Abstract
Background
An early diagnosis of ICU-acquired weakness (ICU-AW) is difficult because disorders of consciousness frequently preclude muscle strength assessment. In this study, we investigated feasibility and accuracy of electrophysiological recordings to diagnose ICU-AW early in non-awake critically ill patients.
Methods
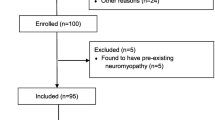
Newly admitted patients, mechanically ventilated ≥2 days and unreactive to verbal stimuli, were included in this study. Electrophysiological recordings comprised nerve conduction studies (NCS) of three nerves and, if coagulation was normal, myography in three muscles. Upon awakening, strength was assessed (ICU-AW: average Medical Research Council score <4), blinded for electrophysiological recordings. Feasibility was expressed as the percentage of recordings that were both possible and had sufficient technical quality. Diagnostic accuracy of feasible (i.e., feasibility >75 %) recordings was analyzed based on cut-off values from healthy controls and from critically ill patients with and without ICU-AW.
Results
Thirty-five patients were included (17 with ICU-AW). Recordings were obtained on day 4 (IQR: 3–6). Feasibility was acceptable for ulnar and peroneal nerve recordings, and low for sural recordings and myography. Diagnostic accuracy based on cut-off values from healthy controls was low. When using cut-off values from critically ill patients with and without ICU-AW, the peroneal compound muscle action potential amplitude and ulnar sensory nerve action potential amplitude had good diagnostic accuracy.
Conclusion
Nerve conduction studies of the ulnar and peroneal nerve are feasible in critically ill patients. The diagnostic accuracy is low using cut-off values from healthy controls. Cut-off values validated specifically for discrimination between critically ill patients with and without ICU-AW may improve diagnostic accuracy.



Similar content being viewed by others
References
Stevens RD, Dowdy DW, Michaels RK, Mendez-Tellez PA, Pronovost PJ, Needham DM. Neuromuscular dysfunction acquired in critical illness: a systematic review. Intensive Care Med. 2007;33:1876–91.
Latronico N, Bolton CF. Critical illness polyneuropathy and myopathy: a major cause of muscle weakness and paralysis. Lancet Neurol. 2011;10:931–41.
Stevens RD, Marshall SA, Cornblath DR, Hoke A, Needham DM, De Jonghe B, Ali NA, Sharshar T. A framework for diagnosing and classifying intensive care unit-acquired weakness. Crit Care Med. 2009;37(10 Suppl):S299–308.
Kress JP, Hall JB. ICU-acquired weakness and recovery from critical illness. N Engl J Med. 2014;370:1626–35.
Vanpee G, Hermans G, Segers J, Gosselink R. Assessment of limb muscle strength in critically ill patients: a systematic review. Crit Care Med. 2014;42:701–11.
Hough CL, Lieu BK, Caldwell ES. Manual muscle strength testing of critically ill patients: feasibility and interobserver agreement. Crit Care. 2011;15:R43.
Novak KR, Nardelli P, Cope TC, Filatov G, Glass JD, Khan J, Rich MM. Inactivation of sodium channels underlies reversible neuropathy during critical illness in rats. J Clin Invest. 2009;119:1150–8.
Latronico N, Shehu I, Guarneri B. Use of electrophysiologic testing. Crit Care Med. 2009;37:S316–20.
Khan J, Harrison TB, Rich MM, Moss M. Early development of critical illness myopathy and neuropathy in patients with severe sepsis. Neurology. 2006;67:1421–5.
Latronico N, Bertolini G, Guarneri B, Botteri M, Peli E, Andreoletti S, Bera P, Luciani D, Nardella A, Vittorielli E, Simini B, Candiani A. Simplified electrophysiological evaluation of peripheral nerves in critically ill patients: the Italian multi-centre CRIMYNE study. Crit Care. 2007;11:R11.
Weber-Carstens S, Koch S, Spuler S, Spies CD, Bubser F, Wernecke KD, Deja M. Nonexcitable muscle membrane predicts intensive care unit-acquired paresis in mechanically ventilated, sedated patients. Crit Care Med. 2009;37:2632–7.
Moss M, Yang M, Macht M, Sottile P, Gray L, McNulty M, Quan D. Screening for critical illness polyneuromyopathy with single nerve conduction studies. Intensive Care Med. 2014;40:683–90.
