Abstract
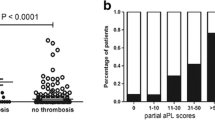
The adjusted global antiphospholipid syndrome score (aGAPSS) is a recently developed thrombotic risk assessment score that considers the antiphospholipid antibody (aPL) profile and conventional cardiovascular risk factors. In this retrospective study, we aimed to evaluate the validity of the aGAPSS in predicting clinical manifestations (criteria and extra-criteria) of antiphospholipid syndrome (APS) in a single centre cohort of patients. Ninety-eight patients with APS ± systemic lupus erythematosus (SLE) were classified according to clinical manifestations as vascular thrombosis (VT), pregnancy morbidity (PM) or both (VT + PM). The aGAPSS was calculated for each patient as previously defined. Mean aGAPSS of the cohort was calculated as 10.2 ± 3.8. Significantly higher aGAPSS values were seen in VT (n = 58) and VT + PM (n = 29) groups when compared to PM (n = 11) group (10.6 ± 3.7 vs 7.4 ± 2.9, P = 0.005; 10.7 ± 4 vs 7.4 ± 2.9, P = 0.008, respectively), mainly due to lower frequencies of cardiovascular risk factors in PM. Higher aGAPPS values were also associated with recurrent thrombosis (11.6 ± 3.7 vs 9.9 ± 3.6, P = 0.04). Regarding extra-criteria manifestations, patients with livedo reticularis (n = 11) and APS nephropathy (n = 9) had significantly higher aGAPSS values (12.9 ± 3.4 vs 9.9 ± 3.7, P = 0.02; 12.4 ± 2.9 vs 10 ± 3.8, P = 0.04, respectively). The computed AUC demonstrated that aGAPSS values ≥10 had the best diagnostic accuracy for thrombosis. Our results suggest that patients with higher aGAPSS values are at higher risk for develo** vascular thrombosis (either first event or recurrence) and extra-criteria manifestations, especially livedo reticularis and APS nephropathy.



Similar content being viewed by others
References
Miyakis S, Lockshin MD, Atsumi T et al (2006) International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost 4:295–306. https://doi.org/10.1111/j.1538-7836.2006.01753.x
Petri M, Orbai AM, Alarcon GS et al (2012) Derivation and validation of the systemic lupus international collaborating clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum 64:2677–2686. https://doi.org/10.1002/art.34473
Willis R, Pierangeli SS (2011) Pathophysiology of the antiphospholipid antibody syndrome. Auto Immun Highlights 2(2):35–52. https://doi.org/10.1007/s13317-011-0017-9
Galli M, Luciani D, Bertolini G, Barbui T (2003) Lupus anticoagulants are stronger risk factors for thrombosis than anticardiolipin antibodies in the antiphospholipid syndrome: a systematic review of the literature. Blood 101:1827–1832. https://doi.org/10.1182/blood-2002-02-0441
Ruffatti A, Del Ross T, Ciprian M et al (2011) Risk factors for a first thrombotic event in antiphospholipid antibody carriers: a prospective multicentre follow-up study. Ann Rheum Dis 70(6):1083–1086. https://doi.org/10.1136/ard.2010.142042
Reynaud Q, Lega J-C, Mismetti P, Chapelle C, Wahl D, Cathébras P, Laporte S (2014) Risk of venous and arterial thrombosis according to type of antiphospholipid antibodies in adults without systemic lupus erythematosus: a systematic review and meta-analysis. Autoimmun Rev 13:595–608. https://doi.org/10.1016/j.autrev.2013.11.004
Pengo V, Biasiolo A, Pegoraro C, Cucchini U, Noventa F, Iliceto S (2005) Antibody profiles for the diagnosis of antiphospholipid syndrome. Thromb Haemost 93(6):1147–1152. https://doi.org/10.1160/TH04-12-0839
Pericleous C, Rahman A (2014) Domain I: the hidden face of antiphospholipid syndrome. Lupus 23(12):1320–1323. https://doi.org/10.1177/0961203314540354
Sciascia S, Sanna G, Murru V, Roccatello D, Khamashta MA, Bertolaccini ML (2014) Anti-prothrombin (aPT) and anti-phosphatidylserine/prothrombin (aPS/PT) antibodies and the risk of thrombosis in the antiphospholipid syndrome. A systematic review. Thromb Haemost 111(2):354–364. https://doi.org/10.1160/TH13-06-0509
