Abstract
Purpose
It is unknown whether the effect of increased distal stabilization can trigger the onset of the supraspinatus and infraspinatus muscles, and if handgrip strength levels can elicit early proximal shoulder stabilization. Hence, we aimed to compare the electromyography activation of the Supraspinatus and Infraspinatus muscles during the abduction motion with handgrip strength in different levels (0%, 30%, and 60%) of maximal voluntary isometric contraction (MVIC).
Methods
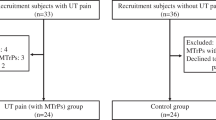
Twenty participants were submitted to abduction shoulder movement with three different handgrip strengths (0%, 30%, and 60%) using electromyography. The onset of Supraspinatus and Infraspinatus muscles was measured. A Friedman’s test was used to compare handgrip conditions and the onset between muscles. Then, multiple comparisons were performed. All alpha errors were set to 5%.
Results
There was an anticipated onset for Supraspinatus muscle at 0% of the MVIC {− 0.554 [− 0.657 to − 0.497] ms vs. − 0.098 [− 0.264 to 0.108] ms, p < 0.001}, at 30% of the MVIC {− 0.560 [− 0.628 to − 0.521] ms vs. − 0.125 [− 0.243 to − 0.031] ms, p < 0.001), and at 60% of the MVIC {− 0.543 [− 0.573 to − 0.514] ms vs. − 0.215 [− 0.325 to − 0.017] ms, p = 0.001}.
Conclusion
Shoulder abduction with handgrip triggers the onset of the Supraspinatus and Infraspinatus muscles. The Supraspinatus muscle elicits an anticipated onset. Two stabilizing strategies are suggested; the internal rotation instability capable be induced by the deltoid muscles (abduction movement) and from the wrist flexor-pronator muscles (handgrip). Both tasks are counteracted and anticipated by the action of the Supraspinatus and Infraspinatus muscles.


Similar content being viewed by others
References
Muratori LM, Lamberg EM, Quinn L, Duff SV (2013) Applying principles of motor learning and control to upper extremity rehabilitation. J Hand Ther 26:94–102. https://doi.org/10.1016/j.jht.2012.12.007 (quiz 103)
Day A, Taylor NF, Green RA (2012) The stabilizing role of the rotator cuff at the shoulder–responses to external perturbations. Clin Biomech (Bristol, Avon) 27:551–556. https://doi.org/10.1016/j.clinbiomech.2012.02.003
Reinold MM, Escamilla RF, Wilk KE (2009) Current concepts in the scientific and clinical rationale behind exercises for glenohumeral and scapulothoracic musculature. J Orthop Sports Phys Ther 39:105–117. https://doi.org/10.2519/jospt.2009.2835
Veeger HEJ, van der Helm FCT (2007) Shoulder function: the perfect compromise between mobility and stability. J Biomech 40:2119–2129. https://doi.org/10.1016/j.jbiomech.2006.10.016
Matsen FA, Chebli C, Lippitt S, American Academy of Orthopaedic Surgeons (2006) Principles for the evaluation and management of shoulder instability. J Bone Joint Surg Am 88:648–659. https://doi.org/10.2106/00004623-200603000-00026
Wickham J, Pizzari T, Stansfeld K et al (2010) Quantifying “normal” shoulder muscle activity during abduction. J Electromyogr Kinesiol 20:212–222. https://doi.org/10.1016/j.jelekin.2009.06.004
Saeterbakken AH, Stien N, Pedersen H et al (2021) The effect of grip width on muscle strength and electromyographic activity in bench press among novice- and resistance-trained men. Int J Environ Res Public Health 18:6444. https://doi.org/10.3390/ijerph18126444
Linaker CH, Walker-Bone K (2015) Shoulder disorders and occupation. Best Pract Res Clin Rheumatol 29:405–423. https://doi.org/10.1016/j.berh.2015.04.001
Lewis CL, Laudicina NM, Khuu A, Loverro KL (2017) The human pelvis: variation in structure and function during gait. Anat Rec (Hoboken) 300:633–642. https://doi.org/10.1002/ar.23552
