Summary
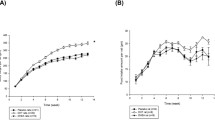
The effect of high concentrations of testosterone on ovarian follicle development was investigated. Primary follicles and granulosa cells were cultured in vitro in media supplemented with a testosterone concentration gradient. The combined effects of testosterone and follicle-stimulating hormone (FSH) on follicular growth and granulosa cell gonadotropin receptor mRNA expression were also investigated. Follicle growth in the presence of high testosterone concentrations was promoted at early stages (days 1–7), but inhibited at later stage (days 7–14) of in vitro culture. Interestingly, testosterone-induced follicle development arrest was rescued by treatment with high concentrations of FSH (400 mIU/mL). In addition, in cultured granulosa cells, high testosterone concentrations induced cell proliferation, and increased the mRNA expression level of FSH receptor (FSHR), and luteinized hormone/choriogonadotropin receptor. It was concluded that high concentrations of testosterone inhibited follicle development, most likely through regulation of the FSH signaling pathway, although independently from FSHR downregulation. These findings are an important step in further understanding the pathogenesis of polycystic ovary syndrome.
Similar content being viewed by others
References
Luo W, Gumen A, Haughian JM, et al. The role of luteinizing hormone in regulating gene expression during selection of a dominant follicle in cattle. Biol Reprod, 2011,84(2):369–378
Wigglesworth K, Lee KB, O'Brien MJ, et al. Bidirectional communication between oocytes and ovarian follicular somatic cells is required for meiotic arrest of mammalian oocytes. Proc Natl Acad Sci USA, 2013,110(39):E3723–3729
Cheng XB, Jimenez M, Desai R, et al. Characterizing the neuroendocrine and ovarian defects of androgen receptor-knockout female mice. Am J Physiol Endocrinol Metab, 2013,305(6):E717–726
Hossain MM, Cao M, Wang Q, et al. Altered expression of miRNAs in a dihydrotestosterone-induced rat PCOS model. J Ovarian Res, 2013,6(1):36
Zhang CP, Yang JL, Zhang J, et al. Notch signaling is involved in ovarian follicle development by regulating granulosa cell proliferation. Endocrinology, 2011,152(6): 2437–2447
Knight PG, Glister C. Potential local regulatory functions of inhibins, activins and follistatin in the ovary. Reproduction, 2001,121(4):503–512
Lenie S, Smitz J. Functional AR signaling is evident in an in vitro mouse follicle culture bioassay that encompasses most stages of folliculogenesis. Biol Reprod, 2009,80(4):685–695
Sánchez F, Adriaenssens T, Romero S, et al. Different follicle-stimulating hormone exposure regimens during antral follicle growth alter gene expression in the cumulus-oocyte complex in mice. Biol Reprod, 2010,83(4):514–524
Gelmann EP. Molecular biology of the androgen receptor. J Clin Oncol, 2002,20(13):3001–3015
Sorokin SP, Hoyt RF ffixJr, McNelly NA. Factors influencing fetal macrophage development: I. Reactions of the tumor necrosis factor-alpha cascade and their inhibitors. Anat Rec, 1996,246(4):481–497
Stocco C. Tissue physiology and pathology of aromatase. Steroids, 2012,77(1–2): 27–35
Tetsuka M, Whitelaw PF, Bremner WJ, et al. Developmental regulation of androgen receptor in rat ovary. J Endocrinol, 1995,145(3):535–543
Hillier SG, Tetsuka M. Role of androgens in follicle maturation and atresia. Baillieres Clin Obstet Gynaecol, 1997,11(2):249–260
Weil SJ, Vendola K, Zhou J, et al. Androgen receptor gene expression in the primate ovary: cellular localization, regulation, and functional correlations. J Clin Endocrinol Metab, 1998,83(7):2479–285
