Abstract
Objective
To determine factors associated with a positive male patient experience (PMPE) at fertility clinics among male patients.
Design: Cross-sectional study
Setting: Not applicable
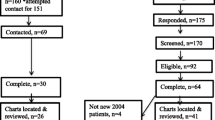
Patients: Male respondents to the FertilityIQ questionnaire (www.fertilityiq.com) reviewing the first or only US clinic visited between June 2015 and August 2020.
Interventions: None
Main outcome measures: PMPE was defined as a score of 9 or 10 out of 10 to the question, “Would you recommend this fertility clinic to a best friend?”. Examined predictors included demographics, payment details, infertility diagnoses, treatment, and outcomes, physician traits, and clinic operations and resources. Multiple imputation was used for missing variables and logistic regression was used to calculate adjusted odds ratios (aORs) for factors associated with PMPE.
Results
Of the 657 men included, 60.9% reported a PMPE. Men who felt their doctor was trustworthy (aOR 5.01, 95% CI 0.97–25.93), set realistic expectations (aOR 2.73, 95% CI 1.10–6.80), and was responsive to setbacks (aOR 2.43, 95% CI 1.14–5.18) were more likely to report PMPE. Those who achieved pregnancy after treatment were more likely to report PMPE; however, this was no longer significant on multivariate analysis (aOR 1.30, 95% CI 0.68–2.47). Clinic-related factors, including ease of scheduling appointments (aOR 4.03, 95% CI 1.63–9.97) and availability of same-day appointments (aOR 4.93, 95% CI 1.75–13.86), were associated with PMPE on both univariate and multivariate analysis. LGBTQ respondents were more likely to report PMPE, whereas men with a college degree or higher were less likely to report PMPE; however, sexual orientation (aOR 3.09, 95% CI 0.86–11.06) and higher educational level (aOR 0.54, 95% CI 0.30–1.10) were not associated with PMPE on multivariate analysis.
Conclusion
Physician characteristics and clinic characteristics indicative of well-run administration were the most highly predictive of PMPE. By identifying factors that are associated with a PMPE, clinics may be able to optimize the patient experience and improve the quality of infertility care that they provide for both men and women.
Similar content being viewed by others
References
Mehta A, Nangia A, Dupree J, Smith J. Limitations and barriers in access to care for male factor infertility. Fertil Steril. 2016;105(5):1128–37.
Smith J, Walsh T, Shindel A, et al. Sexual, marital, and social impact of a man's perceived infertility diagnosis. J Sex Med. 2009;6(9):2505–15.
Hammarberg K, Baker H, Fisher J. Men's experiences of infertility and infertility treatment 5 years after diagnosis of male factor infertility: a retrospective cohort study. Hum Reprod. 2010;25(11):2815–20.
Petok W. Infertility counseling (or the lack thereof) of the forgotten male partner. Fertil Steril. 2015;104(2):260–6.
Mehta A. Qualitative research in male infertility. Urol Clin North Am. 2020;47(2):205–10.
Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3:1.
Dancet E, Nelen W, Sermeus W, Leeuw LD, Kremer J, D'Hooghe T. The patients' perspective on fertility care: a systematic review. Hum Reprod Update. 2010;16(5):467–87.
Lass A, Brinsden P. How do patients choose private in vitro fertilization treatment? A customer survey in a tertiary fertility center in the United Kingdom. Fertil Steril. 2001;75(5):893–7.
Malin M, Hemmink E, Räikkönen O, Sivho S, Perala M. What do women want? Women's experiences of infertility treatment. Soc Sci Med. 2001;53(1):123–33.
Shandley L, Hipp H, Anderson-Bialis J, Boulet S, McKenzie L, Kawass J. Patient-centered care: factors associated with reporting a positive experience at United States fertility clinics. Assisted Reprod. 2020;113(4):797–810.
Okunrintemi V, Valero-Elizondo J, Patrick B, et al. Gender differences in patient-reported outcomes among adults with atherosclerotic cardiovascular disease. J Am Heart Assoc. 2018;7(24)
Otani K, Buchanan P, Desai S, Herrmann P. Different combining process between male and female patients to reach their overall satisfaction. J Patient Exp. 2016;3(4):145–50.
