascular Genetics. 2012;5:391–9.
Pan S, Caleshu CA, Dunn KE, Foti MJ, Moran MK, Soyinka O, Ashley EA. Cardiac Structural and Sarcomere Genes Associated With Cardiomyopathy Exhibit Marked Intolerance of Genetic Variation. Circulation: Cardiovascular Genetics. 2012;5:602–10.
Tharp CA, Haywood ME, Sbaizero O, Taylor MRG, Mestroni L. The giant protein titin’s role in cardiomyopathy: genetic, transcriptional, and post-translational modifications of TTN and their contribution to cardiac disease. Front Physiol. 2019;10:1436.
Schafer S, de Marvao A, Adami E, Fiedler LR, Ng B, Khin E, Rackham OJL, van Heesch S, Pua CJ, Kui M, Walsh R, Tayal U, Prasad SK, Dawes TJW, Ko NSJ, Sim D, Chan LLH, Chin CWL, Mazzarotto F, Barton PJ, Kreuchwig F, de Kleijn DPV, Totman T, Biffi C, Tee N, Rueckert D, Schneider V, Faber A, Regitz-Zagrosek V, Seidman JG, Seidman CE, Linke WA, Kovalik J-P, O’Regan D, Ware JS, Hubner N, Cook SA. Titin-truncating variants affect heart function in disease cohorts and the general population. Nat Genet. 2017;49:46–53.
McAfee Q, Chen CY, Yang Y, Caporizzo MA, Morley M, Babu A, Jeong S, Brandimarto J, Bedi KC, Flam E, Cesare J, Cappola TP, Margulies K, Prosser B, Arany Z. Truncated titin proteins in dilated cardiomyopathy. Sci Translational Med. 2021;13:eabd7287.
Hinson JT, Chopra A, Nafissi N, Polacheck WJ, Benson CC, Swist S, Gorham J, Yang L, Schafer S, Sheng CC, Haghighi A, Homsy J, Hubner N, Church G, Cook SA, Linke WA, Chen CS, Seidman JG, Seidman CE. HEART DISEASE. Titin mutations in iPS cells define sarcomere insufficiency as a cause of dilated cardiomyopathy. Science. 2015;349:982–6.
Fomin A, Gärtner A, Cyganek L, Tiburcy M, Tuleta I, Wellers L, Folsche L, Hobbach AJ, von Frieling-Salewsky M, Unger A, Hucke A, Koser F, Kassner A, Sielemann K, Streckfuß-Bömeke K, Hasenfuss G, Goedel A, Laugwitz K-L, Moretti A, Gummert JF, Dos Remedios CG, Reinecke H, Knöll R, van Heesch S, Hubner N, Zimmermann WH, Milting H, Linke WA. Truncated titin proteins and titin haploinsufficiency are targets for functional recovery in human cardiomyopathy due to TTN mutations. Sci Transl Med. 2021;13:eabd3079.
Yotti R, Seidman CE, Seidman JG. Advances in the genetic basis and pathogenesis of sarcomere cardiomyopathies. Annu Rev Genomics Hum Genet. 2019;20:129–53.
Akinrinade O, Koskenvuo JW, Alastalo T-P. Prevalence of Titin Truncating Variants in General Population. PLoS ONE. 2015;10: e0145284.
Domínguez F, Lalaguna L, Martínez-Martín I, Piqueras-Flores J, Rasmussen TB, Zorio E, Giovinazzo G, Prados B, Ochoa JP, Bornstein B, González-López E, Velázquez-Carreras D, Pricolo MR, Gutiérrez-Agüera F, Bernal JA, Herrero-Galán E, Alegre-Cebollada J, Lara-Pezzi E, García-Pavía P. Titin Missense Variants as a Cause of Familial Dilated Cardiomyopathy. Circulation. 2023;147:1711–3.
Walsh R, Offerhaus JA, Taos R, Bezzina CR. Minor hypertrophic cardiomyopathy genes, major insights into the genetics of cardiomyopathies. Nat Rev Cardiol. 2021;19:151–67.
Chen W, Coombes BJ, Larson NB. Recent advances and challenges of rare variant association analysis in the biobank sequencing era. Front Genet. 2022;13:1014947.
Ingles J, Burns C, Bagnall R, Lam L, Yeates L, Sarina T. Nonfamilial hypertrophic cardiomyopathy: Prevalence, natural history, and clinical implications. Circ Cardiovasc Genet. 2017;10: e001620.
Dellefave L, McNally E. The genetics of dilated cardiomyopathy. Curr Opin Cardiol. 2010;25:198–204.
Tadros R, Francis C, Xu X, Vermeer AMC, Harper AR, Huurman R. Shared genetic pathways contribute to risk of hypertrophic and dilated cardiomyopathies with opposite directions of effect. Nat Genet. 2021;53:128–34.
Miranda AMA, Janbandhu V, Maatz H, Kanemaru K, Cranley J, Teichmann SA, Hübner N, Schneider MD, Harvey RP, Noseda M. Single-cell transcriptomics for the assessment of cardiac disease. Nat Rev Cardiol. 2022:1–20. https://doi.org/10.1038/s41569-022-00805-7.
Michelhaugh SA, Januzzi JL. Finding a Needle in a Haystack: Proteomics in Heart Failure. JACC Basic Transl Sci. 2020;5:1043–53.
