Abstract
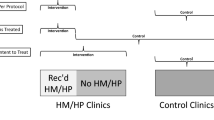
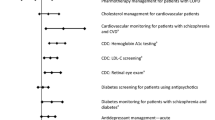
We examine the impact of mental health based primary care on physical health treatment among community mental health center patients in New York State using propensity score adjusted difference in difference models. Outcomes are quality indicators related to outpatient medical visits, diabetes HbA1c monitoring, and metabolic monitoring of antipsychotic treatment. Results suggest the program improved metabolic monitoring for patients on antipsychotics in one of two waves, but did not impact other quality indicators. Ceiling effects may have limited program impacts. More structured clinical programs to may be required to achieve improvements in quality of physical health care for this population.

Similar content being viewed by others
References
Alakeson, V., Frank, R. G., & Katz, R. E. (2010). Specialty care medical homes for people with severe, persistent mental disorders. Health Affairs, 29(5), 867–873.
American Diabetes Association, American Psychiatric Association, American Association of Clinical Endocrinologists, & North American Association for the Study of Obesity. (2004). Consensus development conference on antipsychotic drugs and obesity and diabetes. Diabetes Care, 27(2), 596–601.
Bao, Y., Casalino, L. P., & Pincus, H. A. (2013). Behavioral health and health care reform models: Patient-centered medical home, health home, and accountable care organization. The Journal of Behavioral Health Services & Research, 40(1), 121–132. doi:10.1007/s11414-012-9306-y.
Byrd, V. L., & Dodd, A. H. (2015). Assessing the usability of encounter data for enrollees in comprehensive managed care 2010–2011. https://www.cms.gov/Research-Statistics-Data-and-Systems/Computer-Data-and-Systems/MedicaidDataSourcesGenInfo/Downloads/MAX_Encounter_Brief_2010_2011.pdf.
Center for Mental Health Services. (2016). Primary and Behavioral Health Care Integration Grants (PBHCI). Retrieved from http://www.integration.samhsa.gov/about-us/PBHCI_Performance_Profile_2016.pdf.
Druss, B. G., Esenwein, S. A., Glick, G. E., Deubler, E., Lally, C., Ward, M. C., & Rask, K. J. (2016). Randomized trial of an integrated behavioral health home: The health outcomes management and evaluation (home) study. American Journal of Psychiatry. doi:10.1176/appi.ajp.2016.16050507.
Druss, B. G., Marcus, S. C., Campbell, J., Cuffel, B., Harnett, J., Ingoglia, C., & Mauer, B. (2008). Medical services for clients in community mental health centers: Results from a national survey. Psychiatric Services, 59(8), 917–920. doi:10.1176/ps.2008.59.8.917.
Druss, B. G., Rohrbaugh, R. M., Levinson, C. M., & Rosenheck, R. A. (2001). Integrated medical care for patients with serious psychiatric illness: A randomized trial. Archives of General Psychiatry, 58(9), 861–868.
Druss, B. G., von Esenwein, S. A., Compton, M. T., Rask, K. J., Zhao, L., & Parker, R. M. (2010). A randomized trial of medical care management for community mental health settings: The primary care access, referral, and evaluation (PCARE) study. American Journal of Psychiatry, 167(2), 151–159. doi:10.1176/appi.ajp.2009.09050691.
Druss, B. G., Zhao, L., Von Esenwein, S., Morrato, E. H., & Marcus, S. C. (2011). Understanding excess mortality in persons with mental illness 17-year follow up of a nationally representative US Survey. Medical Care, 49(6), 599–604. doi:10.1097/MLR.0b013e31820bf86e.
Funk, M. J., Westreich, D., Wiesen, C., Sturmer, T., Brookhart, M. A., & Davidian, M. (2011). Doubly robust estimation of causal effects. American Journal of Epidemiology, 173(7), 761–767. doi:10.1093/aje/kwq439.
Goldman, M. L., Spaeth-Rublee, B., & Pincus, H. (2015). Quality indicators for physical and behavioral health care integration. JAMA: The Journal of the American Medical Association, 314(8), 769–770. doi:10.1001/jama.2015.6447.
Harman, J. S., Scholle, S. H., Ng, J. H., Pawlson, L. G., Mardon, R. E., Haffer, S. C., …, Bierman, A. S. (2010). Association of health plans’ healthcare effectiveness data and information set (HEDIS) performance with outcomes of enrollees with diabetes. Medical Care, 48(3), 217–223. doi:10.1097/MLR.0b013e3181ca3fe6.
Horvitz-Lennon, M., Kilbourne, A. M., & Pincus, H. A. (2006). From silos to bridges: Meeting the general health care needs of adults with severe mental illnesses. Health Affairs, 25(3), 659–669.
Horvitz-Lennon, M., Volya, R., Donohue, J. M., Lave, J. R., Stein, B. D., & Normand, S. L. (2014). Disparities in quality of care among publicly insured adults with schizophrenia in four large U.S. states, 2002–2008. Health Services Research, 49(4), 1121–1144. doi:10.1111/1475-6773.12162.
Janssen, E. M., McGinty, E. E., Azrin, S. T., Juliano-Bult, D., & Daumit, G. L. (2015). Review of the evidence: Prevalence of medical conditions in the United States population with serious mental illness. General Hospital Psychiatry. doi:10.1016/j.genhosppsych.2015.03.004.
