Abstract
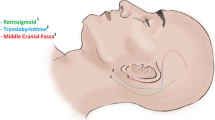
There are several surgical approaches for vestibular schwannoma (VS) resection. However, management has gradually shifted from microsurgical resection, toward surveillance and radiosurgery. One of the arguments against microsurgery via the middle fossa approach (MFA) is the risk of temporal lobe retraction injury or sequelae. Here, we sought to evaluate the incidence of temporal lobe retraction injury or sequela from a MFA via a systematic review of the existing literature. This systematic review was conducted according to the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines. Relevant studies reporting temporal lobe injury or sequela during MFA for VS were identified. Data was aggregated and subsequently analyzed to evaluate the incidence of temporal lobe injury. 22 studies were included for statistical analysis, encompassing 1522 patients that underwent VS resection via MFA. The overall rate of temporal lobe sequelae from this approach was 0.7%. The rate of CSF leak was 5.9%. The rate of wound infection was 0.6%. Meningitis occurred in 1.6% of patients. With the MFA, 92% of patients had good facial outcomes, and 54.9% had hearing preservation. Our series and literature review support that temporal lobe retraction injury or sequelae is an infrequent complication from an MFA for intracanalicular VS resection.

Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
References
Stangerup SE, Caye-Thomasen P (2012) Epidemiology and natural history of vestibular schwannomas. Otolaryngol Clin North Am 45(2):257–268, vii
Kosty JA, Stevens SM, Gozal YM et al (2019) Middle Fossa Approach for Resection of Vestibular Schwannomas: A Decade of Experience. Oper Neurosurg (Hagerstown) 16(2):147–158
Marinelli JP, Lohse CM, Carlson ML (2018) Incidence of Vestibular Schwannoma over the Past Half-Century: A Population-Based Study of Olmsted County. Minnesota Otolaryngol Head Neck Surg 159(4):717–723
Cioffi G, Yeboa DN, Kelly M, et al. (2020) Epidemiology of vestibular schwannoma in the United States, 2004–2016. Neurooncol Adv 2(1):vdaa135
Marinelli JP, Beeler CJ, Carlson ML, Caye-Thomasen P, Spear SA, Erbele ID (2022) Global Incidence of Sporadic Vestibular Schwannoma: A Systematic Review. Otolaryngol Head Neck Surg 167(2):209–214
Koo M, Lai JT, Yang EY, Liu TC, Hwang JH (2018) Incidence of Vestibular Schwannoma in Taiwan from 2001 to 2012: A Population-Based National Health Insurance Study. Ann Otol Rhinol Laryngol 127(10):694–697
Waterval J, Kania R, Somers T (2018) EAONO Position Statement on Vestibular Schwannoma: Imaging Assessment. What are the Indications for Performing a Screening MRI Scan for a Potential Vestibular Schwannoma? J Int Adv Otol 14(1):95–99
Marinelli JP, Nassiri AM, Habermann EB, Lohse CM, Holton SJ, Carlson ML (2021) Underreporting of Vestibular Schwannoma Incidence Within National Brain Tumor and Cancer Registries in the United States. Otol Neurotol 42(6):e758–e763
Neves Cavada M, Fook-Ho Lee M, Jufas NE, Harvey RJ, Patel NP (2021) Intracanalicular Vestibular Schwannoma: A Systematic Review and Meta-analysis of Therapeutics Outcomes. Otol Neurotol 42(3):351–362
Dang L, Tu NC, Chan EY (2020) Current imaging tools for vestibular schwannoma. Curr Opin Otolaryngol Head Neck Surg 28(5):302–307
Lees KA, Tombers NM, Link MJ et al (2018) Natural History of Sporadic Vestibular Schwannoma: A Volumetric Study of Tumor Growth. Otolaryngol Head Neck Surg 159(3):535–542