Bener A, Ghuloum S. Gender difference on patients' satisfaction and expectation towards mental health care. Niger J Clin Pract. 2013;16(3):285–91.
Chen P, Tolpadi A, Elliott M, et al. Gender differences in patients' experience of care in the emergency department. J Gen Intern Med. 2022;37(3):676–9.
Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol. 1993;138:923–36.
Weng H, Hsueh Y, Messam L, Hertz-Picciotto I. Methods of covariate selection: directed acyclic graphs and the change-in-estimate procedure. Am J Epidemiol. 2009;169:1182–90.
Mourad S, Nelen W, Akkermans R, et al. Determinants of patients' experiences and satisfaction with fertility care. Fertil Steril. 2010;94(4):1254–60.
Iv E, Nelen W, Tepe E, Ev L, Verhaak C, Kremer J. Weaknesses, strengths and needs in fertility care according to patients. Hum Reprod. 2010;25(1)
Batbaatar E, Dorjdagva J, Luvsannyam A, Savino M, Amenta P. Determinants of patient satisfaction: a systematic review. Perspect Public Health. 2017;137(2):89–101.
Fenton J, Jerant A, Bertakis K, Franks P. The cost of satisfaction: a national study of patient satisfaction, health care utilization, expenditures, and mortality. Arch Intern Med. 2012;172(5):405–11.
Carini E, Villani L, Pezzullo A, et al. The impact of digital patient portals on health outcomes, system efficiency, and patient attitudes: updated systematic literature review. J Med Internet Res. 2021;23(9)
Kinney A, Sankaranarayanan B. Effects of patient portal use on patient satisfaction: survey and partial least squares analysis. J Med Internet Res. 2021;23(8)
Jones J. LGBT Identification in U.S. Ticks Up to 7.1%. Gallup. https://news.gallup.com/poll/389792/lgbt-identification-ticks-up.aspx
Mulé N, Ross L, Deeprose B, et al. Promoting LGBT health and wellbeing through inclusive policy development. Int J Equity Health. 2009;8(18)
Colpitts E, Gahagan J. The utility of resilience as a conceptual framework for understanding and measuring LGBTQ health. Int J Equity Health. 2016;15(60)
Hudson K, Bruce-Miller V. Nonclinical best practices for creating LGBTQ-inclusive care environments: A sco** review of gray literature. J Gay Lesbian Soc Serv. 2022;35(2):218–40.
Leyser-Whalen O, Bombach B, Mahmoud S, Greil A. From generalist to specialist: a qualitative study of the perceptions of infertility patients. Reprod Biomed Soc Online. 2021;14:204–15.
Quintana J, González N, Bilbao A, et al. Predictors of patient satisfaction with hospital health care. BMC Health Serv Res. 2006;102(6)
Sylvest R, Fürbringer J, Schmidt L. Infertile men’s needs and assessment of fertility care. Ups J Med Sci. 2016;121(4):276–82.
Arya S, Dibb B. The experience of infertility treatment: the male perspective. Hum Fertil. 2016;19(4):242–8.
Iv E, Dancet E, Koolman K, et al. Physicians underestimate the importance of patient-centredness to patients: a discrete choice experiment in fertility care. Hum Reprod. 2011;26(3):584–93.
Zaake D, Kayiira A, Namagembe I. Perceptions, expectations and challenges among men during in vitro fertilization treatment in a low resource setting: a qualitative study. Fertil Res Pract. 2019;5(6)
Fisher J, Hammarberg K. Psychological and social aspects of infertility in men: an overview of the evidence and implications for psychologically informed clinical care and future research. Asian J Androl. 2012;14(1):121–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J.A.B. and D.A.B. have financial relationships with FertilityIQ, which served as the source of data for this article. The remaining authors declare no competing interests.
Attestation statement
• The subjects in this trial have not concomitantly been involved in other randomized trials.
• Data regarding any of the subjects in the study has not been previously published unless specified.
• Data will be made available to the editors of the journal for review or a query upon request.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Siddharth Marthi and Lisa M. Shandley shared the first authorship.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marthi, S., Shandley, L.M., Ismaeel, N. et al. Factors associated with a positive experience at US fertility clinics: the male partner perspective. J Assist Reprod Genet 40, 1317–1328 (2023). https://doi.org/10.1007/s10815-023-02848-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-023-02848-2