Kilbourne, A. M., Fullerton, C., Dausey, D., Pincus, H. A., & Hermann, R. C. (2010). A framework for measuring quality and promoting accountability across silos: The case of mental disorders and co-occurring conditions. Quality and Safety in Health Care, 19(2), 113–116. doi:10.1136/qshc.2008.027706.
Kilbourne, A. M., Pirraglia, P. A. Lai, Z., Bauer, M.S., Charns, M. P., Greenwald, D., … Yano, E. M. (2011). Quality of general medical care among patients with serious mental illness: Does colocation of services matter? Psychiatric Services, 62(8), 922–928. doi:10.1176/ps.62.8.pss6208_0922.
Kronick, R., Gilmer, T., Dreyfus, T., & Lee, L. (2000). Improving health-based payment for Medicaid beneficiaires: CDPS. Health Care Financing Review, 21(3), 29.
Krupski, A., West, I. I., Scharf, D. M., Hopfenbeck, J., Andrus, G., Joesch, J. M., & Snowden, M. (2016). Integrating primary care into community mental health centers: Impact on utilization and costs of health care. Psychiatric Services. doi:10.1176/appi.ps.201500424.
Mangurian, C., Newcomer, J. W., Modlin, C., & Schillinger, D. (2016). Diabetes and cardiovascular care among people with severe mental illness: A literature review. Journal of General Internal Medicine, 31(9), 1083–1091. doi:10.1007/s11606-016-3712-4.
McGinty, E. E., Baller, J., Azrin, S. T., Juliano-Bult, D., & Daumit, G. L. (2015). Quality of medical care for persons with serious mental illness: A comprehensive review. Schizophrenia Research, 165(2–3), 227–235. doi:10.1016/j.schres.2015.04.010.
Mechanic, D., & Olfson, M. (2016). The Relevance of the affordable care act for improving mental health care. Annual Review of Clinical Psychology, 12(1), 515–542. doi:10.1146/annurev-clinpsy-021815-092936.
Mitchell, A. J., Delaffon, V., Vancampfort, D., Correll, C. U., & De Hert, M. (2011). Guideline concordant monitoring of metabolic risk in people treated with antipsychotic medication: Systematic review and meta-analysis of screening practices. Psychological Medicine, 42(1), 125–147. doi:10.1017/S003329171100105X.
Mitchell, A. J., Delaffon, V., Vancampfort, D., Correll, C. U., & De Hert, M. (2012). Guideline concordant monitoring of metabolic risk in people treated with antipsychotic medication: Systematic review and meta-analysis of screening practices. Psychological Medicine, 42(1), 125–147. doi:10.1017/S003329171100105X.
Nasrallah, H. A., Meyer, J. M., Goff, D. C., McEvoy, J. P., Davis, S. M., Stroup, T. S., & Lieberman, J. A. (2006). Low rates of treatment for hypertension, dyslipidemia and diabetes in schizophrenia: data from the CATIE schizophrenia trial sample at baseline. Schizophrenia Research, 86(1–3), 15–22.
National Committee for Quality Assurance. (2016). State of health care quality. Retrieved from http://www.ncqa.org/report-cards/health-plans/state-of-health-care-quality/2016-table-of-contents/schizophrenia.
National Committee for Quality Assurance. What is Hedis? Retrieved from http://www.ncqa.org/hedis-quality-measurement/what-is-hedis.
New York State Department of Health. (2016). Managed care reports. Retrieved from https://www.health.ny.gov/health_care/managed_care/reports/.
Osborn, D. P., Wright, C. A., Levy, G., King, M. B., Deo, R., & Nazareth, I. (2008). Relative risk of diabetes, dyslipidaemia, hypertension and the metabolic syndrome in people with severe mental illnesses: Systematic review and metaanalysis. Bmc Psychiatry, 8, 84. doi:10.1186/1471-244X-8-84.
Pincus, H. A., Spaeth-Rublee, B., & Watkins, K. E. (2011). The case for measuring quality in mental health and substance abuse care. Health Affairs, 30(4), 730–736. doi:10.1377/hlthaff.2011.0268.
Scharf, D. M. (2014). Evaluation of the SAMHSA primary and behavioral health care integration (PBHCI) grant program: Final report (task 13). Santa Monica, CA: RAND. https://www.rand.org/pubs/research_reports/RR546.html.
Scharf, D. M., Breslau, J., Schmidt Hackbarth, N., Kusuke, D., Staplefoote, B. L., & Pincus, H. A. (2014). An examination of New York State’s integrated primary and mental health care services for adults with serious mental illness. Rand Health Quarterly, 4, 13.
Scharf, D. M., Hackbarth, N. S., Eberhart, N. K., Horvitz-Lennon, M., Beckman, R., Han, B., …, Burnam, M. A. (2016) General medical outcomes from the primary and behavioral health care integration grant program. Psychiatric Services. doi:10.1176/appi.ps.201500352.
Funding
This research was supported by a grant from the National Institute of Mental Health (R01MH102379).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to report.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Study procedures were approved by the IRBs of the RAND Corporation and the New York State Office of Mental Health.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Breslau, J., Leckman-Westin, E., Yu, H. et al. Impact of a Mental Health Based Primary Care Program on Quality of Physical Health Care. Adm Policy Ment Health 45, 276–285 (2018). https://doi.org/10.1007/s10488-017-0822-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10488-017-0822-1