Abstract
Purpose
To investigate the role and underlying mechanism of GDF11 on diabetic nephropathy (DN)-related mitochondrial dysfunction and apoptosis.
Methods
A DN model of rats was established in this study. Human Kidney-2 (HK-2) cells were cultured under high-glucose (HG) condition with or without recombinant GDF11 (rGDF11). Mitochondrial morphology of HK-2 cells was analyzed by transmission electron microscope and MitoTracker Red CMXRos staining. Mitochondrial membrane potential (MMP) and ROS production were monitored using JC-1 assay kit and MitoSOX staining, respectively. Cell apoptosis was detected by TUNEL or flow cytometry assays.
Results
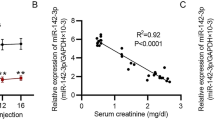
Herein, we observed that GDF11 was down-regulated in renal cortex and serum of DN rats, which was accompanied by renal mitochondrial morphological abnormalities. In line with the findings in vivo, HK-2 cells exposed to HG presented with mitochondrial morphological alterations and further apoptosis accompanied by GDF11 reduction. In addition, HG promoted a decrease in MMP while an increase in mitochondrial ROS production. Conversely, rGDF11 treatment significantly alleviated these HG-induced mitochondrial defects in HK-2 cells. Meanwhile, HK-2 cell apoptosis induced by HG was simultaneously suppressed by rGDF11. Mechanistically, the decreased levels of p-AKT induced by HG were attenuated after rGDF11 administration. Inhibition of the PI3K/AKT pathway resisted the effects of rGDF11 on the MMP and apoptosis of HK-2 cells. In addition, we identified that GDF11 is a target of miR-32-5p. Up-regulation of miR-32-5p could inhibit the expression of GDF11.
Conclusion
rGDF11 treatment rescued HG-induced HK-2 cell mitochondrial dysfunction and apoptosis, which may be dependent on the activation of the PI3K/AKT pathway.





Similar content being viewed by others
Data availability
All data generated or used during the study appear in the submitted article.
References
Anders HJ, Huber TB, Isermann B, Schiffer M (2018) CKD in diabetes: diabetic kidney disease versus nondiabetic kidney disease. Nat Rev Nephrol 14:361–377. https://doi.org/10.1038/s41581-018-0001-y
Barkoudah E, Skali H, Uno H, Solomon SD, Pfeffer MA (2012) Mortality rates in trials of subjects with type 2 diabetes. J Am Heart Assoc 1:8–15. https://doi.org/10.1161/jaha.111.000059
Pagliarini DJ, Calvo SE, Chang B et al (2008) A mitochondrial protein compendium elucidates complex I disease biology. Cell 134:112–123. https://doi.org/10.1016/j.cell.2008.06.016
Soltoff SP (1986) ATP and the regulation of renal cell function. Annu Rev Physiol 48:9–31. https://doi.org/10.1146/annurev.ph.48.030186.000301
Forbes JM, Thorburn DR (2018) Mitochondrial dysfunction in diabetic kidney disease. Nat Rev Nephrol 14:291–312. https://doi.org/10.1038/nrneph.2018.9
Bhargava P, Schnellmann RG (2017) Mitochondrial energetics in the kidney. Nat Rev Nephrol 13:629–646. https://doi.org/10.1038/nrneph.2017.107
Nakashima M, Toyono T, Akamine A, Joyner A (1999) Expression of growth/differentiation factor 11, a new member of the BMP/TGFbeta superfamily during mouse embryogenesis. Mech Dev 80:185–189. https://doi.org/10.1016/s0925-4773(98)00205-6
Simoni-Nieves A, Gerardo-Ramírez M, Pedraza-Vázquez G et al (2019) GDF11 Implications in Cancer Biology and Metabolism. Fact Contro Frontier oncol 9:1039. https://doi.org/10.3389/fonc.2019.01039
Rochette L, Malka G (2019) Neuroprotective potential of GDF11: myth or reality? Inter j mol sci. https://doi.org/10.3390/ijms20143563
