Abstract
Background
Data on the impact of hospital volume and travel distance on patient outcomes after major abdominal surgery remain poorly defined. We sought to characterize the relationship of travel distance, hospital volume, and long-term outcomes of patients undergoing surgical resection of hepatocellular carcinoma (HCC).
Methods
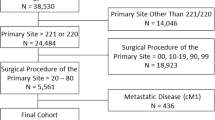
The 2004–2015 National Cancer Database was used to identify patients who underwent resection of HCC. Patients were stratified according to travel distance and hospital volume quartiles, and multivariable regression models were utilized to examine the impact of travel distance, hospital volume, and travel distance/hospital volume on overall survival (OS).
Results
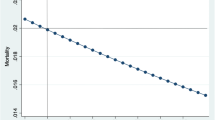
Among the 12,266 patients identified, procedures included wedge/segmental resections (N = 7354, 59.9%), hemi-hepatectomy (N = 4003, 32.6%), and extended hepatectomy (N = 909, 7.5%). Stratifying data into quartiles, travel distance to surgical care was ≤ 5.7 miles (mi), > 5.7–14.2 mi, > 14.2–44.4 mi, and ≥ 44.4 mi, while hospital volume quartiles determined on the hospital level were ≤ 1 case per year, 1.1–4, 4.1–12.5, and ≥ 12.5. On multivariable analysis, increased hospital volume was associated with decreased hazard of mortality (HR 0.69, 95% CI 0.45–0.82, p < 0.001). Travel distance was not significantly associated with hazard of mortality. Furthermore, only hospital volume was associated with mortality (HR 0.67, 95% CI 0.56–0.80, p < 0.001) after controlling for both travel distance and hospital volume.
Conclusions
Only hospital volume was associated with increased hazard of mortality. The benefits of undergoing resection for HCC at a high-volume hospital appear to outweigh the inconvenience of longer travel distances.


Similar content being viewed by others
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108.
Beal EW, Tumin D, Kabir A, Moris D, Zhang XF, Chakedis J, et al. Cohort Contributions to Race- and Gender-Specific Trends in the Incidence of Hepatocellular Carcinoma in the USA. World J Surg. 2018;42(3):835–40.
Kulik L, El-Serag HB. Epidemiology and Management of Hepatocellular Carcinoma. Gastroenterology. 2018.
Wong RJ, Aguilar M, Cheung R, Perumpail RB, Harrison SA, Younossi ZM, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015;148(3):547–55.
Marrero JA, Kulik LM, Sirlin CB, Zhu AX, Finn RS, Abecassis MM, et al. Diagnosis, Staging, and Management of Hepatocellular Carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2018;68(2):723–50.
Agarwal PD, Phillips P, Hillman L, Lucey MR, Lee F, Mezrich JD, et al. Multidisciplinary Management of Hepatocellular Carcinoma Improves Access to Therapy and Patient Survival. J Clin Gastroenterol. 2017;51(9):845–9.
Yopp AC, Mansour JC, Beg MS, Arenas J, Trimmer C, Reddick M, et al. Establishment of a multidisciplinary hepatocellular carcinoma clinic is associated with improved clinical outcome. Ann Surg Oncol. 2014;21(4):1287–95.
Mokdad AA, Zhu H, Marrero JA, Mansour JC, Singal AG, Yopp AC. Hospital Volume and Survival After Hepatocellular Carcinoma Diagnosis. Am J Gastroenterol. 2016;111(7):967–75.
Chapman BC, Paniccia A, Hosokawa PW, Henderson WG, Overbey DM, Messersmith W, et al. Impact of Facility Type and Surgical Volume on 10-Year Survival in Patients Undergoing Hepatic Resection for Hepatocellular Carcinoma. J Am Coll Surg. 2017;224(3):362–72.
