Abstract
Background
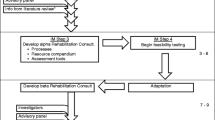
Cancer rehabilitation navigation (CRNav) is a care delivery model that expedites identification and management of symptom-related functional morbidity for individuals undergoing cancer treatment. A CRNav program is unique in that it embeds a cancer rehabilitation professional in the cancer center for patient screening and assessment. The implementation of CRNav programs has not been studied and doing so could facilitate greater uptake of these programs.
Methods
Using implementation science frameworks, we conducted a qualitative, post-implementation analysis of a CRNav program that was implemented in 2019. Semi-structured, 1:1 interviews were guided by the Consolidated Framework for Implementation Research (CFIR) and a combination of deductive and inductive analyses, using a priori established codes, was used to assess the implementation context, and identify emergent themes of barriers and facilitators to implementation. Participant described implementation strategies were characterized and defined using the Expert Consensus Recommendations for Implementing Change (ERIC) taxonomy.
Results
Eleven stakeholders including physicians, administrators, clinical staff, and patients, involved with program development and the implementation effort, participated in interviews. Predominant barriers to implementation included develo** the program infrastructure, and lack of awareness of rehabilitation services among oncology professionals, predominant facilitators of implementation included; physical co-location of the navigator in the cancer center, individual characteristics of the navigator, and unique characteristics of the program. Strategies described that supported implementation included develo** stakeholder interrelationships, evaluating and iteratively adapting the program, creating infrastructure, training and education, and supporting clinicians.
Conclusion
This analysis uses implementation science to methodically analyze and characterize factors that may contribute to successful implementation of a CRNav program. These findings could be used alongside a prospective context-specific analysis to tailor future implementation efforts.
Implications for Cancer Survivors
Implementing a CRNav program expedites a patient’s direct contact with a rehabilitation provider complementing the cancer care delivery team, and providing an additive and often missing service.

Similar content being viewed by others
Data availability
N/A.
Notes
USC IRB Approval Number: 00115153.
References
Stout NL, Silver JK, Raj VS, et al. Toward a National Initiative in Cancer Rehabilitation: Recommendations From a Subject Matter Expert Group. Arch Phys Med Rehabil. 2016;97(11):2006–15. https://doi.org/10.1016/j.apmr.2016.05.002.
Alfano CM, Zucker DS, Pergolotti M, et al. A Precision Medicine Approach to Improve Cancer Rehabilitation’s Impact and Integration with Cancer Care and Optimize Patient Wellness. Curr Phys Med Rehabil Rep. 2017;5(1):64–73.
Stout NL, Binkley JM, Schmitz KH, et al. A prospective surveillance model for rehabilitation for women with breast cancer. Cancer. 2012;118(8 Suppl):2191–200. https://doi.org/10.1002/cncr.27476.
Bartolo M, Zucchella C, Pace A, et al. Early rehabilitation after surgery improves functional outcome in inpatients with brain tumours. J Neurooncol. 2012;107(3):537–44. https://doi.org/10.1007/s11060-011-0772-5.
Arving C, Assmus J, Thormodsen I, Berntsen S, Nordin K. Early rehabilitation of cancer patients-An individual randomized stepped-care stress-management intervention. Psychooncology. 2019;28(2):301–8. https://doi.org/10.1002/pon.4940.
Stout NL, Santa Mina D, Lyons KD, Robb K, Silver JK. A systematic review of rehabilitation and exercise recommendations in oncology guidelines. CA Cancer J Clin. 2021;71(2):149–75. https://doi.org/10.3322/caac.21639.
Barnes CA, Stout NL, Varghese TK Jr, et al. Clinically Integrated Physical Therapist Practice in Cancer Care: A New Comprehensive Approach. Phys Ther. 2020;100(3):543–53. https://doi.org/10.1093/ptj/pzz169.
Stout NL, Sleight A, Pfeiffer D, Galantino ML, deSouza B. Promoting assessment and management of function through navigation: opportunities to bridge oncology and rehabilitation systems of care. Support Care Cancer. 2019;27(12):4497–505. https://doi.org/10.1007/s00520-019-04741-0.