Jamaiyar A, Wan W, Janota DM, Enrick MK, Chilian WM, Yin L (2017) The versatility and paradox of GDF 11. Pharmacol Ther 175:28–34. https://doi.org/10.1016/j.pharmthera.2017.02.032
Zhang Y, Li Q, Liu D et al (2016) GDF11 improves tubular regeneration after acute kidney injury in elderly mice. Sci Rep 6:34624. https://doi.org/10.1038/srep34624
Pons M, Koniaris LG, Moe SM, Gutierrez JC, Esquela-Kerscher A, Zimmers TA (2018) GDF11 induces kidney fibrosis, renal cell epithelial-to-mesenchymal transition, and kidney dysfunction and failure. Surgery 164:262–273. https://doi.org/10.1016/j.surg.2018.03.008
Zhang J, Li Y, Li H et al (2018) gdf11 improves angiogenic function of EPCs in diabetic limb ischemia. Diabetes 67:2084–2095. https://doi.org/10.2337/db17-1583
Lu B, Zhong J, Pan J et al (2019) Gdf11 gene transfer prevents high fat diet-induced obesity and improves metabolic homeostasis in obese and STZ-induced diabetic mice. J Transl Med 17:422. https://doi.org/10.1186/s12967-019-02166-1
Walker RG, Barrandon O, Poggioli T et al (2020) Exogenous GDF11, but not GDF8, reduces body weight and improves glucose homeostasis in mice. Sci Rep 10:4561. https://doi.org/10.1038/s41598-020-61443-y
Katsimpardi L, Kuperwasser N, Camus C et al (2020) Systemic GDF11 stimulates the secretion of adiponectin and induces a calorie restriction-like phenotype in aged mice. Aging Cell 19:e13038
Wang HJ, Liu H, Lin YH, Zhang SJ (2021) MiR-32-5p knockdown inhibits epithelial to mesenchymal transition and renal fibrosis by targeting SMAD7 in diabetic nephropathy. Hum Exp Toxicol 40:587–595. https://doi.org/10.1177/0960327120952157
Li XY, Wang SS, Han Z et al (2017) Triptolide restores autophagy to alleviate diabetic renal fibrosis through the miR-141-3p/PTEN/Akt/mTOR pathway. Mol therapy Nuc acid 9:48–56. https://doi.org/10.1016/j.omtn.2017.08.011
Jiang XS, **ang XY, Chen XM et al (2020) Inhibition of soluble epoxide hydrolase attenuates renal tubular mitochondrial dysfunction and ER stress by restoring autophagic flux in diabetic nephropathy. Cell Death Dis 11:385. https://doi.org/10.1038/s41419-020-2594-x
Uhlén M, Fagerberg L, Hallström BM et al (2015) Proteomics tissue-based map of the human proteome. Science 347:1260419
Thoudam T, Jeon JH, Ha CM, Lee IK (2016) Role of Mitochondria-associated endoplasmic reticulum membrane in inflammation-mediated metabolic diseases. Mediators Inflamm 2016:1851420. https://doi.org/10.1155/2016/1851420
Higgins GC, Coughlan MT (2014) Mitochondrial dysfunction and mitophagy: the beginning and end to diabetic nephropathy? Br J Pharmacol 171:1917–1942. https://doi.org/10.1111/bph.12503
Abe Y, Sakairi T, Kajiyama H, Shrivastav S, Beeson C, Kopp JB (2010) Bioenergetic characterization of mouse podocytes. Am J Physiol Cell Physiol 299:C464-476. https://doi.org/10.1152/ajpcell.00563.2009
Yuan Y, Huang S, Wang W et al (2012) Activation of peroxisome proliferator-activated receptor-γ coactivator 1α ameliorates mitochondrial dysfunction and protects podocytes from aldosterone-induced injury. Kidney Int 82:771–789. https://doi.org/10.1038/ki.2012.188
Fan Y, Yang Q, Yang Y et al (2019) Sirt6 suppresses high glucose-induced mitochondrial dysfunction and apoptosis in podocytes through AMPK activation. Int J Biol Sci 15:701–713. https://doi.org/10.7150/ijbs.29323
Garrido-Moreno V, Díaz-Vegas A, López-Crisosto C et al (2019) GDF-11 prevents cardiomyocyte hypertrophy by maintaining the sarcoplasmic reticulum-mitochondria communication. Pharmacol res 146:104273
Anqi X, Ruiqi C, Yanming R, Chao Y (2019) Neuroprotective potential of GDF11 in experimental intracerebral hemorrhage in elderly rats. J clinical neurosci 63:182–188. https://doi.org/10.1016/j.jocn.2019.02.016
