Abstract
Background
Alcohol use disorder (AUD) is a highly prevalent public health problem that contributes to opioid- and benzodiazepine-related morbidity and mortality. Even though co-utilization of these substances is particularly harmful, data are sparse on opioid or benzodiazepine prescribing patterns among individuals with AUD.
Objective
To estimate temporal trends and disparities in opioid, benzodiazepine, and opioid/benzodiazepine co-prescribing among individuals with AUD in New York State (NYS).
Design/Participants
Serial cross-sectional study analyzing merged data from the NYS Office of Addiction Services and Supports (OASAS) and the NYS Department of Health Medicaid Data Warehouse. Subjects with a first admission to an OASAS treatment program from 2005–2018 and a primary AUD were included. A total of 148,328 subjects were identified.
Measures
Annual prescribing rates of opioids, benzodiazepines, or both between the pre- (2005–2012) and post- (2013–2018) Internet System for Tracking Over-Prescribing (I-STOP) periods. I-STOP is a prescription monitoring program implemented in NYS in August 2013. Analyses were stratified based on sociodemographic factors (age, sex, race/ethnicity, and location).
Results
Opioid prescribing rates decreased between the pre- and post-I-STOP periods from 25.1% (95% CI, 24.9–25.3%) to 21.3% (95% CI, 21.2–21.4; P <.001), while benzodiazepine (pre: 9.96% [95% CI, 9.83–10.1%], post: 9.92% [95% CI, 9.83–10.0%]; P =.631) and opioid/benzodiazepine prescribing rates remained unchanged (pre: 3.01% vs. post: 3.05%; P =.403). After I-STOP implementation, there was a significant decreasing trend in opioid (change, −1.85% per year, P <.0001), benzodiazepine (−0.208% per year, P =.0184), and opioid/benzodiazepine prescribing (−0.267% per year, P <.0001). Opioid, benzodiazepine, and co-prescription rates were higher in females, White non-Hispanics, and rural regions.
Conclusions
Among those with AUD, opioid prescribing decreased following NYS I-STOP program implementation. While both benzodiazepine and opioid/benzodiazepine co-prescribing rates remained high, a decreasing trend was evident after program implementation. Continuing high rates of opioid and benzodiazepine prescribing necessitate the development of innovative approaches to improve the quality of care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Alcohol use disorder (AUD) is a major public health problem that impacts up to 17 million Americans and costs society $249 billion each year.1, 2 Alcohol-related visits to the emergency department (ED) have increased substantially, and alcohol use is the fourth leading cause of preventable death in the USA.3, 4 Alcohol use is likely to be correlated with a higher risk of misusing multiple substances including opioids and benzodiazepines,5, 6 and the negative consequences of these substances — including overdoses and death — are more pronounced when combined with alcohol.3, 7,8,9 While opioid and benzodiazepine prescribing is well researched, less is known about the co-utilization of alcohol with these prescription medications.
The co-use of alcohol, opioids, and benzodiazepines is associated with a greater risk of morbidity and mortality. Castle et al. examined the Drug Abuse Warning Network (DAWN) and found that the rate of alcohol-related ED visits doubled between 2005 and 2010.3 Nearly 60% of these visits also involved the use of centrally acting agents, almost half of which were opioids or benzodiazepines. Similarly, another DAWN study showed that alcohol was involved in 22% of opioid-related deaths reported within the database in 2010.9 A recent study of MarketScan medical claims showed that an AUD diagnosis predicted a significantly higher risk of opioid overdoses, accidents, and injuries.10 Benzodiazepine utilization has also been increasing significantly with a 67% increase in the number of prescriptions and a 3-fold increase in the quantity between the mid-1990s to 2013.11, 12 In addition, individuals prescribed both an opioid and a benzodiazepine increased 41% from 2002 to 2014.13 Even though co-utilization of these substances is problematic, data are sparse on opioid or benzodiazepine prescribing patterns among individuals with documented AUD. In addition, there is very little empirical evidence on concurrent benzodiazepine, opioid, and alcohol use. Additional information regarding prescribing patterns for these substances could assist policymakers in addressing the increased risk of morbidity and mortality associated with their co-utilization.
