Abstract
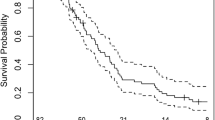
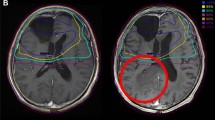
This study was designed to investigate the impact of interim progression of disease (PD) during the surgery-to-radiotherapy interval (SRI) and its predictors in glioblastoma based on MRIs. A total of 222 patients were planned for radiotherapy (RT) and 166 of them were evaluable for the presence of interim PD by 2 separate MRIs. The size criteria from the updated Response Assessment in Neuro-Oncology criteria was adopted to determine interim PD. 32 (19.3%) patients experienced interim PD, and their median survival (MS) was shorter than patients without PD in univariate (11.3 vs. 19.6 months, p < 0.001) and multivariate analysis (HR 2.237, 95% CI 1.367–3.660, p = 0.002). The volume of residual enhancing tumor (p = 0.003) and prolongation of the SRI (p = 0.004) were significant predictors of interim PD. Every 1-cc increase in residual enhancing tumor and every 1-day prolongation of the SRI significantly increased the risk of interim PD by 3.9% (p = 0.003) and 8.1% (p = 0.004), respectively. A significant portion of patients demonstrate interim PD during SRI and these patients have poor prognosis. The presence of interim PD should be concerned as a significant confounding factor for stratification in future clinical trials. A baseline pre-RT MRI is essential for accurate disease evaluation and RT-target delineation, especially in patients with larger residual disease after surgery and prolonged SRI due to the high risk of interim PD.

Similar content being viewed by others
References
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Eng J Med 352:987–996
Rønning PA, Helseth E, Meling TR, Johannesen TB (2012) A population-based study on the effect of temozolomide in the treatment of glioblastoma multiforme. Neuro Oncol 14:1178–1184
Pennington C, Kilbride L, Grant R, Wardlaw JM (2006) A pilot study of brain tumour growth between radiotherapy planning and delivery. Clin Oncol (R Coll Radiol) 18:104–108
Pirzkall A, McGue C, Saraswathy S et al (2009) Tumor regrowth between surgery and initiation of adjuvant therapy in patients with newly diagnosed glioblastoma. Neuro Oncol 11:842–852
Stensjøen AL, Solheim O, Kvistad KA, Håberg AK, Salvesen Ø, Berntsen EM (2015) Growth dynamics of untreated glioblastomas in vivo. Neuro Oncol 17:1402–1411
Ellingson BM, Nguyen HN, Lai A et al (2016) Contrast-enhancing tumor growth dynamics of preoperative, treatment-naive human glioblastoma. Cancer 122:1718–1727
Gilbert MR, Wang M, Aldape KD et al (2013) Dose-dense temozolomide for newly diagnosed glioblastoma: a randomized phase III clinical trial. J Clin Oncol 31:4085–4091
Gilbert MR, Dignam JJ, Armstrong TS et al (2014) A randomized trial of bevacizumab for newly diagnosed glioblastoma. N Engl J Med 370:699–708
Niyazi M, Brada M, Chalmers AJ et al (2016) ESTRO-ACROP guideline ‘‘target delineation of glioblastomas”. Radiother Oncol 118:35–42
Merkel A, Soeldner D, Wendl C et al (2017) Early postoperative tumor progression predicts clinical outcome in glioblastoma-implication for clinical trials. J Neurooncol 132:249–254
Osborn AG (2012) Osborn’s brain: imaging, pathology, and anatomy, 1st edn. Amirsys, Inc, Salt Lake City
Mehrara E, Forssell-Aronsson E, Ahlman H, Bernhardt P (2007) Specific growth rate versus doubling time for quantitative characterization of tumor growth rate. Cancer Res 67:3970–3975
Wen PY, Macdonald DR, Reardon DA et al (2010) Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol 28:1963–1972
Bette S, Gempt J, Huber T et al (2016) Patterns and time dependence of unspecific enhancement in postoperative magnetic resonance imaging after glioblastoma resection. World Neurosurg 90:440–447
Kreth FW, Thon N, Simon M et al (2013) Gross total but not incomplete resection of glioblastoma prolongs survival in the era of radiochemotherapy. Ann Oncol 24:3117–3123
Huang J, Barbera L, Brouwers M, Browman G, Mackillop WJ (2003) Does delay in starting treatment affect the outcomes of radiotherapy? A systematic review. J Clin Oncol 21:555–563
Sun MZ, Oh T, Ivan ME et al (2015) Survival impact of time to initiation of chemoradiotherapy after resection of newly diagnosed glioblastoma. J Neurosurg 122:1144–1150
Loureiro LV, Victor Eda S, Callegaro-Filho D et al (2016) Minimizing the uncertainties regarding the effects of delaying radiotherapy for Glioblastoma: a systematic review and meta-analysis. Radiother Oncol 118:1–8
Louvel G, Metellus P, Noel G et al (2016) Delaying standard combined chemoradiotherapy after surgical resection does not impact survival in newly diagnosed glioblastoma patients. Radiother Oncol 118:9–15
Funding
This work was supported by the National R&D Program for Cancer Control by National Cancer Center Korea [Grant No. 1320220] and the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIP) [Grant No. 2013M2A2A7043683] to Il Han Kim.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that we have no conflict of interest.
Ethical approval
This study was performed with the approval of the Health Institutional Review Board of Seoul National University Hospital, Seoul, Korea (IRB No. H-1507-138-690). For this type of study formal consent is not required. The current article also does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Wee, C.W., Kim, E., Kim, T.M. et al. Impact of interim progression during the surgery-to-radiotherapy interval and its predictors in glioblastoma treated with temozolomide-based radiochemotherapy. J Neurooncol 134, 169–175 (2017). https://doi.org/10.1007/s11060-017-2505-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-017-2505-x