Coughlan MT, Higgins GC, Nguyen TV et al (2016) Deficiency in apoptosis-inducing factor recapitulates chronic kidney disease via aberrant mitochondrial homeostasis. Diabetes 65:1085–1098. https://doi.org/10.2337/db15-0864
Coughlan MT, Nguyen TV, Penfold SA et al (2016) Map** time-course mitochondrial adaptations in the kidney in experimental diabetes. Clin sci 130:711–720
Liesa M, Shirihai OS (2013) Mitochondrial dynamics in the regulation of nutrient utilization and energy expenditure. Cell Metab 17:491–506. https://doi.org/10.1016/j.cmet.2013.03.002
**ao A, Zhang Y, Ren Y et al (2021) GDF11 alleviates secondary brain injury after intracerebral hemorrhage via attenuating mitochondrial dynamic abnormality and dysfunction. Sci Rep 11:3974. https://doi.org/10.1038/s41598-021-83545-x
Li H, Li Y, **ang L et al (2017) GDF11 attenuates development of type 2 diabetes via improvement of Islet β-Cell function and survival. Diabetes 66:1914–1927. https://doi.org/10.2337/db17-0086
Fresno Vara JA, Casado E, de Castro J, Cejas P, Belda-Iniesta C, González-Barón M (2004) PI3K/Akt signalling pathway and cancer. Cancer Treat Rev 30:193–204. https://doi.org/10.1016/j.ctrv.2003.07.007
Jafari M, Ghadami E, Dadkhah T, Akhavan-Niaki H (2019) PI3k/AKT signaling pathway: erythropoiesis and beyond. J Cell Physiol 234:2373–2385. https://doi.org/10.1002/jcp.27262
Pfeffer CM, Singh ATK (2018) Apoptosis: a target for anticancer therapy. Inter j mol sci. https://doi.org/10.3390/ijms19020448
Gao X, Li X, Ho CT et al (2020) Cocoa tea (Camellia ptilophylla) induces mitochondria-dependent apoptosis in HCT116 cells via ROS generation and PI3K/Akt signaling pathway. Food res inter. 129:108854
Wang L, Ma G, Zhang Y et al (2018) Effect of mitochondrial cytochrome c release and its redox state on the mitochondrial-dependent apoptotic cascade reaction and tenderization of yak meat during postmortem aging. Food res inter 111:488–497. https://doi.org/10.1016/j.foodres.2018.05.049
Wang W, Hao Y, Li F (2019) Notoginsenoside R1 alleviates high glucose-evoked damage in RSC96 cells through down-regulation of miR-503. Art cells 47:3947–3954. https://doi.org/10.1080/21691401.2019.1671434
Huang D, Peng Y, Ma K et al (2020) Puerarin relieved compression-induced apoptosis and mitochondrial dysfunction in human nucleus pulposus mesenchymal stem cells via the PI3K/Akt pathway. Stem cells inter 2020:7126914. https://doi.org/10.1155/2020/7126914
Acknowledgements
This work was supported by the Natural Science Foundation of Heilongjiang Province (Grant No. LH2020H064)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare no conflict of interest.
Ethical approval
This study was approved by the Experimental Animal Ethics Committee of The Fourth Affiliated Hospital of Harbin Medical University. We have read the journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
11255_2023_3495_MOESM1_ESM.tif
Supplementary file1 Fig. S1 (A) Quantification of MitoTracker Red CMXRos staining in Fig. 2F: the ratio of HK-2 cells with fragmented mitochondria. (B-C) Quantification of JC-1 (shown in Fig. 2G) and Mito SOX staining (shown in Fig. 2H), respectively (TIF 387 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, H., Zhang, Y., Liu, H. et al. GDF11, a target of miR-32-5p, suppresses high-glucose-induced mitochondrial dysfunction and apoptosis in HK-2 cells through PI3K/AKT signaling activation. Int Urol Nephrol 55, 1767–1778 (2023). https://doi.org/10.1007/s11255-023-03495-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03495-3