Over the past decade, opioid misuse has led to most US states adopting prescription monitoring programs (PMPs) to facilitate controlled substances and track prescribing practices.14 These programs aim to detect high-risk prescribing and drug-seeking behavior to reduce prescription drug supply and diversion. In August 2013, New York State (NYS) implemented the Internet System for Tracking Over-Prescribing (I-STOP) PMP, which required real-time submission of dispensed controlled substance data, authorized PMP access for pharmacists, and was compulsory for any practitioner writing prescriptions for a Schedule II, III, or IV controlled substance.15 The NYS I-STOP was unique as it was the first to mandate that clinicians consult the PMP database to review a patient’s prescription history prior to prescribing controlled substances. It was shown that the number of opioid prescriptions declined and opioid morbidity levelled off following I-STOP implementation.16, 17 However, these findings may not extend to other controlled substances and may be different in specific patient populations such as those with AUD. Furthermore, differences in controlled substance prescribing and ultimately patient outcomes may be specific to certain sociodemographic groups.
To implement a comprehensive and targeted intervention or treatment strategy, it is first necessary to understand treatment patterns and sub-groups at highest risk of overdose or overdose-related mortality. Therefore, we linked two NYS databases to (1) examine temporal trends in opioids, benzodiazepines, and co-prescribing accounting for the introduction of NYS I-STOP; (2) evaluate disparities in prescribing trends based on sociodemographic factors; and (3) explore associations between patient-level factors and co-prescribing in individuals with a primary AUD problem.
METHODS
Data Source and Patient Sample
This serial cross-sectional study linked data in two NYS databases: the NYS Office of Addiction Services and Supports (OASAS) Client Data System (CDS) and the NYS Department of Health Medicaid Data Warehouse (MDW). The CDS collects data on admissions and discharges for NYS residents in need of addiction services, with support provided through OASAS-certified treatment programs. The CDS data items are self-reported by clients during their care, and treatment providers submit these data through batch submission.
We initially identified subjects with a first admission to an OASAS treatment program from January 1, 2005, to December 31, 2018. Subjects were included if they were aged between 18 and 65 at time of index OASAS admission and were admitted for treatment with a primary alcohol use problem. Although OASAS treatment centers did not begin assessing for AUD until 2017, we assume that nearly all of them would have met criteria for an alcohol use disorder. In fact, 79% of the sample received an International Classification of Disease, Ninth Revision (ICD-9) or Tenth Revision (ICD-10) AUD diagnosis in subsequent Medicaid records. OASAS CDS treatment data were then merged with NYS MDW claims data using a unique client identifier to anonymously track subjects. Subjects were included if they had at least one MDW claim within the same year as the index OASAS admission. After entry, subjects were required to have at least one MDW claim within each sequential year to ensure that subjects were still eligible and active within NYS Medicaid for each specific year. We excluded subjects reporting either secondary or tertiary problems with opioids and those with less than one year of Medicaid service after the initial alcohol use admission. After the eligibility criteria were applied, 148,328 eligible subjects with a primary AUD remained in the sample for this study. The University at Buffalo institutional review board approved the study protocol.
Prescription Drugs and Covariates
The primary exposure was defined as a prescription claim for an opioid or benzodiazepine. Opioids were defined as medications containing fentanyl, levorphanol, morphine, pentazocine, oxycodone, dextropropoxyphene, hydrocodone, tramadol, tapenatadol, meperidine, hydromorphone, oxymorphone, codeine, dihydrocodeine, butorphanol, nalbuphine, and opium. We excluded prescriptions for opioid-containing cough medications. Benzodiazepines were identified as medications containing diazepam, lorazepam, alprazolam, clorazepic acid, clonazepam, estazolam, oxazepam, quazepam, temazepam, triazolam, clobazam, midazolam, chlordiazepoxide, and flurazepam. We also explored medications for opioid use disorder (MOUD) including buprenorphine, methadone, and naltrexone. The medications were identified based on National Drug Codes (NDCs) through the First Databank drug database. Opioid and benzodiazepine co-prescribing and dual opioid therapy were defined as an overlap in claims for at least 7 days. Chronic opioid usage was defined based on CDC criteria and included receipt of an opioid for >90 days.