Holliday EB, Allen PK, Elhalawani H, Abdel-Rahman O. Treatment at a high-volume centre is associated with improved survival among patients with non-metastatic hepatocellular carcinoma. Liver Int. 2018;38(4):665–75.
Sato M, Tateishi R, Yasunaga H, Matsui H, Fushimi K, Ikeda H, et al. Association between hospital volume and in-hospital mortality following radiofrequency ablation for hepatocellular carcinoma. BJS Open. 2017;1(2):50–4.
Lu LC, Shao YY, Kuo RN, Lin ZZ, Yeh YC, Shau WY, et al. Hospital volume of percutaneous radiofrequency ablation is closely associated with treatment outcomes for patients with hepatocellular carcinoma. Cancer. 2013;119(6):1210–6.
Ross K, Patzer RE, Goldberg DS, Lynch RJ. Sociodemographic Determinants of Waitlist and Posttransplant Survival Among End-Stage Liver Disease Patients. Am J Transplant. 2017;17(11):2879–89.
Lidsky ME, Sun Z, Nussbaum DP, Adam MA, Speicher PJ, Blazer DG. Going the Extra Mile: Improved Survival for Pancreatic Cancer Patients Traveling to High-volume Centers. Ann Surg. 2017;266(2):333–8.
**a L, Taylor BL, Mamtani R, Christodouleas JP, Guzzo TJ. Associations Between Travel Distance, Hospital Volume, and Outcomes Following Radical Cystectomy in Patients With Muscle-invasive Bladder Cancer. Urology. 2018;114:87–94.
Boffa DJ, Rosen JE, Mallin K, Loomis A, Gay G, Palis B, et al. Using the National Cancer Database for Outcomes Research: A Review. JAMA Oncol. 2017;3(12):1722–8.
NCDB. Getting Started - A User's Guide. 2015.
**dal M, Zheng C, Quadri HS, Ihemelandu CU, Hong YK, Smith AK, et al. Why Do Long-Distance Travelers Have Improved Pancreatectomy Outcomes? J Am Coll Surg. 2017;225(2):216–25.
Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349(22):2117–27.
Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346(15):1128–37.
Bagaria SP, Chang YH, Gray RJ, Ashman JB, Attia S, Wasif N. Improving Long-Term Outcomes for Patients with Extra-Abdominal Soft Tissue Sarcoma Regionalization to High-Volume Centers, Improved Compliance with Guidelines or Both? Sarcoma. 2018;2018:8141056.
Dudley RA, Johansen KL, Brand R, Rennie DJ, Milstein A. Selective referral to high-volume hospitals: estimating potentially avoidable deaths. JAMA. 2000;283(9):1159–66.
Hata T, Motoi F, Ishida M, Naitoh T, Katayose Y, Egawa S, et al. Effect of Hospital Volume on Surgical Outcomes After Pancreaticoduodenectomy: A Systematic Review and Meta-analysis. Ann Surg. 2016;263(4):664–72.
Markar SR, Mackenzie H, Wiggins T, Askari A, Karthikesalingam A, Faiz O, et al. Influence of national centralization of oesophagogastric cancer on management and clinical outcome from emergency upper gastrointestinal conditions. Br J Surg. 2018;105(1):113–20.
Idrees JJ, Merath K, Gani F, Bagante F, Mehta R, Beal E, et al. Trends in centralization of surgical care and compliance with National Cancer Center Network guidelines for resected cholangiocarcinoma. HPB (Oxford). 2018.
Barrington DA, Dilley SE, Landers EE, Thomas ED, Boone JD, Straughn JM, et al. Distance from a Comprehensive Cancer Center: A proxy for poor cervical cancer outcomes? Gynecol Oncol. 2016;143(3):617–21.
Bilimoria KY, Ko CY, Tomlinson JS, Stewart AK, Talamonti MS, Hynes DL, et al. Wait times for cancer surgery in the United States: trends and predictors of delays. Ann Surg. 2011;253(4):779–85.
