Abstract
Background and objective
Obstructive sleep apnea (OSA) and coronary artery disease (CAD) are known to be associated with activation of inflammatory pathways. Treatment of OSA is hypothesized to lead to a reduction in inflammation. This study investigated the association between OSA and inflammation in CAD patients, and determined the effect of one night of continuous positive airway pressure (CPAP) therapy.
Materials and methods
Patients with stable CAD and moderate–severe OSA underwent overnight polysomnography (PSG) one night, and again during CPAP the following night. Cardiac stress and inflammation markers were determined in the morning after each PSG.
Results
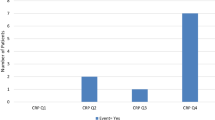
Included were 23 patients with OSA (74% male; age 63 ± 10 years; ejection fraction 50 ± 8%). During CPAP, the most remarkable decreases from baseline were observed in the apnea–hypopnea index (AHI; from 35 ± 21 to 11 ± 11/h; p < 0.001), high-sensitivity C‑reactive protein (hs-CRP; 0.396 ± 0.428 to 0.308 ± 0.299 mg/dL; p = 0.006), and creatine kinase-MB (CKMB; 1.818 ± 1.014 to 1.551 ± 0.819 U/L; p = 0.018). After adjusting for age, gender, obesity, and heart failure severity as relevant confounders, there was a significant correlation between baseline AHI and myoglobin (r = 0.650; p = 0.002). Likewise, there were correlations between mean desaturation and CKMB (r = 0.606, p = 0.007), and between time spent with O2 saturation <90% (T < 90%) and interleukin 6 (r = 0.525, p = 0.013).
Conclusion
Among CAD patients there are clear correlations between surrogate measures of OSA severity, such as T < 90%, mean desaturation, and AHI, and inflammation, even after adjustment for obesity and the severity of heart failure as crucial confounding factors. Effective treatment of OSA with CPAP decreased cardiac stress and inflammation.
Zusammenfassung
Hintergrund und Ziel der Arbeit
Sowohl die obstruktive Schlafapnoe (OSA) als auch die koronare Herzkrankheit (KHK) sind bekanntermaßen mit einer Aktivierung inflammatorischer Wege assoziiert. Eine Therapie der OSA führt mutmaßlich zu einer Verminderung der Entzündung. In dieser Studie wurde die Assoziation von OSA und KHK in Bezug auf die Entzündung und die Effekte einer einmaligen nächtlichen Überdrucktherapie (CPAP) untersucht.
Material und Methoden
Patienten mit stabiler KHK und moderater bis schwerer OSA unterzogen sich einer Nacht mit diagnostischer Polysomnographie (PSG) und einer PSG während der Therapie mit Überdruckbeatmung („continuous positive airway pressure“, CPAP) in der Folgenacht. Marker für kardiale Belastung und Entzündung wurden jeweils am Morgen nach der PSG bestimmt.
Ergebnisse
23 Patienten (74 % männlich; 63 ± 10 Jahre alt; Ejektionsfraktion: 50 ± 8 %) zeigten eine obstruktive Schlafapnoe. Unter CPAP wies der Apnoe-Hypopnoe-Index (AHI) einen signifikanten Abfall auf (AHI; von 35 ± 21 auf 11 ± 11/h; p < 0,001). Außerdem zeigte sich ein signifikanter Abfall im hochsensitiven CRP (hs-CRP; von 0,396 ± 0,428 auf 0,308 ± 0,299 mg/dl; p = 0,006) und in der Kreatininkinase-MB (CKMB; von 1,818 ± 1,014 auf 1,551 ± 0,819 U/l; p = 0,018). Es ergab sich – in einem multivariaten Modell nach Adjustierung für Alter, Geschlecht, Adipositas und Schwere der Herzinsuffizienz als wichtige Störfaktoren – eine signifikante Korrelation zwischen dem Ausgangs-AHI und Myoglobin (r = 0,650; p = 0,002). Darüber hinaus zeigten sich Korrelationen zwischen der mittleren Sauerstoffentsättigung und dem CKMB-Wert (r = 0,606; p = 0,007) sowie zwischen der Zeit mit einer Sauerstoffsättigung unter 90 % (T < 90 %) und Interleukin-6 (r = 0,525; p = 0,013).