Escamilla RF, Yamashiro K, Paulos L, Andrews JR (2009) Shoulder muscle activity and function in common shoulder rehabilitation exercises. Sports Med 39:663–685. https://doi.org/10.2165/00007256-200939080-00004
Cricchio M, Frazer C (2011) Scapulothoracic and scapulohumeral exercises: a narrative review of electromyographic studies. J Hand Ther 24:322–333. https://doi.org/10.1016/j.jht.2011.06.001 (quiz 334)
Kang J-I, Moon Y-J, Choi H et al (2016) The effect of exercise types for rotator cuff repair patients on activities of shoulder muscles and upper limb disability. J Phys Ther Sci 28:2772–2777. https://doi.org/10.1589/jpts.28.2772
Alizadehkhaiyat O, Fisher AC, Kemp GJ et al (2011) Shoulder muscle activation and fatigue during a controlled forceful hand grip task. J Electromyogr Kinesiol 21:478–482. https://doi.org/10.1016/j.jelekin.2011.03.002
Horsley I, Herrington L, Hoyle R et al (2016) Do changes in hand grip strength correlate with shoulder rotator cuff function? Shoulder Elbow 8:124–129. https://doi.org/10.1177/1758573215626103
Sporrong H, Palmerud G, Herberts P (1996) Hand grip increases shoulder muscle activity, an EMG analysis with static hand contractions in 9 subjects. Acta Orthop Scand 67:485–490. https://doi.org/10.3109/17453679608996674
Sporrong H, Palmerud G, Herberts P (1995) Influences of handgrip on shoulder muscle activity. Eur J Appl Physiol Occup Physiol 71:485–492. https://doi.org/10.1007/BF00238549
Shenouda M, El-Tokhy M (2014) Efficacy of hand grip strength on supraspinatus muscle activity in patients with shoulder im**ement syndrome. Indian J Physiother Occup Ther 8(1):187–197. https://doi.org/10.5958/j.0973-5674.8.1.036
Rodriguez-Yunta E (2004) Committees of ethical and scientific evaluation for research in human beings and the guidelines CIOMS 2002. Acta bioeth 10(1):37–47. https://doi.org/10.4067/S1726-569X2004000100005
Armstrong CA, Oldham JA (1999) A comparison of dominant and non-dominant hand strengths. J Hand Surg Br 24:421–425. https://doi.org/10.1054/jhsb.1999.0236
Gerodimos V, Karatrantou K, Psychou D et al (2017) Static and dynamic handgrip strength endurance: test-retest reproducibility. J Hand Surg Am 42:e175–e184. https://doi.org/10.1016/j.jhsa.2016.12.014
John B, de Luca C (1985) Muscles alive: their functions revealed by electromyography, 5th edn. Williams & Wilkins, Baltimore
Perotto A, Delagi E, Iazzetti J, Morrison D (2005) Anatomical guide for the electromyographer: the limbs and trunk, illustrated ed. Charles C Thomas Publisher, LTD, Springfield
Criswell E, Cram J (2010) CRAM’S introduction to surface electromyography, 2nd ed. Jones and Bartlett Publishers, LLC, Sadbury
Papagiannis GI, Triantafyllou AI, Roumpelakis IM et al (2019) Methodology of surface electromyography in gait analysis: review of the literature. J Med Eng Technol 43:59–65. https://doi.org/10.1080/03091902.2019.1609610
Glousman R, Jobe F, Tibone J et al (1988) Dynamic electromyographic analysis of the throwing shoulder with glenohumeral instability. J Bone Joint Surg Am 70:220–226
Myers JB, Riemann BL, Ju Y-Y et al (2003) Shoulder muscle reflex latencies under various levels of muscle contraction. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-200302000-00017
Cools AM, Witvrouw EE, Declercq GA et al (2003) Scapular muscle recruitment patterns: trapezius muscle latency with and without im**ement symptoms. Am J Sports Med 31:542–549. https://doi.org/10.1177/03635465030310041101
David G, Magarey ME, Jones MA et al (2000) EMG and strength correlates of selected shoulder muscles during rotations of the glenohumeral joint. Clin Biomech (Bristol, Avon) 15:95–102. https://doi.org/10.1016/s0268-0033(99)00052-2