Salem N, Galal A, Mastronardi V, Talaat M, Sobhy O, Sanna M (2019) Audiological Evaluation of Vestibular Schwannoma Patients with Normal Hearing. Audiol Neurootol 24(3):117–126
Marinelli JP, Schnurman Z, Killeen DE et al (2022) Long-term natural history and patterns of sporadic vestibular schwannoma growth: A multi-institutional volumetric analysis of 952 patients. Neuro Oncol 24(8):1298–1306
Chan SA, Marinelli JP, Hahs-Vaughn DL, Nye C, Link MJ, Carlson ML (2021) Evolution in Management Trends of Sporadic Vestibular Schwannoma in the United States Over the Last Half-century. Otol Neurotol 42(2):300–305
Reznitsky M, Petersen M, West N, Stangerup SE, Caye-Thomasen P (2021) The natural history of vestibular schwannoma growth-prospective 40-year data from an unselected national cohort. Neuro Oncol 23(5):827–836
Khandalavala KR, Saba ES, Kocharyan A et al (2022) Hearing Preservation in Observed Sporadic Vestibular Schwannoma: A Systematic Review. Otol Neurotol 43(6):604–610
Noudel R, Gomis P, Duntze J, Marnet D, Bazin A, Roche PH (2009) Hearing preservation and facial nerve function after microsurgery for intracanalicular vestibular schwannomas: comparison of middle fossa and retrosigmoid approaches. Acta Neurochir (Wien) 151(8):935–944; discussion 944–935
Ogino A, Lunsford LD, Long H et al (2021) Stereotactic radiosurgery as the first-line treatment for intracanalicular vestibular schwannomas. J Neurosurg 135(4):1051–1057
Dzierzecki S, Turek G, Czapski B et al (2020) Gamma knife surgery in the treatment of intracanalicular vestibular schwannomas. Acta Neurol Scand 141(5):415–422
Balossier A, Tuleasca C, Delsanti C et al (2023) Long-Term Hearing Outcome After Radiosurgery for Vestibular Schwannoma: A Systematic Review and Meta-Analysis. Neurosurgery 92(6):1130–1141
Jakubeit T, Sturtz S, Sow D et al (2022) Single-fraction stereotactic radiosurgery versus microsurgical resection for the treatment of vestibular schwannoma: a systematic review and meta-analysis. Syst Rev 11(1):265
Zhang Z, Nguyen Y, De Seta D et al (2016) Surgical treatment of sporadic vestibular schwannoma in a series of 1006 patients. Acta Otorhinolaryngol Ital 36(5):408–414
Fík Z, Zverina E, Lisy J et al (2023) Hearing After Vestibular Schwannoma Surgery: Is It Preserved Forever? Otol Neurotol 44(3):260–265
Peker S, Samanci Y, Ozdemir IE, Kunst HPM, Eekers DBP, Temel Y (2022) Long-term results of upfront, single-session Gamma Knife radiosurgery for large cystic vestibular schwannomas. Neurosurg Rev 46(1):2
Anaizi AN, DiNapoli VV, Pensak M, Theodosopoulos PV (2016) Small Vestibular Schwannomas: Does Surgery Remain a Viable Treatment Option? J Neurol Surg B Skull Base 77(3):212–218
Frischer JM, Gruber E, Schoffmann V et al. (2018) Long-term outcome after Gamma Knife radiosurgery for acoustic neuroma of all Koos grades: a single-center study. J Neurosurg 1–10
Ansari SF, Terry C, Cohen-Gadol AA (2012) Surgery for vestibular schwannomas: a systematic review of complications by approach. Neurosurg Focus 33(3):E14
Berger A, Alzate JD, Bernstein K et al (2022) Modern Hearing Preservation Outcomes After Vestibular Schwannoma Stereotactic Radiosurgery. Neurosurgery 91(4):648–657
Ismail O, Sobhy O, Assal S, Sanghera P, Begg P, Irving R (2022) Comparing Hearing Outcomes in Irradiated and Conservatively Managed Vestibular Schwannoma. Otol Neurotol 43(3):e374–e381
Watanabe S, Yamamoto M, Kawabe T et al (2016) Stereotactic radiosurgery for vestibular schwannomas: average 10-year follow-up results focusing on long-term hearing preservation. J Neurosurg 125(Suppl 1):64–72
