Abstract
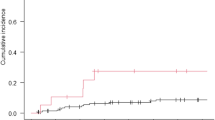
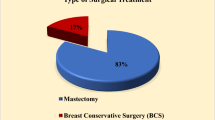
To compare the local control and brain radionecrosis in patients with brain metastasis primarily treated by single-fraction radiosurgery (SRS) or hypofractionated stereotactic radiotherapy (HFSRT). Between January 2012 and December 2017, 179 patients with only 1–3 brain metastases (total: 287) primarily treated by SRS (14 Gy) or HFSRT (23.1 Gy in 3 fractions of 7.7 Gy, every other day) were retrospectively analyzed in a single center. Follow-up imaging data were available in 152 patients with 246 lesions. The corresponding Biological Effective Dose (BED) were 33.6 Gy and 40.9 Gy respectively for SRS and HFSRT group, assuming an α/β of 10 Gy. Local control (LC) and risk of radionecrosis (RN) were calculated by the Kaplan–Meier method. The actuarial local control rates at 6 and 12 months were 94% and 88.1% in SRS group, and 87.6% and 78.4%, in HFSRT group (p = 0.06), respectively. Only the total volume of edema was associated with worse LC (p = 0.01, HR 1.02, 95% CI [1.004–1.03]) in multivariate analysis. Brain radionecrosis occurred in 1 lesion in SRS group and 9 in HFSRT group. Median time to necrosis was 5.5 months (range 1–9). Only the volume of GTV was associated with RN (p = 0.02, HR 1.09, 95% CI [1.01–1.18]) in multivariate analysis. Multi-fraction SRT dose of 23.31 Gy in 3 fractions has similar efficacy to single-fraction SRT dose of 14 Gy in patients with brain metastases. A slightly higher occurrence of radionecrosis appeared in HFSRT group.


Similar content being viewed by others
References
Soffietti R, Abacioglu U, Baumert B, Combs SE, Kinhult S, Kros JM et al (2017) Diagnosis and treatment of brain metastases from solid tumors: guidelines from the European Association of Neuro-Oncology (EANO). Neuro-Oncol févr 19(2):162–174
Auchter RM, Lamond JP, Alexander E, Buatti JM, Chappell R, Friedman WA et al (1996) A multiinstitutional outcome and prognostic factor analysis of radiosurgery for resectable single brain metastasis. Int J Radiat Oncol Biol Phys 35(1):27–35
Muacevic A, Wowra B, Siefert A, Tonn J-C, Steiger H-J, Kreth FW (2008) Microsurgery plus whole brain irradiation versus Gamma Knife surgery alone for treatment of single metastases to the brain: a randomized controlled multicentre phase III trial. J Neurooncol 87(3):299–307
Chang EL, Wefel JS, Hess KR, Allen PK, Lang FF, Kornguth DG et al (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10(11):1037–1044
Andrews DW, Scott CB, Sperduto PW, Flanders AE, Gaspar LE, Schell MC et al (2004) Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. The Lancet 363(9422):1665–1672
Kocher M, Soffietti R, Abacioglu U, Villà S, Fauchon F, Baumert BG et al (2011) Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952–26001 study. J Clin Oncol 29(2):134–141
Minniti G, D’Angelillo RM, Scaringi C, Trodella LE, Clarke E, Matteucci P et al (2014) Fractionated stereotactic radiosurgery for patients with brain metastases. J Neurooncol avr 117(2):295–301
Ernst-Stecken A, Ganslandt O, Lambrecht U, Sauer R, Grabenbauer G (2006) Phase II trial of hypofractionated stereotactic radiotherapy for brain metastases: results and toxicity. Radiother Oncol J Eur Soc Ther Radiol Oncol 81(1):18–24
Narayana A, Chang J, Yenice K, Chan K, Lymberis S, Brennan C et al (2007) Hypofractionated stereotactic radiotherapy using intensity-modulated radiotherapy in patients with one or two brain metastases. Stereotact Funct Neurosurg 85(2–3):82–87
Kwon AK, Dibiase SJ, Wang B, Hughes SL, Milcarek B, Zhu Y (2009) Hypofractionated stereotactic radiotherapy for the treatment of brain metastases. Cancer 115(4):890–898
Saitoh JI, Saito Y, Kazumoto T, Kudo S, Ichikawa A, Hayase N et al (2010) Therapeutic effect of linac-based stereotactic radiotherapy with a micro-multileaf collimator for the treatment of patients with brain metastases from lung cancer. Jpn J Clin Oncol 40(2):119–124
Rajakesari S, Arvold ND, Jimenez RB, Christianson LW, Horvath MC, Claus EB et al (2014) Local control after fractionated stereotactic radiation therapy for brain metastases. J Neurooncol 120(2):339–346
Higuchi Y, Serizawa T, Nagano O, Matsuda S, Ono J, Sato M et al (2009) Three-staged stereotactic radiotherapy without whole brain irradiation for large metastatic brain tumors. Int J Radiat Oncol Biol Phys 74(5):1543–1548