Disparities in opioid and benzodiazepine prescribing based on age, sex assigned at birth, race/ethnicity, and location were evaluated, as differences have been reported for these sociodemographics.18,19,20,21 Age was stratified into three categories (18–35 years, 36–55 years, and >55 years) and race/ethnicity was stratified into four categories (White non-Hispanic, Black non-Hispanic, Other non-Hispanic, and Hispanic). Subject location was identified using three-digit zip codes, and subjects were assigned to one of the four major NYS Department of Health (DOH) geographic regions: Capital, Central, Metropolitan, and Western.22 Pre-existing comorbidities were identified using relevant ICD-9 and -10 codes based on the Charlson Comorbidity Index (CCI) and were stratified into four groups scoring 0, 1–2, 2–3, and >4.23 Pain diagnoses were defined based on ICD-9 and -10 codes and assigned to one of five categories: 1, arthritis/joint pain; 2, back/cervical pain; 3, neuropathies/neuralgias; 4, headaches/migraines; and 5, unclassified pain.24
Statistical Analysis
Using descriptive statistics, we conducted a repeated cross-sectional analysis of the annual prevalence rates of benzodiazepines, opioids, and their co-prescription. Annual prevalence rates were defined as the number of subjects having at least one prescription claim for an opioid, benzodiazepine, or both in each study year. A stratified analysis was conducted to evaluate differences in prescribing rates based on the pre-specified sociodemographic parameters (age, sex, race/ethnicity, and location).
In NYS, the prescription monitoring I-STOP program was signed into law in August 2012 and implemented in August 2013. This was identified as a natural inflection point, so we evaluated prescribing trends pre- (2005–2012) and post- (2013–2018) I-STOP implementation. Prescribing rates were evaluated in two ways: (1) by comparing prevalence rates and 95% confidence intervals (CIs) in the pre- and post-I-STOP periods using a two-rate chi-square test, and (2) using a segmented regression analysis of interrupted time series data to assess trend changes in regression line slope and level. This analysis allowed the estimation of changes in prescribing rates before and after program implementation while accounting for both sudden changes and changes in trends for the outcomes of interest.25 A change in level would indicate an immediate effect on prescribing rates, while a change in slope (or trend) of the regression line would point to a longer, more sustained response for the outcome. We accounted for autocorrelation in the error terms to estimate the coefficients for the level and trend changes caused by the introduction of the I-STOP program.
Next, we developed a multinomial logistic regression model to explore the relationship between patient-level factors and opioids, benzodiazepines, and co-prescriptions, with data pooled across the entire sample. The multinomial model included three levels: (1) prescribed neither an opioid nor a benzodiazepine (reference); (2) prescribed either an opioid or a benzodiazepine; and (3) co-prescribed an opioid and benzodiazepine. Each model included demographics (age, sex, race/ethnicity, location) and pre-existing conditions (comorbidity burden and pain diagnoses). Odds ratios (ORs) and 95% CIs were estimated, and each estimate was adjusted for all other variables in the model. All analyses were performed using IBM SPSS Statistics v.27 (IBM Corp., Armonk, NY) and SAS v.9.4 (SAS Institute, Cary, NC), and all hypothesis testing was two-sided with a significance set at p<0.05.
RESULTS
Changes in Opioid, Benzodiazepine, Co-Prescription, and MOUD Rates
Opioids
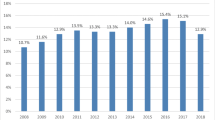
Opioid prescribing rates in adults with AUD were 25.1% (95% CI, 24.9–25.3) in the pre-I-STOP period and 21.3% (95% CI, 21.1–21.4) in the post-I-STOP period (P<.0001) (Table 1). The results of segmented regression analyses for opioid, benzodiazepine, and co-prescribing are summarized in Table 2 and Figure 1. For opioid prescribing, there was a significant increase in the slope (coefficient 1.578, P<.0001) prior to the introduction of the I-STOP program, followed by a significant decreasing trend after program implementation (coefficient −1.857, P<.0001). Hydrocodone was the most commonly prescribed opioid during the early period (2005–2012), with annual prescribing rates ranging from 9.80 to 14.25% (Fig. 2). The rate of oxycodone prescribing increased from 1.29% in 2005 to a peak of 10.92% in 2015. Both hydrocodone and oxycodone prescribing rates decreased in the post-I-STOP period but remained the most commonly prescribed opioids.
Trends in the prevalence of opioid, benzodiazepine, and co-prescribing in those with alcohol use disorder in New York State, 2005–2018. The shaded area represents when the New York State I-STOP program was signed into law (August 2012) and then implemented (August 2013). Abbreviation; I-STOP, Internet System for Tracking Over Prescribing.
Annual prescribing rates for select opioid medications among alcohol use disorder subjects in New York State, 2005–2018. Other includes the following opioids: levorphanol, pentazocine, propoxyphene, tapentadol, meperidine, dihydrocodeine, butorphanol, nalbuphine, and opium. The shaded area represents when the New York State I-STOP program was signed into law (August 2012) and then implemented (August 2013). Abbreviation; I-STOP, Internet System for Tracking Over Prescribing.