Rajaratnam BS, Goh JC, Kumar PV (2013) Control strategies to re-establish glenohumeral stability after shoulder injury. BMC Sports Sci Med Rehabil 5:26. https://doi.org/10.1186/2052-1847-5-26
Vosloo M, Keough N, De Beer MA (2017) The clinical anatomy of the insertion of the rotator cuff tendons. Eur J Orthop Surg Traumatol 27:359–366. https://doi.org/10.1007/s00590-017-1922-z
Seo NJ, Armstrong TJ, Ashton-Miller JA, Chaffin DB (2008) Wrist strength is dependent on simultaneous power grip intensity. Ergonomics 51:1594–1605. https://doi.org/10.1080/00140130802216925
Davidson PA, Pink M, Perry J, Jobe FW (1995) Functional anatomy of the flexor pronator muscle group in relation to the medial collateral ligament of the elbow. Am J Sports Med 23:245–250. https://doi.org/10.1177/036354659502300220
Antony NT, Keir PJ (2010) Effects of posture, movement and hand load on shoulder muscle activity. J Electromyogr Kinesiol 20:191–198. https://doi.org/10.1016/j.jelekin.2009.04.010
Reed D, Cathers I, Halaki M, Ginn K (2013) Does supraspinatus initiate shoulder abduction? J Electromyogr Kinesiol 23:425–429. https://doi.org/10.1016/j.jelekin.2012.11.008
Phillips D, Kosek P, Karduna A (2018) The contribution of the supraspinatus muscle at sub-maximal contractions. J Biomech 68:65–69. https://doi.org/10.1016/j.jbiomech.2017.12.015
Alpert SW, Pink MM, Jobe FW et al (2000) Electromyographic analysis of deltoid and rotator cuff function under varying loads and speeds. J Shoulder Elbow Surg 9:47–58. https://doi.org/10.1016/s1058-2746(00)90009-0
Dyrna F, Kumar NS, Obopilwe E et al (2018) Relationship between deltoid and rotator cuff muscles during dynamic shoulder abduction: a biomechanical study of rotator cuff tear progression. Am J Sports Med 46:1919–1926. https://doi.org/10.1177/0363546518768276
Spall P, Ribeiro DC, Sole G (2016) Electromyographic activity of shoulder girdle muscles in patients with symptomatic and asymptomatic rotator cuff tears: a systematic review and meta-analysis. PM R 8:894–906. https://doi.org/10.1016/j.pmrj.2016.02.015
Veen EJD, Koorevaar CT, Verdonschot KHM et al (2021) Compensatory movement patterns are based on abnormal activity of the biceps brachii and posterior deltoid muscles in patients with symptomatic rotator cuff tears. Clin Orthop Relat Res 479:378–388. https://doi.org/10.1097/CORR.0000000000001555
Sperling L, Dahlman S, Wikström L et al (1993) A cube model for the classification of work with hand tools and the formulation of functional requirements. Appl Ergon 24:212–220. https://doi.org/10.1016/0003-6870(93)90009-x
Wattanaprakornkul D, Cathers I, Halaki M, Ginn KA (2011) The rotator cuff muscles have a direction specific recruitment pattern during shoulder flexion and extension exercises. J Sci Med Sport 14:376–382. https://doi.org/10.1016/j.jsams.2011.01.001
Funding
The authors do not have any financial. This research did not receive any grant support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the IRB of the MEDS clinic (Santiago, Chile) and the CEC of SS.OO. (Santiago, Chile) with reference number #16122016.
Informed consent
All participants gave their written informed consent to be enrolled in this study.
Consent for publication
All authors declare that they have contributed significantly to this manuscript. Also, the authors authorized this manuscript to be published.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Torres, J., Droppelmann, G., Silvestre, R. et al. Supraspinatus activation precedes the infraspinatus muscle during the shoulder abduction in different levels of handgrip strengths. Sport Sci Health 18, 915–921 (2022). https://doi.org/10.1007/s11332-021-00875-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11332-021-00875-z