Cervera R, Serrano R, Pons-Estel GJ, on behalf of the Euro-Phospholipid Project Group (European Forum on Antiphospholipid Antibodies) et al (2015) Morbidity and mortality in the antiphospholipid syndrome during a 10-year period: a multicentre prospective study of 1000 patients. Ann Rheum Dis 74:1011–1018. https://doi.org/10.1136/annrheumdis-2013-204838
Artim-Esen B, Çene E, Şahinkaya Y, Ertan S, Pehlivan Ö, Kamali S, Gül A, Öcal L, Aral O, Inanç M (2014) Cluster analysis of autoantibodies in 852 patients with systemic lupus erythematosus from a single center. J Rheumatol 41(7):1304–1310. https://doi.org/10.3899/jrheum.130984
Miller CC, Reardon MJ, Safi HJ (2001) Risk stratification: a practical guide for clinicians. Cambridge University Press, Cambridge
Otomo K, Atsumi T, Amengual O, Fujieda Y, Kato M, Oku K, Horita T, Yasuda S, Koike T (2012) Efficacy of the antiphospholipid score for the diagnosis of antiphospholipid syndrome and its predictive value for thrombotic events. Arthritis Rheum 64:504–512. https://doi.org/10.1002/art.33340
Sciascia S, Sanna G, Murru V, Roccatello D, Khamashta MA, Bertolaccini ML (2013) GAPSS: the global anti-phospholipid syndrome score. Rheumatology (Oxford) 52:1397–1403. https://doi.org/10.1093/rheumatology/kes388
Sciascia S, Sanna G, Murru V, Roccatello D, Khamashta MA, Bertolaccini ML (2015) The global anti-phospholipid syndrome score in primary APS. Rheumatology (Oxford) 54:134–138. https://doi.org/10.1093/rheumatology/keu307
Oku K, Amengual O, Bohgaki T, Horita T, Yasuda S, Atsumi T (2015) An independent validation of the global anti-phospholipid syndrome score in a Japanese cohort of patients with autoimmune diseases. Lupus 24:774–775. https://doi.org/10.1177/0961203314561284
Fernandez Mosteirin N, Saez Comet L, Salvador Osuna C, Calvo Villas JM, Velilla Marco J (2017) Independent validation of the adjusted GAPSS: role of thrombotic risk assessment in the real-life setting. Lupus 26:1328–1332. https://doi.org/10.1177/0961203317703493
Radin M, Ugolini-Lopes MR, Sciascia S, Andrade D (2018) Extra-criteria manifestations of antiphospholipid syndrome: risk assessment and management. Semin Arthritis Rheum 48(1):117–120. https://doi.org/10.1016/j.semarthrit.2017.12.006
Kwaan HC, Samama M (2019) Clinical thrombosis. CRC Press
Karande GY, Hedgire SS, Sanchez Y (2017) Advanced imaging in acute and chronic deep vein thrombosis. Cardiovasc Diagn Ther 6(6):493–507. https://doi.org/10.21037/cdt.2016.12.06
Williams B, Mancia G, Spiering W, ESC Scientific Document Group et al (2018) 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J 39(33):3021–3104. https://doi.org/10.1093/eurheartj/ehy339
Grundy SM, Stone NJ, Bailey AL et al (2019) 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol 73(24):3168–3209. https://doi.org/10.1016/j.jacc.2018.11.002
American Diabetes Association (2020) 2. Classification and diagnosis of diabetes: standards of medical Care in Diabetes-2020. Diabetes Care 43(Suppl 1):S14–S31. https://doi.org/10.2337/dc20-S002
Pengo V (2012) ISTH guidelines on lupus anticoagulant testing. Thromb Res 130(Suppl 1):S76–S77. https://doi.org/10.1016/j.thromres.2012.08.283
Ruopp MD, Perkins NJ, Whitcomb BW, Schisterman EF (2008) Youden index and optimal cut-point estimated from observations affected by a lower limit of detection. Biom J 50(3):419–430. https://doi.org/10.1002/bimj.200710415
Habibzadeh F, Habibzadeh P, Yadollahie M (2016) On determining the most appropriate test cut-off value: the case of tests with continuous results. Biochem Med (Zagreb) 26(3):297–307. https://doi.org/10.11613/BM.2016.034
Ruffatti A, Del Ross T, Ciprian M et al (2009) Risk factors for a first thrombotic event in antiphospholipid antibody carriers. A multicentre, retrospective follow-up study. Ann Rheum Dis 68:397–399. https://doi.org/10.1136/ard.2008.096669
Sciascia S, Cosseddu D, Montaruli B, Kuzenko A, Bertero MT (2011) Risk scale for the diagnosis of antiphospholipid syndrome. Ann Rheum Dis 70:1517–1518. https://doi.org/10.1136/ard.2010.145177