Benzodiazepines
The benzodiazepine prescribing rate in the pre-I-STOP period was 9.96% (95% CI, 9.83–10.1), and the rate remained elevated in the post-I-STOP period (9.92%, 95% CI 9.83–10.0; p=0.631) (Table 1). The slope for benzodiazepine prescribing significantly increased in the pre-I-STOP period (coefficient 1.0546, P<.0001) with a small but significant decrease after program implementation (coefficient −0.2075, P=.0184) (Table 2, Fig. 1).
Opioid and Benzodiazepine Co-prescribing
The opioid and benzodiazepine co-prescription rate in the pre-period was 3.01% (95% CI, 2.94–3.08), which remained unchanged in the post-I-STOP period (3.05%, 95% CI, 2.99–3.10; P=.403). There was a significant increase in the slope for co-prescribing prior to I-STOP implementation followed by a significant decrease in the post-I-STOP period (coefficient −0.2677, P<.0001).
Medications for Opioid Use Disorder
The overall prescribing rate for MOUD was 1.95% (95% CI, 1.90–2.01) in the pre-I-STOP period and increased to 4.98% (4.91–5.04) in the post-period (p<.0001) (Supplemental Table 1). Annual prescribing rates for buprenorphine and naltrexone increased significantly in the post-I-STOP period (p<.0001). Methadone prescribing rates remained relatively unchanged over the study period and were the least utilized MOUD (Supplemental Fig. 1).
Differences in Prescribing Rates Based on Age, Sex, Race/Ethnicity, and Location
Opioids
Opioid prescribing rates varied significantly based on age, with the highest rates seen among those aged 36–55 years compared to those aged 18–35 and >55 years (pre-I-STOP 27.4%, 24.2%, and 18.35%, respectively; P<.001 between groups) (Table 3 and Supplemental Fig. 2). There was a significant decrease in the slope for opioid prescribing within each age group (P<.0001), but prescribing rates remained significantly different between groups (P<.001) (Supplemental Table 2 and Supplemental Fig. 2). Opioid prescribing rates for females were consistently higher than males (pre-I-STOP: 32.22% vs. 21.68%) in both the pre- and post-I-STOP periods (P<.001). The increase in trend was similar for both females and males in the pre-I-STOP period, with a greater decrease seen for females in the post-I-STOP period (P<.0001). With respect to race and ethnicity, prescribing rates were higher in White non-Hispanic (29.88%) individuals in the pre-I-STOP period compared to Black non-Hispanic (21.75%), Other non-Hispanic (19.37%), and Hispanic groups (20.55%; P<.001 between groups) (Table 3). Notably, opioid prescribing decreased significantly in the post-I-STOP period for all race/ethnicity groups. Finally, in terms of the four NYS DoH geographic regions over time (calendar periods 2005–2008, 2009–2012, 2013–2015, and 2016–2018), the NYS Capital region had a prescribing rate of 30.95% (95% CI, 29.49–32.46) in the 2005–2008 period that increased to 35.69% (95% CI, 34.70–36.70) in 2009–2012 (23.1% increase, P<.001) (Supplemental Fig. 3). This region had the highest opioid prescribing rate over the different time intervals, while the NYS Metropolitan region had the lowest rate of the four regions, with a peak prescribing rate of 22.81% (95% CI, 22.53–23.10) in 2009–2012 and a decrease to 15.77% (95% CI, 15.57–15.97) in 2016–2018 (30.1% reduction, P<.001).
Benzodiazepines
Differences in benzodiazepine prescribing rates were seen between age groups within the pre- and post-I-STOP periods, with the highest prescribing rates seen in subjects >55 years of age (P<.001) (Table 3 and Supplemental Fig. 4). The prescribing rate for females was approximately twice that of males within the pre- (female 15.46 vs. male 7.284; P<.0001) and post-I-STOP periods (female 14.76 vs. male 7.465; P<.001). Prescribing trends increased significantly for both sexes in the pre-I-STOP period followed by a significant yet subtle decreasing trend in the post-I-STOP period (Supplemental Table 2). The White non-Hispanic group had the highest rate of benzodiazepine prescribing during both time periods compared to the other race/ethnicity groups (P<.001). The benzodiazepine prescribing rate for the Black non-Hispanic group increased over the study periods from 3.878% to 4.162% (P=.003). The prescribing trend increased for the Black non-Hispanic group in the pre-I-STOP period (coefficient 0.4907; P<.0001) followed by a nonsignificant decrease in the post-I-STOP period (coefficient −0.0132; P=.7974).