Haas J, Frese KS, Peil B, Kloos W, Keller A, Nietsch R. Atlas of the clinical genetics of human dilated cardiomyopathy. Eur Heart J. 2015;36:1123–35.
Reichart D, Newby GA, Wakimoto H, Lun M, Gorham JM, Curran JJ, Raguram A, DeLaughter DM, Conner DA, Marsiglia JDC, Kohli S, Chmatal L, Page DC, Zabaleta N, Vandenberghe L, Liu DR, Seidman JG, Seidman C. Efficient in vivo genome editing prevents hypertrophic cardiomyopathy in mice. Nat Med. 2023;29:412–21.
Chai AC, Cui M, Chemello F, Li H, Chen K, Tan W, Atmanli A, McAnally JR, Zhang Y, Xu L, Liu N, Bassel-Duby R, Olson EN. Base editing correction of hypertrophic cardiomyopathy in human cardiomyocytes and humanized mice. Nat Med. 2023;29:401–11.
O’Connor CM, Fiuzat M, Carson PE, Anand IS, Plehn JF, Gottlieb SS, Silver MA, Lindenfeld J, Miller AB, White M, Walsh R, Nelson P, Medway A, Davis G, Robertson AD, Port JD, Carr J, Murphy GA, Lazzeroni LC, Abraham WT, Liggett SB, Bristow MR. Combinatorial pharmacogenetic interactions of bucindolol and β1, α2C adrenergic receptor polymorphisms. PLoS ONE. 2012;7: e44324.
Aleong RG, Sauer WH, Robertson AD, Liggett SB, Bristow MR. Adrenergic receptor polymorphisms and prevention of ventricular arrhythmias with bucindolol in patients with chronic heart failure. Circ Arrhythm Electrophysiol. 2013;6:137–43.
Kao DP, Davis G, Aleong R, O’Connor CM, Fiuzat M, Carson PE. Effect of bucindolol on heart failure outcomes and heart rate response in patients with reduced ejection fraction heart failure and atrial fibrillation. Eur J Heart Fail. 2013;15(3):324–33.
Reza N, Owens AT. Advances in the Genetics and Genomics of Heart Failure. Curr Cardiol Rep. 2020;22:132.
Spertus JA, Fine JT, Elliott P, Ho CY, Olivotto I, Saberi S, Li W, Dolan C, Reaney M, Sehnert AJ, Jacoby D. Mavacamten for treatment of symptomatic obstructive hypertrophic cardiomyopathy (EXPLORER-HCM): health status analysis of a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2021;397:2467–75.
Bristol-Myers Squibb. An exploratory, open-label, proof-of-concept, phase 2a study of Mavacamten (MYK-461) in participants with heart failure with preserved ejection fraction (HFpEF) and chronic elevation of cardiac biomarkers. https://classic.clinicaltrials.gov/ct2/show/NCT04766892.
Helms AS, Davis FM, Coleman D, Bartolone SN, Glazier AA, Pagani F, Yob JM, Sadayappan S, Pedersen E, Lyons R, Westfall MV, Jones R, Russell MW, Day SM. Sarcomere Mutation-Specific Expression Patterns in Human Hypertrophic Cardiomyopathy. Circulation: Cardiovascular Genetics. 2014;7:434–43.
Glazier AA, Thompson A, Day SM. Allelic Imbalance and Haploinsufficiency in MYBPC3-linked Hypertrophic Cardiomyopathy. Pflugers Arch. 2019;471:781–93.
Butters A, Thomson K, Harrington F, Henden N, McGuire K, Byrne AB et al. A rare splice-site variant in cardiac troponin-T (TNNT2): the need for ancestral diversity in genomic reference datasets. medRxiv. 2024. https://doi.org/10.1101/2024.02.08.24302375.
Meder B, Rühle F, Weis T, Homuth G, Keller A, Franke J. A genome-wide association study identifies 6p21 as novel risk locus for dilated cardiomyopathy. Eur Heart J. 2014;35:1069–77.
Aragam K, Chaffin M, Levinson R, McDermott G, Choi S, Shoemaker M. Phenotypic refinement of heart failure in a national biobank facilitates genetic discovery. Circulation. 2019;139:489–501.
Acknowledgements
K.A.M. is supported by the British Heart Foundation [FS/IPBSRF/22/27059, RE/18/4/34215] and the NIHR Imperial College Biomedical Research Centre. The views expressed in this work are those of the authors and not necessarily those of the funders. For open access, the authors have applied a CC BY public copyright license to any Author Accepted Manuscript version arising from this submission. The graphical abstract was created with BioRender.com.
Author information
Authors and Affiliations
Contributions
Conceptualization: K.M.; Writing – original draft: P.D., N.K., S.M., G.S.; Writing – review & editing: K.M., P.D., N.K., S.M.; Visualization: P.D., N.K., S.M.; Supervision: K.M.
Corresponding author
Ethics declarations
Conflicts of Interest / Compliance with Ethical Standards
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Editor-in-Chief Enrique Lara-Pezzi oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mukhopadhyay, S., Dixit, P., Khanom, N. et al. The Genetic Factors Influencing Cardiomyopathies and Heart Failure across the Allele Frequency Spectrum. J. of Cardiovasc. Trans. Res. (2024). https://doi.org/10.1007/s12265-024-10520-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12265-024-10520-y