Sciascia S, Cuadrado MJ, Sanna G, Murru V, Roccatello D, Khamashta MA, Bertolaccini ML (2014) Thrombotic risk assessment in systemic lupus erythematosus: validation of the global antiphospholipid syndrome score in a prospective cohort. Arthritis Care Res 66(12):1915–1920. https://doi.org/10.1002/acr.22388
Zuily S, de Laat B, Mohamed S, TAC(I)T investigators et al (2015) Validity of the global anti-phospholipid syndrome score to predict thrombosis: a prospective multicentre cohort study. Rheumatology (Oxford) 54(11):2071–2075. https://doi.org/10.1093/rheumatology/kev238
Sciascia S, Radin M, Sanna G, Cecchi I, Roccatello D, Bertolaccini ML (2018) Clinical utility of the global anti-phospholipid syndrome score (GAPSS) for risk stratification: a pooled analysis. Rheumatology (Oxford) 57(4):661–665. https://doi.org/10.1093/rheumatology/kex466
Radin M, Sciascia S, Erkan D, APS ACTION et al (2019) The adjusted global antiphospholipid syndrome score (aGAPSS) and the risk of recurrent thrombosis: results from the APS ACTION cohort. Semin Arthritis Rheum 49(3):464–468. https://doi.org/10.1016/j.semarthrit.2019.04.009
Radin M, Schreiber K, Costanzo P, Cecchi I, Roccatello D, Baldovino S, Bazzan M, Cuadrado MJ, Sciascia S (2017) The adjusted global antiphospholipid syndrome score (aGAPSS) for risk stratification in young APS patients with acute myocardial infarction. Int J Cardiol 240:72–77. https://doi.org/10.1016/j.ijcard.2017.02.155
Radin M, Schreiber K, Cecchi I, Roccatello D, Cuadrado MJ, Sciascia S (2018) The risk of ischaemic stroke in primary APS patients: a prospective study. Eur J Neurol 25(2):320–325. https://doi.org/10.1111/ene.13499
Bettiol A, Emmi G, Finocchi M et al (2020) Obstetric antiphospholipid syndrome is not associated with an increased risk of subclinical atherosclerosis. Rheumatology (Oxford). https://doi.org/10.1093/rheumatology/keaa116
Veerasamy M, Bagnall A, Neely D, Allen J, Sinclair H, Kunadian V (2015) Endothelial dysfunction and coronary artery disease: a state of the art review. Cardiol Rev 23(3):119–129. https://doi.org/10.1097/CRD.0000000000000047
Libby P, Pasterkamp G, Crea F, Jang IK (2019) Reassessing the mechanisms of acute coronary syndromes. Circ Res 124(1):150–160. https://doi.org/10.1161/CIRCRESAHA.118.311098
Mineo C (2013) Inhibition of nitric oxide and antiphospholipid antibody-mediated thrombosis. Curr Rheumatol Rep 15(5):324. https://doi.org/10.1007/s11926-013-0324-4
Jara LJ, Medina G, Vera-Lastra O, Amigo MC (2006) Accelerated atherosclerosis, immune response and autoimmune rheumatic diseases. Autoimmun Rev 5(3):195–201. https://doi.org/10.1016/j.autrev.2005.06.005
Hollan I, Meroni PL, Ahearn JM et al (2013) Cardiovascular disease in autoimmune rheumatic diseases. Autoimmun Rev 12(10):1004–1015. https://doi.org/10.1016/j.autrev.2013.03.013
Bilora F, Boccioletti V, Girolami B, Zanon E, Armani M, Petrobelli F, Girolami A (2002) Are antiphospholipid antibodies an independent risk factor for atherosclerosis? Clin Appl Thromb Hemost 8(2):103–113. https://doi.org/10.1177/107602960200800205
Matsuura E, Hughes GR, Khamashta MA (2008) Oxidation of LDL and its clinical implication. Autoimmun Rev 7(7):558–566. https://doi.org/10.1016/j.autrev.2008.04.018
Matsuura E, Kobayashi K, Inoue K, Lopez LR, Shoenfeld Y (2005) Oxidized LDL/beta2-glycoprotein I complexes: new aspects in atherosclerosis. Lupus 14(9):736–741. https://doi.org/10.1191/0961203305lu2211oa
Andrade D, Bortolotto L, Bonfá E, Borba E (2016) Primary antiphospholipid syndrome: absence of premature atherosclerosis in patients without traditional coronary artery disease risk factors. Lupus 25(5):472–478. https://doi.org/10.1177/0961203315617841
Funding
No funding to declare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors do not have any conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Uludağ, Ö., Bektaş, M., Çene, E. et al. Validation of the adjusted global antiphospholipid syndrome score in a single centre cohort of APS patients from Turkey. J Thromb Thrombolysis 51, 466–474 (2021). https://doi.org/10.1007/s11239-020-02195-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-020-02195-4