Opioids and Benzodiazepines Co-prescribing
Opioid and benzodiazepine co-prescribing followed similar sociodemographic trends as the individual opioid and benzodiazepine groups (Table 3 and Supplemental Fig. 5). The highest prescribing rates were in those aged 36–55 years, and this was consistent in both the pre- and post-I-STOP periods (P<.001). Prescribing rates were consistently higher for females than males, and no changes were seen in the pre- and post-I-STOP periods for either sex (Table 3). The White non-Hispanic group had a higher prescribing rate than the other groups in both periods.
Relationship Between Patient-Level Factors and Prescribing Rates
In the multivariable analysis, factors associated with prescribing an opioid or benzodiazepine included female sex (aOR 1.388, 95% CI, 1.371–1.405; P<.001), higher comorbidity burden (CCI Score >4; aOR 1.461, 95% CI, 1.426–1.498; P<.001), location outside of the Metropolitan NYS region, and a previous pain diagnosis (Supplemental Table 3). Older age was associated with a lower odds of being prescribed an opioid or benzodiazepine (36–55 years; aOR 0.934, 95% CI, 0.923–0.947; P<.001 and >55 years; aOR 0.471, 95% CI, 0.461–0.483; P<.001). Compared to the White non-Hispanic group, other races/ethnicity groups were less likely to receive an opioid or benzodiazepine (all P<.001). The findings were similar for opioid and benzodiazepine co-prescribing.
DISCUSSION
This study merged two NYS DOH databases to provide estimates for opioid, benzodiazepine, and opioid/benzodiazepine prescribing rates among individuals with a primary AUD problem. Opioid prescribing rates increased during the pre-I-STOP period to reach a peak in 2012 followed by a significant decline thereafter. The prevalence of benzodiazepine and opioid/benzodiazepine co-prescription also increased in the early time periods, followed by slight declines. Notably, benzodiazepine and co-prescription rates did not decrease at the same rate as opioids in the post-I-STOP period. There were significant differences in prescribing rates based on sociodemographic factors including higher opioid, benzodiazepine, and co-prescription rates in females, White non-Hispanic persons, and rural regions.
Opioid prescribing among individuals with AUD was common, reaching a peak in 2012. Currently, the literature is sparse on the co-use of alcohol and opioids making direct comparisons difficult. Research in this area has focused on alcohol use in those using opioids or those with opioid use disorder (OUD) rather than evaluating an AUD-focused sample. Saha et al. examined the National Epidemiologic Survey on Alcohol and Related Conditions–III, a US population-based sample, and found that non-medical prescription opioid use and OUD increase the risk of having an AUD in adults.26 Hser et al. evaluated 5307 adult patients with OUD in an electronic health record database from 2006–2015 and found 23.4% had an AUD diagnosis.27 Similarly, secondary analyses aggregating treatment-seeking samples across ten National Institute on Drug Abuse clinical trials (n=1397) indicated that 38% had a comorbid AUD.28
The opioid prescribing rate changed following the introduction of the I-STOP program in 2013, with notable decreases overall and within each sociodemographic group. Brown et al. previously reported that the number of opioid prescriptions filled by pharmacies appeared to decrease after the I-STOP program was introduced in 2013 through to the end of the study in 2015.16 A systematic evaluation involving six states showed a relationship between reducing access to opioid prescriptions and increased overdose deaths.29 It is possible that reducing the availability of opioids has led patients to illicit opioids like heroin, which could lead to the unintended effect of increasing overdose deaths. Although we cannot definitively rule out other systematic factors as the reason for the decreasing trend, many such factors occurred both well before and well after the implementation of the I-STOP program. This includes increased national awareness of the opioid epidemic and the implementation of a 7-day supply limit for opioids to treat initial, acute pain in 2016. The introduction of this legislation shows that there was increasing awareness leading up to that point. However, the inflection point does seem to coincide more directly with the 2013 implementation of this program. Our observation of a recent decreasing trend related to alcohol and opioid co-use is pertinent given the impact of co-utilization on morbidity and mortality. Further studies focusing on opioid use in those with AUD are required.