Schlussfolgerungen
Bei Patienten mit KHK ergaben sich robuste Korrelationen zwischen Surrogatmarkern der Schwere der OSA, wie z. B. T < 90 %, mittlere Sauerstoffentsättigung und AHI, sowie Inflammationsmarkern, selbst nach Adjustierung für Adipositas und Schwere der Herzinsuffizienz als entscheidende Störfaktoren. Eine effektive Therapie der OSA mit CPAP vermindert kardialen Stress und Entzündung.



Similar content being viewed by others
References
Lloyd-Jones DM, Larson MG, Beiser A, Levy D (1999) Lifetime risk of develo** coronary heart disease. Lancet 353:89–92
Prinz C, Bitter T, Piper C, Horstkotte D, Faber L, Oldenburg O (2010) Patienten mit koronarer Herzerkrankung leiden häufig unter Schlafapnoe. Wien Med Wochenschr 160:349–355
Mentz RJ, Kelly JP, von Lueder TG, Voors AA, Lam CS, Cowie MR, Kjeldsen K, Jankowska EA, Atar D, Butler J, Fiuzat M, Zannad F, Pitt B, O’Connor CM (2014) Noncardiac comorbidities in heart failure with reduced versus preserved ejection fraction. J Am Coll Cardiol 64:2281–2293
Bradley TD, Floras JS (2009) Obstructive sleep apnoea and its cardiovascular consequences. Lancet 373:82–93
**e X, Pan L, Ren D, Du C, Guo Y (2013) Effects of continuous positive airway pressure therapy on systemic inflammation in obstructive sleep apnea: a meta-analysis. Sleep Med 14:1139–1150
Libby P (2002) Inflammation in atherosclerosis. Nature 420:868–874
Swirski FK, Nahrendorf M (2013) Leukocyte behavior in atherosclerosis, myocardial infarction, and heart failure. Science 339(6116):161–166
Oldenburg O, Wellmann B, Buchholz A, Bitter T, Fox H, Thiem U, Horstkotte D, Wegscheider K (2015) Nocturnal hypoxemia is associated with increased mortality in stable heart failure patients. Eur Heart J 37:1695–1703
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, Marcus CL, Mehra R, Parthasarathy S, Quan SF, Redline S, Strohl KP, Davidson Ward SL, Tangredi MM, American Academy of Sleep Medicine (2012) American Academy of Sleep Medicine. Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. J Clin Sleep Med 8:597–619
Spicuzza L, Caruso D, Di Maria G (2015) Obstructive sleep apnoea syndrome and its management. Ther Adv Chronic Dis 6:273–285
Palazzuoli A, Gallotta M, Quatrini I, Nuti R (2010) Natriuretic peptides (BNP and NT-proBNP): measurement and relevance in heart failure. Vasc Health Risk Manag 6:411–418
Larkin EK, Rosen CL, Kirchner H, Storfer-Isser A, Emancipator JL, Johnson NL, Zambito AM, Tracy RP, Jenny NS, Redline S (2005) Variation of C‑reactive protein levels in adolescents: association with sleep-disordered breathing and sleep duration. Circulation 111:1978–1984
Shamsuzzaman ASM, Winnicki M, Lanfranchi P, Wolk R, Kara T, Accurso V, Somers VK (2002) Elevated C‑reactive protein in patients with obstructive sleep apnea. Circulation 105:2462–2464
Ip MSM, Tse H‑F, Lam B, Tsang KWT, Lam W‑K (2004) Endothelial function in obstructive sleep apnea and response to treatment. Am J Respir Crit Care Med 169:348–353
Randby A, Namtvedt SK, Einvik G, Hrubos-Strmø H, Hagve TA, Somers VK, Omland T (2012) Obstructive sleep apnea is associated with increased high-sensitivity cardiac troponin T levels. Chest 142:639–646