Yang MY, Fortune JE. Testosterone stimulates the primary to secondary follicle transition in bovine follicles in vitro. Biol Reprod, 2006,75(6):924–932
Sen A, Hammes SR. Granulosa cell-specific androgen receptors are critical regulators of ovarian development and function. Mol Endocrinol, 2010,24(7):1393–1403
McKenna TJ, Loughlin T, Daly L, et al. Variable clinical and hormonal manifestations of hyperandrogenemia. Metabolism, 1984,33(8):714–717
Loughlin T, Cunningham SK, Culliton M, et al. Altered androstenedione and estrone dynamics associated with abnormal hormonal profiles in amenorrheic subjects with weight loss or obesity. Fertil Steril, 1985,43(5):720–725
Dunaif A. Insulin resistance and the polycystic ovary syndrome: mechanism and implications for pathogenesis. Endocr Rev, 1997,18(6):774–800
Walters KA, Allan CM, Handelsman DJ. Rodent models for human polycystic ovary syndrome. Biol Reprod, 2012,86(5):149, 1–12
Balen AH, Conway GS, Kaltsas G, et al. Polycystic ovary syndrome: the spectrum of the disorder in 1741 patients. Hum Reprod, 1995,6(8):2107–2111
Wachs DS, Coffler MS, Malcom PJ, et al. Increased androgen response to follicle-stimulating hormone administration in women with polycystic ovary syndrome. J Clin Endocrinol Metab, 2008,93(5):1827–1833
Teissier MP, Chable H, Paulhac S, et al. Comparison of follicle steroidogenesis from normal and polycystic ovaries in women undergoing IVF: relationship between steroid concentrations, follicle size, oocyte quality and fecundability. Hum Reprod, 2000,15(12):2471–2477
Jabara S, Coutifaris C. In vitro fertilization in the PCOS patient: clinical considerations. Semin Reprod Med, 2003, 21(3):317–324
Caldwell AS, Middleton LJ, Jimenez M, et al. Characterization of reproductive, metabolic, and endocrine features of polycystic ovary syndrome in female hyperandrogenic mouse models. Endocrinology, 2014,155(8):3146–3159
Daniel SA, Armstrong DT. Enhancement of follicle-stimulating hormone-induced aromatase activity by androgens in cultured rat granulosa cells. Endocrinology, 1980,107(4):1027–1033
Fulghesu AM, Apa R, Belosi C, et al. Recombinant versus urinary follicle-stimulating hormone in the low-dose regimen in anovulatory patients with polycystic ovary syndrome: a safer and more effective treatment. Horm Res, 2001,55(5):224–228
Ajossa S, Guerriero S, Paoletti AM, et al. The treatment of polycystic ovary syndrome. Minerva Ginecol, 2004,56(1): 15–26
Duda M, Durlej-Grzesiak M, Tabarowski Z, et al. Effects of testosterone and 2-hydroxyflutamide on progesterone receptor expression in porcine ovarian follicles in vitro. Reprod Biol, 2012,12(4):333–340
Itami S, Yasuda K, Yoshida Y, et al. Co-culturing of follicles with interstitial cells in collagen gel reproduced follilcular development accompanied with theca cell layer formation. Reprod Biol Endocrinol, 2011,17(9):159
Zhao KK, Cui YG, Jiang YQ, et al. Effect of HSP10 on apoptosis induced by testosterone in cultured mouse ovarian granulosa cells. Eur J Obstet Gynecol Reprod Biol, 2013,171(2):301–306
Alexandraki KI, Kaltsas GA. Endocrinopathies and other disorders inducing a polycystic ovary syndrome phenotype. Front Horm Res, 2013,40:142–157
Luchetti CG, Solano ME, Sander V, et al. Effects of dehydroepiandrosterone on ovarian cystogenesis and immune function. J Reprod Immunol, 2004,64(1–2):59–74
Sander V, Luchetti CG, Solano ME, et al. Role of the N, N'-dimethylbiguanide metformin in the treatment of female prepuberal BALB/c mice hyperandrogenized with dehydroepiandrosterone. Reproduction, 2006,131(3):591–602
Barad DH, Gleicher N. Increased oocyte production after treatment with dehydroepiandrosterone. Fertil Steril, 2005, 84(3):756