Dowling EM, Patel NS, Lohse CM et al (2019) Durability of Hearing Preservation Following Microsurgical Resection of Vestibular Schwannoma. Otol Neurotol 40(10):1363–1372
Boari N, Bailo M, Gagliardi F et al (2014) Gamma Knife radiosurgery for vestibular schwannoma: clinical results at long-term follow-up in a series of 379 patients. J Neurosurg 121(Suppl):123–142
Bashjawish B, Kilic S, Baredes S, Eloy JA, Liu JK, Ying YM (2019) Changing trends in management of vestibular schwannoma: A National Cancer Database study. Laryngoscope 129(5):1197–1205
Gupta VK, Thakker A, Gupta KK (2020) Vestibular Schwannoma: What We Know and Where We are Heading. Head Neck Pathol 14(4):1058–1066
Kirchmann M, Karnov K, Hansen S, Dethloff T, Stangerup SE, Caye-Thomasen P (2017) Ten-Year Follow-up on Tumor Growth and Hearing in Patients Observed With an Intracanalicular Vestibular Schwannoma. Neurosurgery 80(1):49–56
Wu MJ, Knoll RM, Chen JX et al (2022) A Subset of Intracanalicular Vestibular Schwannomas Demonstrates Minimal Growth Over a 10-Year Period. Otol Neurotol 43(3):376–384
van Linge A, Borsboom GJ, Wieringa MH, Goedegebure A (2016) Hearing Loss Progresses Faster in Patients With Growing Intracanalicular Vestibular Schwannomas. Otol Neurotol 37(9):1442–1448
Alzhrani G, Shelton C, Couldwell WT (2017) Middle fossa approach for resection of vestibular schwannoma. Acta Neurochir (Wien) 159(6):1023–1026
Wang AC, Chinn SB, Than KD et al (2013) Durability of hearing preservation after microsurgical treatment of vestibular schwannoma using the middle cranial fossa approach. J Neurosurg 119(1):131–138
Ginzkey C, Scheich M, Harnisch W et al (2013) Outcome on hearing and facial nerve function in microsurgical treatment of small vestibular schwannoma via the middle cranial fossa approach. Eur Arch Otorhinolaryngol 270(4):1209–1216
Kutz JW, Jr., Scoresby T, Isaacson B et al. (2012) Hearing preservation using the middle fossa approach for the treatment of vestibular schwannoma. Neurosurgery 70(2):334–340; discussion 340–331
Tawfik KO, Khan UA, Friedman RA (2021) Treatment of Small Vestibular Schwannomas. Curr Otorhinolaryngol Reports 9(2):139–154
Committee on Hearing and Equilibrium guidelines for the evaluation of hearing preservation in acoustic neuroma (vestibular schwannoma). (1995) American Academy of Otolaryngology-Head and Neck Surgery Foundation, INC. Otolaryngol Head Neck Surg 113(3):179–180
House JW, Brackmann DE (1985) Facial nerve grading system. Otolaryngol Head Neck Surg 93(2):146–147
Gantz BJ, Parnes LS, Harker LA, McCabe BF (1986) Middle cranial fossa acoustic neuroma excision: results and complications. Ann Otol Rhinol Laryngol 95(5 Pt 1):454–459
Shelton C, Brackmann DE, House WF, Hitselberger WE (1989) Middle fossa acoustic tumor surgery: results in 106 cases. Laryngoscope 99(4):405–408
Sameshima T, Fukushima T, McElveen JT, Jr., Friedman AH (2010) Critical assessment of operative approaches for hearing preservation in small acoustic neuroma surgery: retrosigmoid vs middle fossa approach. Neurosurgery 67(3):640–644; discussion 644–645
Budohoski KP, Rennert RC, Gordon SA, et al. (2022) Factors associated with hearing outcomes after a middle fossa approach in 131 consecutive patients with vestibular schwannomas. J Neurosurg 1–10
Meyer TA, Canty PA, Wilkinson EP, Hansen MR, Rubinstein JT, Gantz BJ (2006) Small acoustic neuromas: surgical outcomes versus observation or radiation. Otol Neurotol 27(3):380–392