Turker Y, Baltaci D, Turker Y, Ozturk S, Sonmez CI, Deler MH, Sariguzel YC, Sariguzel F, Ankarali H (2015) Investigation of relationship of visceral body fat and inflammatory markers with metabolic syndrome and its components among apparently healthy individuals. Int J Clin Exp Med 8:13067–13077
Gottlieb JD, Schwartz AR, Marshall J, Ouyang P, Kern L, Shetty V, Trois M, Punjabi NM, Brown C, Najjar SS, Gottlieb SS (2009) Hypoxia, not the frequency of sleep apnea, induces acute hemodynamic stress in patients with chronic heart failure. J Am Coll Cardiol 54:1706–1712
Ciccone MM, Favale S, Scicchitano P, Mangini F, Mitacchione G, Gadaleta F, Longo D, Iacoviello M, Forleo C, Quistelli G, Taddei S, Resta O, Carratù P (2012) Reversibility of the endothelial dysfunction after CPAP therapy in OSAS patients. Int J Cardiol 158:383–386
Colish J, Walker JR, Elmayergi N, Almutairi S, Alharbi F, Lytwyn M, Francis A, Bohonis S, Zeglinski M, Kirkpatrick ID, Sharma S, Jassal DS (2012) Obstructive sleep apnea: effects of continuous positive airway pressure on cardiac remodeling as assessed by cardiac biomarkers, echocardiography, and cardiac MRI. Chest 141:674–681
Barceló A, Esquinas C, Bauçà JM, Piérola J, De La Peña M, Arqué M, Sánchez-de-la-Torre M, Alonso-Fernández A, Barbé F (2014) Effect of CPAP treatment on plasma high sensitivity troponin levels in patients with obstructive sleep apnea. Respir Med 108:1060–1063
Spießhöfer J, Fox H, Lehmann R, Efken C, Heinrich J, Bitter T, Körber B, Horstkotte D, Oldenburg O (2015) Heterogenous haemodynamic effects of adaptive servoventilation therapy in slee** patients with heart failure and Cheyne-Stokes respiration compared to healthy volunteers. Heart Vessels 31:1117–1130
Spießhöfer J, Heinrich J, Lehmann R, Efken C, Fox H, Bitter T, Körber B, Horstkotte D, Oldenburg O (2015) Respiratory effects of adaptive servoventilation therapy in patients with heart failure and Cheyne-Stokes respiration compared to healthy volunteers. Respiration 89:374–382
Oldenburg O, Spießhöfer J, Fox H, Bitter T, Horstkotte D (2015) Cheyne-Stokes respiration in heart failure: friend or foe? Hemodynamic effects of hyperventilation in heart failure patients and healthy volunteers. Clin Res Cardiol 104:328–333
Mehra R, Gottlieb DJ (2015) A paradigm shift in the treatment of central sleep apnea in heart failure. Chest 148:848–851
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
T. Bitter, H. Fox, and O. Oldenburg received honoraria for speaking at symposia and financial support for attending symposia by ResMed Germany Inc., Novartis, and Bayer; H. Fox received financial support for educational programs by Novartis. F. Schindhelm received financial support for attending a symposium by Itamar. J. Spießhöfer, H. Schmalgemeier, S. Pearse, A. Türoff, and D. Horstkotte declare that they have no competing interests.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
J. Spießhöfer and H. Schmalgemeier share first authorship
Rights and permissions
About this article
Cite this article
Spießhöfer, J., Schmalgemeier, H., Schindhelm, F. et al. Inflammation in patients with obstructive sleep apnea and coronary artery disease. Somnologie 21, 257–264 (2017). https://doi.org/10.1007/s11818-017-0111-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11818-017-0111-y