We found that benzodiazepine and opioid/benzodiazepine prescribing in those with AUD has been declining since 2013, although the overall rate remains similar to the pre-2013 rate. This finding is disconcerting given the additive or synergistic effects of sedating substances such as alcohol and benzodiazepines and the effects of opioids on respiratory depression and healthcare outcomes.2, 6, 27, 28 A Drug Abuse Warning Network (DAWN) analysis reported that approximately 30% of benzodiazepine overdoses seen in EDs involved alcohol and 21% of benzodiazepine-related deaths involved alcohol.9 The growing trend in benzodiazepine prescribing is similar to that seen in the general population. A recent study evaluated the prevalence of opioid overdose deaths (OODs) between 1999 and 2017 using the Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research (WONDER) database.7 Over this timeframe, non-linear increases were seen in both alcohol and benzodiazepine co-involvement in OODs, and benzodiazepine prescribing rates were associated with OODs. Parallel increases in benzodiazepine prescribing and opioid-benzodiazepine co-prescription have been documented in recent years in a nationally representative US sample.29, 30 Votaw et al. also examined benzodiazepine use among those with a documented AUD using a general population sample.30 The authors found that 27.1% reported lifetime benzodiazepine use and 7.6% reported using within the past year. Individuals with co-occurring AUD and opioid use disorder reported the highest rates of benzodiazepine use in the past month. Novel approaches are required to reduce benzodiazepine and benzodiazepine/opioid co-prescribing in those with AUD to prevent overdoses and, ultimately, death.
We identified differences in opioid and benzodiazepine prescribing based on patient characteristics including race/ethnicity, geographic location, and sex. These findings are consistent with previous evidence evaluating disparities in the prescription of opioids and benzodiazepines.12, 21, 31,32,33,34 The current opioid epidemic has concentrated primarily on White communities with the literature documenting disparities based on implicit biases and reduced healthcare access.21, 31, 32, 35, 36 Previous literature has also shown that both Hispanic and Black patients are less likely to receive analgesics as compared to White patients.34, 37 Racial and ethnic disparities in prescribing practices extend to benzodiazepines where there are differences in the diagnosis of anxiety and other mental health conditions.21, 38 Opioid prescribing practices have also differed based on geographic location with higher opioid prescribing in nonmetropolitan (rural) counties. Garcia et al. showed that patients in rural areas within the USA had an 87% higher chance of receiving an opioid prescription.33 The authors attributed these increases to prescription drug misuse at an earlier age, higher prevalence of chronic pain among persons in rural areas, or a higher density of older adults who have a higher prevalence of pain conditions.33, 39, 40 Finally, a person’s sex assigned at birth has also played a role with women more likely to receive opioids and benzodiazepines.13, 41 The higher proportion of opioid prescribing has been linked to women seeking medical care more frequently and having a higher prevalence of chronic pain and anxiety disorders.13, 42 Discrepancies in the prescription of opioids and benzodiazepines continue to exist based on certain social-demographic patterns. Identifying high-risk groups based on a combination of factors is a necessary next step to better allocate interventions, treatments, and resources.
Our study has several limitations. First, the study included individuals that sought treatment for AUD at one of the NYS OASAS treatment centers. It is possible that prescribing patterns are different among individuals with polysubstance use who do not seek treatment; indeed, differences in patient characteristics, neuropsychiatric measures, and alcohol dependence have been reported between treatment-seeking and non-treatment-seeking individuals with alcohol dependence.33 Nevertheless, this remains one of the only studies to examine the co-use of opioids and benzodiazepines in individuals with a history of alcohol problems. Second, the collected sociodemographic characteristics were self-reported, so misclassification is possible; yet, we still detected rather large differences in prescribing patterns based on certain patient characteristics. Finally, we analyzed pharmacy prescription claims and these data can only capture claims paid through the NYS Medicaid system. It is possible that individuals obtained opioid or benzodiazepine prescriptions outside of Medicaid, so the number of opioid, benzodiazepine, or co-prescription users may be underrepresented.
CONCLUSION
We found that opioid prescribing increased in those with a primary AUD in the pre-I-STOP period and began to decrease in the post-I-STOP period. Overall benzodiazepine and co-prescribing rates remained unchanged between periods, although there was a notable decreasing trend following I-STOP implementation. There were significant differences in prescribing rates based on certain sociodemographic characteristics. Overall, opioid and benzodiazepine prescribing among this higher-risk group still occurred at high rates, representing an opportunity to develop innovative approaches to improve patient care and quality in those with alcohol and polysubstance use. Further research is needed to identify patients at greatest risk and continue to develop and integrate evidence-based interventions into treatment platforms.
References
Sacks JJ, Gonzales KR, Bouchery EE, Tomedi LE, Brewer RD. 2010 National and state costs of excessive alcohol consumption. Am J Prev Med. 2015;49(5):e73-e79.
Witkiewitz K, Vowles KE. Alcohol and opioid use, co-use, and chronic pain in the context of the opioid epidemic: a critical review. Alcohol Clin Exp Res. 2018;42(3):478-488.