**an-Hao J, Zhen G, Ya-Sheng Y, Wei-Dong Z (2022) Resection of Vestibular Schwannoma Through Middle Cranial Fossa Approach with Endoscopic Assistance. World Neurosurg 158:e225–e230
Moon IS, Choi IS, Shin SH, Yang S, Jung Y, Na G (2022) Endoscopic-Assisted Keyhole Middle Cranial Fossa Approach for Small Vestibular Schwannomas. J Clin Med 11(9)
Kohlberg GD, Lipschitz N, Raghavan AM et al (2021) Middle Cranial Fossa Approach to Vestibular Schwannoma Resection in the Older Patient Population. Otol Neurotol 42(1):e75–e81
Lipschitz N, Kohlberg GD, Tawfik KO et al (2019) Cerebrospinal Fluid Leak Rate after Vestibular Schwannoma Surgery via Middle Cranial Fossa Approach. J Neurol Surg B Skull Base 80(4):437–440
Scheich M, Ginzkey C, Ehrmann Muller D, ShehataDieler W, Hagen R (2017) Complications of the Middle Cranial Fossa Approach for Acoustic Neuroma Removal. J Int Adv Otol 13(2):186–190
Raheja A, Bowers CA, MacDonald JD et al (2016) Middle Fossa Approach for Vestibular Schwannoma: Good Hearing and Facial Nerve Outcomes with Low Morbidity. World Neurosurg 92:37–46
DeMonte F, Gidley PW (2012) Hearing preservation surgery for vestibular schwannoma: experience with the middle fossa approach. Neurosurg Focus 33(3):E10
Arts HA, Telian SA, El-Kashlan H, Thompson BG (2006) Hearing preservation and facial nerve outcomes in vestibular schwannoma surgery: results using the middle cranial fossa approach. Otol Neurotol 27(2):234–241
Colletti V, Fiorino F (2005) Is the middle fossa approach the treatment of choice for intracanalicular vestibular schwannoma? Otolaryngol Head Neck Surg 132(3):459–466
Stripf T, Bruehl K, Mann WJ, Amedee RG (2004) Clinical and radiologic sequelae of the middle fossa approach to the internal auditory canal. Otol Neurotol 25(5):787–790
Thomsen J, Stougaard M, Becker B, Tos M, Jennum P (2000) Middle fossa approach in vestibular schwannoma surgery. Postoperative hearing preservation and EEG changes. Acta Otolaryngol 120(4):517–522
Holsinger FC, Coker NJ, Jenkins HA (2000) Hearing preservation in conservation surgery for vestibular schwannoma. Am J Otol 21(5):695–700
Slattery WH 3rd, Brackmann DE, Hitselberger W (1997) Middle fossa approach for hearing preservation with acoustic neuromas. Am J Otol 18(5):596–601
Weber PC, Gantz BJ (1996) Results and complications from acoustic neuroma excision via middle cranial fossa approach. Am J Otol 17(4):669–675
Brackmann DE, House JR 3rd, Hitselberger WE (1994) Technical modifications to the middle fossa craniotomy approach in removal of acoustic neuromas. Am J Otol 15(5):614–619
Monfared A, Mudry A, Jackler R (2010) The history of middle cranial fossa approach to the cerebellopontine angle. Otol Neurotol 31(4):691–696
House WF (1961) Surgical exposure of the internal auditory canal and its contents through the middle, cranial fossa. Laryngoscope 71:1363–1385
Yokoh A, Sugita K, Kobayashi S (1987) Clinical study of brain retraction in different approaches and diseases. Acta Neurochir (Wien) 87(3–4):134–139
Fukamachi A, Koizumi H, Nukui H (1985) Postoperative intracerebral hemorrhages: a survey of computed tomographic findings after 1074 intracranial operations. Surg Neurol 23(6):575–580
Li D, Zeng M, Yao Y, Zhang N, Yang T, **a C (2022) Retractorless Surgery for Petroclival Meningiomas via the Subtemporal Approach: A Try to Reduce Brain Retraction Injury. Comput Math Methods Med 2022:6436542
Kashimura H, Ogasawara K, Kubo Y et al (2008) Brain retraction technique using gelatin sponge in the subtemporal approach. Neurol Med Chir (Tokyo) 48(3):143–146