Gleicher N, Weghofer A, Barad DH. The role of androgens in follicle maturation and ovulation induction: friend or foe of infertility treatment? Reprod Biol Endocrinol, 2011,17(9):116
Walters KA, Allan CM, Handelsman DJ. Androgen actions and the ovary. Biol Reprod, 2008,78(3):380–389
Vendola KA, Zhou J, Adesanya OO, et al. Androgens stimulate early stages of follicular growth in the primate ovary. J Clin Invest, 1998,101(12):2622–2629
Pradeep PK, Li X, Peegel H, et al. Dihydrotestosterone inhibits granulosa cell proliferation by decreasing the cyclin D2 mRNA expression and cell cycle arrest at G1 phase. Endocrinology, 2002,143(8):2930–2935
Wang Q, Leader A, Tsang BK. Follicular stage-dependent regulation of apoptosis and steroidogenesis by prohibitin in rat granulosa cells. J Ovarian Res, 2013,6(1):23
Kriplani A, Agarwal N. Effects of metformin on clinical and biochemical parameters in polycystic ovary syndrome. J Reprod Med, 2004,49(5):361–367
Elia E, Sander V, Luchetti CG, et al. The mechanisms involved in the action of metformin in regulating ovarian function in hyperandrogenized mice. Mol Hum Reprod, 2006,12(8):475–481
Belgorosky D, Sander VA, Yorio MP, et al. Hyperandrogenism alters intraovarian parameters during early folliculogenesis in mice. Reprod Biomed Online, 2010,20(6): 797–807
Gervásio CG, Bernuci MP, Silva-de-Sá MF, et al. The role of androgen hormones in early follicular development. ISRN Obstet Gynecol, 2014,10(2014):818010.
Mersereau JE, Evans ML, Moore DH, et al. Luteal phase estrogen is decreased in regularly menstruating older women compared with a reference population of younger women. Menopause, 2008,15(3):482–486
Passos MJ, Vasconcelos GL, Silva AW, et al. Accelerated growth of bovine preantral follicles in vitro after stimulation with both FSH and BMP-15 is accompanied by ultrastructural changes and increased atresia. Theriogenology, 2013,79(9):1269–1277
Chaves RN, Duate AB, Rodrigues GQ, et al. The effects of insulin and follicle-simulating hormone (FSH) during in vitro development of ovariangoat preantral follicles and the relative mRNA expression for insulin and FSH receptors and cytochrome P450 aromatase in cultured follicles. Biol Reprod, 2012,87(3):69
Chen ZJ, Shi YH, Li Y, et al. Clinical analysis of assistant treatment proposals for infertile women with polycystic ovary syndrome. Zhonghua Fu Chan Ke Za Zhi (Chinese), 2008,43(8):571–575
Laisk T, Haller-Kikkatalo K, Laanpere M, et al. Androgen receptor epigenetic variations influence early follicular phase gonadotropin levels. Acta Obstet Gynecol Scand, 2010,89(12):1557–1563
Chen ZJ, Zhao H, He L, et al. Genome-wide association study identifies susceptibility loci for polycystic ovary syndrome on chromosome 2p16.3, 2p21 and 9q33.3. Nat Genet, 2011,43(1):55–59
Author information
Authors and Affiliations
Corresponding authors
Additional information
These authors contributed equally to this work.
This project was supported by grants from the National Basic Research Program of China (973 program) (Nos. 2012CB944700 and 2011CB944502), the National Natural Science Foundation of China (No. 31371453), the Scientific Research Foundation of Shandong Province of Outstanding Young Scientist (No. 2012BSE27089), and 2012 Shandong Province Post-Doctoral Innovation Foundation (Nos. 201102017 and 201203052).
Rights and permissions
About this article
Cite this article
Liu, T., Cui, Yq., Zhao, H. et al. High levels of testosterone inhibit ovarian follicle development by repressing the FSH signaling pathway. J. Huazhong Univ. Sci. Technol. [Med. Sci.] 35, 723–729 (2015). https://doi.org/10.1007/s11596-015-1497-z
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-015-1497-z