Castle IJ, Dong C, Haughwout SP, White AM. Emergency department visits for adverse drug reactions involving alcohol: United States, 2005 to 2011. Alcohol Clin Exp Res. 2016;40(9):1913-1925.
Gonzales K, Roeber J, Kanny D, et al. Alcohol-attributable deaths and years of potential life lost-11 States, 2006-2010. Mmwr-Morbid Mortal W. 2014;63(10):213-216.
Serdarevic M, Gurka KK, Striley CW, Vaddiparti K, Cottler LB. Prevalence of concurrent prescription opioid and hazardous alcohol use among older women: results from a cross-sectional study of community members. J Commun Health. 2019;44(1):172-177.
Gudin JA, Mogali S, Jones JD, Comer SD. Risks, management, and monitoring of combination opioid, benzodiazepines, and/or alcohol use. Postgrad Med. 2013;125(4):115-130.
Tori ME, Larochelle MR, Naimi TS. Alcohol or benzodiazepine co-involvement with opioid overdose deaths in the United States, 1999-2017. JAMA Netw Open. 2020;3(4).
Frank D, Mateu-Gelabert P, Guarino H, et al. High risk and little knowledge: overdose experiences and knowledge among young adult nonmedical prescription opioid users. Int J Drug Policy. 2015;26(1):84-91.
Jones CM, Paulozzi LJ, Mack KA. Alcohol involvement in opioid pain reliever and benzodiazepine drug abuse-related emergency department visits and drug-related deaths - United States, 2010. Mmwr-Morbid Mortal W. 2014;63(40):881-885.
Landsman-Blumberg PB, Katz N, Gajria K, Coutinho AD, Yeung PP, White R. Burden of alcohol abuse or dependence among long-term opioid users with chronic noncancer pain. J Manag Care Spec Pharm. 2017;23(7):718-724.
Bachhuber MA, Hennessy S, Cunningham CO, Starrels JL. Increasing benzodiazepine prescriptions and overdose mortality in the United States, 1996-2013. Am J Public Health. 2016;106(4):686-688.
Votaw VR, Geyer R, Rieselbach MM, McHugh RK. The epidemiology of benzodiazepine misuse: a systematic review. Drug Alcohol Depend. 2019;200:95-114.
Hwang CS, Kang EM, Kornegay CJ, Staffa JA, Jones CM, McAninch JK. Trends in the concomitant prescribing of opioids and benzodiazepines, 2002-2014. Am J Prev Med. 2016;51(2):151-160.
Wilson MN, Hayden JA, Rhodes E, Robinson A, Asbridge M. Effectiveness of prescription monitoring programs in reducing opioid prescribing, dispensing, and use outcomes: a systematic review. J Pain. 2019;20(12):1383-1393.
I-STOP/PMP - Internet System for Tracking Over-Prescribin - Prescription Monitoring Program. New York State Department of Health. Available at: https://www.health.ny.gov/professionals/narcotic/prescription_monitoring/. Accessed on September 7, 2021.
Brown R, Riley MR, Ulrich L, et al. Impact of New York prescription drug monitoring program, I-STOP, on statewide overdose morbidity. Drug Alcohol Depend. 2017;178:348-354.
Pylypchuk Y, Parasrampuria S, Smiley C, Searcy T. Impact of electronic prescribing of controlled substances on opioid prescribing: evidence from I-STOP Program in New York. Med Care Res Rev. 2021:1077558721994994.
Olfson M, King M, Schoenbaum M. Benzodiazepine use in the United States. JAMA Psychiatry. 2015;72(2):136-142.
Vozoris NT. Benzodiazepine and opioid co-usage in the US population, 1999-2014: an exploratory analysis. Sleep. 2019;42(4).
Bertisch SM, Herzig SJ, Winkelman JW, Buettner C. National use of prescription medications for insomnia: NHANES 1999-2010. Sleep. 2014;37(2):343-+.
Friedman J, Kim D, Schneberk T, et al. Assessment of racial/ethnic and income disparities in the prescription of opioids and other controlled medications in California. JAMA Intern Med. 2019;179(4):469-476.
New York State County/Zip Code Perinatal Data Profile - 2016-2018. New York State Deparmtent of Health. Available at: https://www.health.ny.gov/statistics/chac/perinatal/county/2016-2018/. Accessed: April 12, 2021.
Glasheen WP, Cordier T, Gumpina R, Haugh G, Davis J, Renda A. Charlson Comorbidity Index: ICD-9 update and ICD-10 translation. Am Health Drug Benefits. 2019;12(4):188-197.