Nadler MB, Rose AAN, Prince R, et al. Increasing Referrals of Patients With Gastrointestinal Cancer to a Cancer Rehabilitation Program: A Quality Improvement Initiative. JCO Oncol Pract. 2021;17(4):e593–602. https://doi.org/10.1200/OP.20.00432.
IJsbrandy C, Ottevanger PB, Gerritsen WR, van Harten WH, Hermens RP. Determinants of adherence to physical cancer rehabilitation guidelines among cancer patients and cancer centers: a cross-sectional observational study. J Cancer Surviv. 2021;15(1):163–77.
Rosario-Concepción RA, Calderín YB, Aponte CL, López-Acevedo CE, Sepúlveda-Irrizarry FL. Oncologists’ Attitude and Knowledge about Cancer Rehabilitation. PM&R. 2021;13(12):1357–61.
National Academies of Sciences, Engineering, and Medicine. Establishing effective patient navigation programs in oncology: proceedings of a workshop. Washington, DC: The National Academies Press; 2018. https://doi.org/10.17226/25073.
Neo J, Fettes L, Gao W, Higginson IJ, Maddocks M. Disability in activities of daily living among adults with cancer: A systematic review and meta-analysis. Cancer Treat Rev. 2017;61:94–106. https://doi.org/10.1016/j.ctrv.2017.10.006.
Mitchell SA, Chambers DA. Leveraging Implementation Science to Improve Cancer Care Delivery and Patient Outcomes. J Oncol Pract. 2017;13(8):523–9. https://doi.org/10.1200/JOP.2017.024729.
Nilsen P, Bernhardsson S. Context matters in implementation science: a sco** review of determinant frameworks that describe contextual determinants for implementation outcomes. BMC Health Serv Res. 2019;19(1):189. https://doi.org/10.1186/s12913-019-4015-3.
Brown CH, Curran G, Palinkas LA, et al. An Overview of Research and Evaluation Designs for Dissemination and Implementation. Annu Rev Public Health. 2017;38:1–22. https://doi.org/10.1146/annurev-publhealth-031816-044215.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. https://doi.org/10.1186/1748-5908-4-50.
Powell BJ, Waltz TJ, Chinman MJ, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10(1):21. https://doi.org/10.1186/s13012-015-0209-1.
Kirk MA, Kelley C, Yankey N, Birken SA, Abadie B, Damschroder L. A systematic review of the use of the Consolidated Framework for Implementation Research. Implement Sci. 2016;11:72. https://doi.org/10.1186/s13012-016-0437-z.
Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–907. https://doi.org/10.1007/s11135-017-0574-8.
Selvi AF. Qualitative content analysis. In: McKinley J, Rose H, editors. The Routledge handbook of research methods in applied linguistics. 1st ed. London: Routledge; 2019. p. 440–52.
Chun Tie Y, Birks M, Francis K. Grounded theory research: A design framework for novice researchers. SAGE Open Med. 2019;7:2050312118822927. https://doi.org/10.1177/2050312118822927.
Miech EJ, Rattray NA, Flanagan ME, Damschroder L, Schmid AA, Damush TM. Inside help: An integrative review of champions in healthcare-related implementation. SAGE Open Med. 2018;6:2050312118773261. https://doi.org/10.1177/2050312118773261.
Li SA, Jeffs L, Barwick M, Stevens B. Organizational contextual features that influence the implementation of evidence-based practices across healthcare settings: a systematic integrative review. Syst Rev. 2018;7(1):72. https://doi.org/10.1186/s13643-018-0734-5.
Harrington SE, Litterini AJ. The Critical Need for Oncology Rehabilitation Education in the Entry-Level Doctor of Physical Therapy Curriculum. Rehabil Oncol. 2022;40(1):3–4.
Waltz TJ, Powell BJ, Fernandez ME, Abadie B, Damschroder LJ. Choosing implementation strategies to address contextual barriers: diversity in recommendations and future directions. Implement Sci. 2019;14(1):42. https://doi.org/10.1186/s13012-019-0892-4.