Tomaszewski JJ, Handorf E, Corcoran AT, Wong YN, Mehrazin R, Bekelman JE, et al. Care transitions between hospitals are associated with treatment delay for patients with muscle invasive bladder cancer. J Urol. 2014;192(5):1349–54.
Xu Z, Becerra AZ, Justiniano CF, Boodry CI, Aquina CT, Swanger AA, et al. Is the Distance Worth It? Patients With Rectal Cancer Traveling to High-Volume Centers Experience Improved Outcomes. Dis Colon Rectum. 2017;60(12):1250–9.
Lafaro K, Grandhi MS, Herman JM, Pawlik TM. The importance of surgical margins in primary malignancies of the liver. J Surg Oncol. 2016;113(3):296–303.
Dong S, Wang Z, Wu L, Qu Z. Effect of surgical margin in R0 hepatectomy on recurrence-free survival of patients with solitary hepatocellular carcinomas without macroscopic vascular invasion. Medicine (Baltimore). 2016;95(44):e5251.
Hu W, Pang X, Guo W, Wu L, Zhang B. Relationship of different surgical margins with recurrence-free survival in patients with hepatocellular carcinoma. Int J Clin Exp Pathol. 2015;8(3):3404–9.
Mesman R, Westert GP, Berden BJ, Faber MJ. Why do high-volume hospitals achieve better outcomes? A systematic review about intermediate factors in volume-outcome relationships. Health Policy. 2015;119(8):1055–67.
NCCN. NCCN Guidelines Version 5.2018: Hepatocellular Carcinoma. 2018.
Zhang J, Mavros MN, Cosgrove D, Hirose K, Herman JM, Smallwood-Massey S, et al. Impact of a single-day multidisciplinary clinic on the management of patients with liver tumours. Curr Oncol. 2013;20(2):e123–31.
Delitto D, Black BS, Cunningham HB, Sliesoraitis S, Lu X, Liu C, et al. Standardization of surgical care in a high-volume center improves survival in resected pancreatic head cancer. Am J Surg. 2016;212(2):195–201.e1.
Edwards EB, Roberts JP, McBride MA, Schulak JA, Hunsicker LG. The effect of the volume of procedures at transplantation centers on mortality after liver transplantation. N Engl J Med. 1999;341(27):2049–53.
Axelrod DA, Guidinger MK, McCullough KP, Leichtman AB, Punch JD, Merion RM. Association of center volume with outcome after liver and kidney transplantation. Am J Transplant. 2004;4(6):920–7.
Edwards EB, Harper AM, Hirose R, Mulligan DC. The impact of broader regional sharing of livers: 2-year results of "Share 35". Liver Transpl. 2016;22(4):399–409.
Nguyen GC, Thuluvath NP, Segev DL, Thuluvath PJ. Volumes of liver transplant and partial hepatectomy procedures are independently associated with lower postoperative mortality following resection for hepatocellular carcinoma. Liver Transpl. 2009;15(7):776–81.
Bilimoria KY, Bentrem DJ, Stewart AK, Winchester DP, Ko CY. Comparison of Commission on Cancer-approved and -nonapproved hospitals in the United states: Implications for studies that use the National Cancer Data Base. J Clin Oncol. 2009;27(25):4177–81.
Author information
Authors and Affiliations
Contributions
EWB, RM, DIT, AP, KM, MED, JC, AE, and TMP conceived of and designed this work. RM and EWB performed data analysis. EWB drafted the manuscript. EWB, RM, AP, KM, MED, JC, AE, and TMP critically revised the manuscript, provided approval of the final version, and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Beal, E.W., Mehta, R., Merath, K. et al. Outcomes After Resection of Hepatocellular Carcinoma: Intersection of Travel Distance and Hospital Volume. J Gastrointest Surg 23, 1425–1434 (2019). https://doi.org/10.1007/s11605-019-04233-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04233-w