Lehrer EJ, Peterson JL, Zaorsky NG, Brown PD, Sahgal A, Chiang VL et al (2019) Single versus multifraction stereotactic radiosurgery for large brain metastases: an international meta-analysis of 24 trials. Int J Radiat Oncol Biol Phys 103(3):618–630
Kim Y-J, Cho KH, Kim J-Y, Lim YK, Min HS, Lee SH et al (2011) Single-dose versus fractionated stereotactic radiotherapy for brain metastases. Int J Radiat Oncol 81(2):483–489
Feuvret L, Vinchon S, Martin V, Lamproglou I, Halley A, Calugaru V et al (2014) Stereotactic radiotherapy for large solitary brain metastases. Cancer/Radiothérapie 18(2):97–106
Fokas E, Henzel M, Surber G, Kleinert G, Hamm K, Engenhart-Cabillic R (2012) Stereotactic radiosurgery and fractionated stereotactic radiotherapy: comparison of efficacy and toxicity in 260 patients with brain metastases. J Neurooncol 109(1):91–98
Minniti G, Scaringi C, Paolini S, Lanzetta G, Romano A, Cicone F et al (2016) Single-fraction versus multifraction (3 × 9 Gy) stereotactic radiosurgery for large (%3e 2 cm) brain metastases: a comparative analysis of local control and risk of radiation-induced brain necrosis. Int J Radiat Oncol 95(4):1142–1148
Ishihara T, Yamada K, Harada A, Isogai K, Tonosaki Y, Demizu Y et al (2016) Hypofractionated stereotactic radiotherapy for brain metastases from lung cancer: Evaluation of indications and predictors of local control. Strahlenther Onkol 192(6):386–393
Kirkpatrick JP, Soltys SG, Lo SS, Beal K, Shrieve DC, Brown PD (2017) The radiosurgery fractionation quandary: single fraction or hypofractionation? Neuro-Oncol 19(suppl_2):ii38–49
Shuryak I, Carlson DJ, Brown JM, Brenner DJ (2015) High-dose and fractionation effects in stereotactic radiation therapy: analysis of tumor control data from 2965 patients. Radiother Oncol 115(3):327–334
Wiggenraad R, Kanter AV, Kal HB, Taphoorn M, Vissers T, Struikmans H (2011) Dose–effect relation in stereotactic radiotherapy for brain metastases. A systematic review Radiother Oncol 98(3):292–297
Baliga S, Garg MK, Fox J, Kalnicki S, Lasala PA, Welch MR et al (2017) Fractionated stereotactic radiation therapy for brain metastases: a systematic review with tumour control probability modelling. Br J Radiol 90(1070):20160666
Rodrigues G, Warner A, Bauman G, Senan S, Lagerwaard F (2014) Systematic review of fractionated brain metastases radiotherapy. J Radiat Oncol 3(1):29–41
Matsuyama T, Kogo K, Oya N (2013) Clinical outcomes of biological effective dose-based fractionated stereotactic radiation therapy for metastatic brain tumors from non-small cell lung cancer. Int J Radiat Oncol Biol Phys 85(4):984–990
Kirkpatrick JP, Meyer JJ, Marks LB (2008) The linear-quadratic model is inappropriate to model high dose per fraction effects in radiosurgery. Semin Radiat Oncol 18(4):240–243
Brenner DJ (2008) The linear-quadratic model is an appropriate methodology for determining isoeffective doses at large doses per fraction. Semin Radiat Oncol 18(4):234–239
Brown JM, Carlson DJ, Brenner DJ (2014) The tumor radiobiology of SRS and SBRT: are more than the 5 R’s Involved? Int J Radiat Oncol Biol Phys 88(2):254–262
Song CW, Lee Y-J, Griffin RJ, Park I, Koonce NA, Hui S et al (2015) Indirect tumor cell death after high-dose hypofractionated irradiation: implications for stereotactic body radiation therapy and stereotactic radiation surgery. Int J Radiat Oncol Biol Phys 93(1):166–172
Pin Y, Antoni D, Keller A, Truntzer P, Clavier JB, Schaeffer O, et al. Clinical evaluation of a semi-automated contouring tool for edema surrounding brain metastasis: the Metabrain software. In submission [Internet]. 2018; Available on: https://github.com/yvanpin/Metabrain
Lucia F, Key S, Dissaux G, Goasduff G, Lucia A-S, Ollivier L et al (2019) Inhomogeneous tumor dose distribution provides better local control than homogeneous distribution in stereotactic radiotherapy for brain metastases. Radiother Oncol 130:132–138
Nataf F, Schlienger M, Liu Z, Foulquier JN, Grès B, Orthuon A et al (2008) Radiosurgery with or without A 2-mm margin for 93 single brain metastases. Int J Radiat Oncol Biol Phys 70(3):766–772
Noël G, Simon JM, Valery CA, Cornu P, Boisserie G, Hasboun D et al (2003) Radiosurgery for brain metastasis: impact of CTV on local control. Radiother Oncol 68(1):15–21