Meyers DC, Durlak JA, Wandersman A. The quality implementation framework: a synthesis of critical steps in the implementation process. Am J Community Psychol. 2012;50(3–4):462–80. https://doi.org/10.1007/s10464-012-9522-x.
Paskett ED, Krok-Schoen JL, Gray DM 2nd. Patient Navigation-An Effective Strategy to Reduce Health Care Costs and Improve Health Outcomes. JAMA Oncol. 2017;3(6):825–6. https://doi.org/10.1001/jamaoncol.2016.6107.
National Academies of Sciences, Engineering, and Medicine. Long-term survivorship care after cancer treatment: proceedings of a workshop. Washington, DC: The National Academies Press; 2018. https://doi.org/10.17226/25043.
Pergolotti M, Deal AM, Lavery J, Reeve BB, Muss HB. The prevalence of potentially modifiable functional deficits and the subsequent use of occupational and physical therapy by older adults with cancer. J Geriatr Oncol. 2015;6(3):194–201.
Cheville AL, Beck LA, Petersen TL, Marks RS, Gamble GL. The detection and treatment of cancer-related functional problems in an outpatient setting. Support Care Cancer. 2009;17(1):61–7. https://doi.org/10.1007/s00520-008-0461-x.
L’Hotta AJ, Varughese TE, Lyons KD, Simon L, King AA. Assessments used to measure participation in life activities in individuals with cancer: a sco** review. Support Care Cancer. 2020;28(8):3581–92. https://doi.org/10.1007/s00520-020-05441-w.
Kline RM, Arora NK, Bradley CJ, et al. Long-Term Survivorship Care After Cancer Treatment - Summary of a 2017 National Cancer Policy Forum Workshop. J Natl Cancer Inst. 2018;110(12):1300–10. https://doi.org/10.1093/jnci/djy176.
Alfano CM, Leach CR, Smith TG, et al. Equitably improving outcomes for cancer survivors and supporting caregivers: A blueprint for care delivery, research, education, and policy. CA: Cancer J Clin. 2019;69(1):35–49. https://doi.org/10.3322/caac.21548.
Basch E. Missing Patients’ Symptoms in Cancer Care Delivery—The Importance of Patient-Reported Outcomes. JAMA Oncol. 2016;2(4):433–4. https://doi.org/10.1001/jamaoncol.2015.4719.
Spill GR, Hlubocky FJ, Daugherty CK. Oncologists’ and Physiatrists’ Attitudes Regarding Rehabilitation for Patients With Advanced Cancer. PM&R. 2012;4(2):96–108. https://doi.org/10.1016/j.pmrj.2011.08.539.
Laugsand EA, Sprangers MA, Bjordal K, Skorpen F, Kaasa S, Klepstad P. Health care providers underestimate symptom intensities of cancer patients: a multicenter European study. Health Qual Life Outcome. 2010;8:104. https://doi.org/10.1186/1477-7525-8-104.
Maiwald P, Weis J, Kurlemann U, et al. Barriers to utilisation of cancer rehabilitation from the expert’s view: A cross-sectional survey. Eur J Cancer Care (Engl). 2022;31(1):e13522. https://doi.org/10.1111/ecc.13522.
Funding
This work was funded by the APTA Academy of Oncologic Physical Therapy Research Grant 2021.
Author information
Authors and Affiliations
Contributions
Concept development—NS, SH, AP, MA.
Data collection—NS, VP, BS, AP.
Data analysis—NS, VP, BS, AP.
Manuscript writing—NS, SH, VP.
Figure preparation- NS.
Manuscript review and approval- all authors.
Corresponding author
Ethics declarations
Ethics approval
University of South Carolina IRB approval: 00115153, West Virginia University IRB: 2202514439.
Consent for publication
All authors have reviewed the final manuscript and consent to publication.
Competing interests
Stout- Survivorship solutions LLC, Medbridge Inc.
Harrington, Perry, Alappattu, Pfab, Stewart, Manes—none.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stout, N.L., Harrington, S.E., Perry, A. et al. Implementation of a Cancer Rehabilitation Navigation Program: a qualitative analysis of implementation determinants and strategies. J Cancer Surviv (2023). https://doi.org/10.1007/s11764-023-01374-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11764-023-01374-5