Rich MM, Bird SJ, Raps EC, McCluskey LF, Teener JW. Direct muscle stimulation in acute quadriplegic myopathy. Muscle Nerve. 1997;20:665–73.
Allen DC, Arunachalam R, Mills KR. Critical illness myopathy. Further evidence from muscle-fiber excitability studies of an acquired channelopathy. Muscle Nerve. 2008;37:14–22.
Appleton R, Kinsella J. Nonexcitable muscle membrane predicts intensive care unit-acquired paresis in mechanically ventilated. sedated patients. Crit Care Med. 2010;38:1233–4 author reply 1234.
Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig LM, Moher D, Rennie D, de Vet HCW, Lijmer JG, The Standards for Reporting of Diagnostic Accuracy Group. The STARD statement for reporting studies of diagnostic accuracy: explanation and elaboration. Ann Intern Med. 2003;44:639–50.
Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O’Neal PV, Keane KA, Tesoro EP, Elswick RK. The Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002;166:1338–44.
Van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19:604–7.
Kimura J. Nerve conduction studies and electromyography. In: Dyck P, Thomas P, Griffin J, Low P, Poduslo J, editors. Peripher neuropathy. Philadelphia: Saunders; 1993. p. 598–635.
American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 1992;20:864–74.
Annane D, Bellissant E, Cavaillon J-M. Septic shock. Lancet. 2005;365:63–78.
Verhamme C, Schaik IN, Koelman JHTM, Haan RJ, Vermeulen M, Visser M. Clinical disease severity and axonal dysfunction in hereditary motor and sensory neuropathy Ia. J Neurol. 2004;251:1491–7.
Koch S, Spuler S, Deja M, Bierbrauer J, Dimroth A, Behse F, Spies CD, Wernecke KD, Weber-Carstens S. Critical illness myopathy is frequent: accompanying neuropathy protracts ICU discharge. J Neurol Neurosurg Psychiatry. 2011;82:287–93.
Latronico N, Nattino G, Guarneri B, Fagoni N, Amantini A, Bertolini G. Validation of the peroneal nerve test to diagnose critical illness polyneuropathy and myopathy in the intensive care unit: the multicentre Italian CRIMYNE-2 diagnostic accuracy study. F1000Research 2014;1–11.
Park EJ, Nishida T, Sufit RL, Minieka MM. Prolonged compound muscle action potential duration in critical illness myopathy: report of nine cases. J Clin Neuromuscul Dis. 2004;5:176–83.
Goodman BP, Harper CM, Boon AJ. Prolonged compound muscle action potential duration in critical illness myopathy. Muscle Nerve. 2009;40:1040–2.
Patel SB, Kress JP. Sedation and analgesia in the mechanically ventilated patient. Am J Respir Crit Care Med. 2012;185:486–97.
Guarneri B, Bertolini G, Latronico N. Long-term outcome in patients with critical illness myopathy or neuropathy: the Italian multicentre CRIMYNE study. J Neurol Neurosurg Psychiatry. 2008;79:838–41.
Koch S, Wollersheim T, Bierbrauer J, Haas K, Mörgeli R, Deja M, Spies CD, Spuler S, Krebs M, Weber-Carstens S. Long term recovery in critical illness myopathy is complete, contrary to polyneuropathy. Muscle Nerve. 2014;50:431–6.
Acknowledgments
This research was performed within the framework of CTMM, the Center for Translational Molecular Medicine (www.ctmm.nl), project MARS (Grant 04I-201).
Conflict of interest
This study was not sponsored. Dr. L. Wieske is currently receiving a personal grant (ZonMw–AGIKO grant [project number 40-00703-98-11636]) from the Netherlands Organization for Health Research and Development, Prof. I.N. van Schaik received departmental honoraria for serving on scientific advisory boards and a steering committee for CSL-Behring. For the remaining authors none were declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wieske, L., Verhamme, C., Witteveen, E. et al. Feasibility and Diagnostic Accuracy of Early Electrophysiological Recordings for ICU-Acquired Weakness: An Observational Cohort Study. Neurocrit Care 22, 385–394 (2015). https://doi.org/10.1007/s12028-014-0066-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-014-0066-9