Kirkpatrick JP, Wang Z, Sampson JH, McSherry F, Herndon JE, Allen KJ et al (2015) Defining the optimal planning target volume in image-guided stereotactic radiosurgery of brain metastases: results of a randomized trial. Int J Radiat Oncol Biol Phys 91(1):100–108
Shaw E, Scott C, Souhami L, Dinapoli R, Kline R, Loeffler J et al (2000) Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: final report of RTOG protocol 90–05. Int J Radiat Oncol Biol Phys 47(2):291–298
Vogelbaum MA, Angelov L, Lee S-Y, Li L, Barnett GH, Suh JH (2006) Local control of brain metastases by stereotactic radiosurgery in relation to dose to the tumor margin. J Neurosurg 104(6):907–912
Chao ST, Barnett GH, Vogelbaum MA, Angelov L, Weil RJ, Neyman G et al (2008) Salvage stereotactic radiosurgery effectively treats recurrences from whole-brain radiation therapy. Cancer 113(8):2198–2204
Molenaar R, Wiggenraad R, Verbeek-de Kanter A, Walchenbach R, Vecht C (2009) Relationship between volume, dose and local control in stereotactic radiosurgery of brain metastasis. Br J Neurosurg 23(2):170–178
Schomas DA, Roeske JC, MacDonald RL, Sweeney PJ, Mehta N, Mundt AJ (2005) Predictors of tumor control in patients treated with linac-based stereotactic radiosurgery for metastatic disease to the brain. Am J Clin Oncol 28(2):180–187
Jiang X, **ao J, Zhang Y, Xu Y, Li X, Chen X et al (2012) Hypofractionated stereotactic radiotherapy for brain metastases larger than three centimeters. Radiat Oncol Lond Engl 7:36
Wegner R, Leeman J, Kabolizadeh P, Rwigema J-C, Mintz A, Burton S et al (2015) Fractionated stereotactic radiosurgery for large brain metastases. Am J Clin Oncol 38(2):135–139
Murai T, Ogino H, Manabe Y, Iwabuchi M, Okumura T, Matsushita Y et al (2014) Fractionated stereotactic radiotherapy using cyberKnife for the treatment of large brain metastases: a dose escalation study. Clin Oncol 26(3):151–158
Bilger A, Frenzel F, Oehlke O, Wiehle R, Milanovic D, Prokic V et al (2017) Local control and overall survival after frameless radiosurgery: a single center experience. Clin Transl Radiat Oncol 7:55–61
Tini P, Nardone V, Pastina P, Battaglia G, Vinciguerra C, Carfagno T et al (2017) Perilesional edema in brain metastasis from non-small cell lung cancer (NSCLC) as predictor of response to radiosurgery (SRS). Neurol Sci 38(6):975–982
Berghoff AS, Ilhan-Mutlu A, Wöhrer A, Hackl M, Widhalm G, Hainfellner JA et al (2014) Prognostic significance of Ki67 proliferation index, HIF1 alpha index and microvascular density in patients with non-small cell lung cancer brain metastases. Strahlenther Onkol Organ Dtsch Rontgengesellschaft Al 190(7):676–685
Spanberger T, Berghoff AS, Dinhof C, Ilhan-Mutlu A, Magerle M, Hutterer M et al (2013) Extent of peritumoral brain edema correlates with prognosis, tumoral growth pattern, HIF1a expression and angiogenic activity in patients with single brain metastases. Clin Exp Metastasis 30(4):357–368
Aoyama H, Shirato H, Onimaru R, Kagei K, Ikeda J, Ishii N et al (2003) Hypofractionated stereotactic radiotherapy alone without whole-brain irradiation for patients with solitary and oligo brain metastasis using noninvasive fixation of the skull. Int J Radiat Oncol Biol Phys 56(3):793–800
Blonigen BJ, Steinmetz RD, Levin L, Lamba MA, Warnick RE, Breneman JC (2010) Irradiated volume as a predictor of brain radionecrosis after linear accelerator stereotactic radiosurgery. Int J Radiat Oncol Biol Phys 77(4):996–1001
Navarria P, Clerici E, Carta G, Attuati L, Picozzi P, Franzese C et al (2018) Randomized phase III trial comparing gamma knife and linac based (EDGE) approaches for brain metastases radiosurgery: results from the gadget trial. Int J Radiat Oncol Biol Phys 102(3):S143–S144
Inoue HK, Seto K, Nozaki A, Torikai K, Suzuki Y, Saitoh J et al (2013) Three-fraction CyberKnife radiotherapy for brain metastases in critical areas: referring to the risk evaluating radiation necrosis and the surrounding brain volumes circumscribed with a single dose equivalence of 14 Gy (V14). J Radiat Res 54(4):727–735
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Loo, M., Pin, Y., Thierry, A. et al. Single-fraction radiosurgery versus fractionated stereotactic radiotherapy in patients with brain metastases: a comparative study. Clin Exp Metastasis 37, 425–434 (2020). https://doi.org/10.1007/s10585-020-10031-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-020-10031-5