Romanelli RJ, Shah SN, Ikeda L, et al. Patient characteristics and healthcare utilization of a chronic pain population within an integrated healthcare system. Am J Manag Care. 2017;23(2):e50-e56.
Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299-309.
Saha TD, Kerridge BT, Goldstein RB, et al. Nonmedical prescription opioid use and DSM-5 nonmedical prescription opioid use disorder in the United States. J Clin Psychiatry. 2016;77(6):772-780.
Hser YI, Mooney LJ, Saxon AJ, Miotto K, Bell DS, Huang D. Chronic pain among patients with opioid use disorder: results from electronic health records data. J Subst Abuse Treat. 2017;77:26-30.
Hartzler B, Donovan DM, Huang Z. Comparison of opiate-primary treatment seekers with and without alcohol use disorder. J Subst Abuse Treat. 2010;39(2):114-123.
Lee B, Zhao W, Yang KC, Ahn YY, Perry BL. Systematic evaluation of state policy interventions targeting the US opioid epidemic, 2007-2018. Jama Netw Open. 2021;4(2):e2036687.
Votaw VR, Witkiewitz K, Valeri L, Bogunovic O, McHugh RK. Nonmedical prescription sedative/tranquilizer use in alcohol and opioid use disorders. Addict Behav. 2019;88:48-55.
Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc Natl Acad Sci U S A. 2016;113(16):4296-4301.
Chen I, Kurz J, Pasanen M, et al. Racial differences in opioid use for chronic nonmalignant pain. J Gen Intern Med. 2005;20(7):593-598.
Garcia MC, Heilig CM, Lee SH, et al. Opioid prescribing rates in nonmetropolitan and metropolitan counties among primary care providers using an electronic health record system - United States, 2014-2017. MMWR Morb Mortal Wkly Rep. 2019;68(2):25-30.
Todd KH, Samaroo N, Hoffman JR. Ethnicity as a risk factor for inadequate emergency department analgesia. Jama-J Am Med Assoc. 1993;269(12):1537-1539.
Song ZR. Mortality quadrupled among opioid-driven hospitalizations, notably within lower-income and disabled White populations. Health Affair. 2017;36(12):2054-2061.
Anderson KO, Green CR, Payne R. Racial and ethnic disparities in pain: causes and consequences of unequal care. J Pain. 2009;10(12):1187-1204.
Todd KH, Deaton C, D'Adamo AP, Goe L. Ethnicity and analgesic practice. Ann Emerg Med. 2000;35(1):11-16.
Stockdale SE, Lagomasino IT, Siddique J, McGuire T, Miranda J. Racial and ethnic disparities in detection and treatment of depression and anxiety among psychiatric and primary health care visits, 1995-2005. Med Care. 2008;46(7):668-677.
Keyes KM, Cerda M, Brady JE, Havens JR, Galea S. Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. Am J Public Health. 2014;104(2):e52-59.
Monnat SM, Rigg KK. Examining rural/urban differences in prescription opioid misuse among US adolescents. J Rural Health. 2016;32(2):204-218.
Agarwal SD, Landon BE. Patterns in outpatient benzodiazepine prescribing in the United States. Jama Netw Open. 2019;2(1):e187399
Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(1):8-19.
Funding
This work was supported by the National Institutes of Health (grant R21/R33 AA026954 to Drs. Leonard & Elkin and grant K23 HL153582 to Dr. Jacobs). This work was supported in part by the National Center for Advancing Translational Sciences award UL1 TR001412 to the University at Buffalo. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data, preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Dr. Jacobs had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Jacobs, Tober, and Lu
Acquisition, analysis, or interpretation of data: all authors
Drafting of the manuscript: Jacobs and Tober
Critical revision of the manuscript for important intellectual content: all authors
Statistical analysis: Jacobs and Tober
Obtained funding: Leonard and Elkin
Supervision: Jacobs
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior Presentations: The preliminary results were previously presented as a virtual poster at the Annual Meeting of the American College of Clinical Pharmacy, October 2021.
Supplementary information
ESM 1
(DOCX 1473 kb)
Rights and permissions
About this article
Cite this article
Jacobs, D.M., Tober, R., Yu, C. et al. Trends in Prescribing Opioids, Benzodiazepines, and Both Among Adults with Alcohol Use Disorder in New York State. J GEN INTERN MED 38, 138–146 (2023). https://doi.org/10.1007/s11606-022-07682-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-022-07682-3