Nelson RF, Roche JP, Gantz BJ, Hansen MR (2016) Middle Cranial Fossa (MCF) Approach Without the Use of Lumbar Drain for the Management of Spontaneous Cerebral Spinal Fluid (CSF) Leaks. Otol Neurotol 37(10):1625–1629
Teschner M, Lang CP, Salcher R, Haumann S, Lenarz T (2015) Impact of Elevation of Temporal Lobe During Middle Fossa Acoustic Neuroma Surgery on Contralateral Speech Discrimination. Otol Neurotol 36(10):1720–1724
Ren Y, Tawfik KO, Cueva RA (2021) Audiometric Outcomes Following Transmastoid and Middle Cranial Fossa Approaches for Repair of Cerebrospinal Fluid Otorrhea. Otol Neurotol 42(3):424–430
Lobo BC, Baumanis MM, Nelson RF (2017) Surgical repair of spontaneous cerebrospinal fluid (CSF) leaks: A systematic review. Laryngoscope Investig Otolaryngol 2(5):215–224
Woodson EA, Dempewolf RD, Gubbels SP et al (2010) Long-term hearing preservation after microsurgical excision of vestibular schwannoma. Otol Neurotol 31(7):1144–1152
Quist TS, Givens DJ, Gurgel RK, Chamoun R, Shelton C (2015) Hearing preservation after middle fossa vestibular schwannoma removal: are the results durable? Otolaryngol Head Neck Surg 152(4):706–711
Ahmed S, Arts HA, El-Kashlan H, Basura GJ, Thompson BG, Telian SA (2018) Immediate and Long-term Hearing Outcomes With the Middle Cranial Fossa Approach for Vestibular Schwannoma Resection. Otol Neurotol 39(1):92–98
Killeen DE, Barnett SL, Mickey BE, Hunter JB, Isaacson B, Kutz JW Jr (2021) The Association of Vestibular Schwannoma Volume With Facial Nerve Outcomes After Surgical Resection. Laryngoscope 131(4):E1328–E1334
Ren Y, MacDonald BV, Tawfik KO, Schwartz MS, Friedman RA (2021) Clinical Predictors of Facial Nerve Outcomes After Surgical Resection of Vestibular Schwannoma. Otolaryngol Head Neck Surg 164(5):1085–1093
Macielak RJ, Driscoll CLW, Link MJ, Haynes DS, Lohse CM, Carlson ML (2020) Vestibular Schwannoma Practice Patterns: An International Cross-specialty Survey. Otol Neurotol 41(10):e1304–e1313
Giammattei L, Passeri T, Abbritti R, et al. (2022) Surgical morbidity of the extradural anterior petrosal approach: the Lariboisière experience. J Neurosurg 138(1):276–286. https://doi.org/10.3171/2022.3.JNS212962. Published 2022 May 13
di Russo P, Giammattei L, Passeri T et al (2022) Lariboisiere Hospital pre-operative surgical checklist to improve safety during transpetrosal approaches. Acta Neurochir (Wien) 164(11):2819–2832. https://doi.org/10.1007/s00701-022-05278-8
Moon IS, Choi IS, Shin SH, Yang S, Jung Y, Na G (2022) Endoscopic-Assisted Keyhole Middle Cranial Fossa Approach for Small Vestibular Schwannomas. J Clin Med 11(9):2324. https://doi.org/10.3390/jcm11092324. Published 2022 Apr 21
Funding
No funding was received for this project.
Author information
Authors and Affiliations
Contributions
G.F.M., G.J.R., K.P. and I.P. all contributed to collecting the data, writing the manuscript, analyzing the data, confirming methodology and investigating. K.A.,C.D., S.L.,H.V.L. and S.A. all supervised the project and methodologies and approved the final manuscript.
Corresponding author
Ethics declarations
Our authors have no financial relationships to disclose relevant to the submission.
Ethical approval
This declaration is not applicable, the information in the submission is available in the current neurosurgical literature.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Flores-Milan, G., Rainone, G.J., Piper, K. et al. Temporal lobe injury with middle fossa approach to intracanalicular vestibular schwannomas: a systematic review. Neurosurg Rev 47, 188 (2024). https://doi.org/10.1007/s10143-024-02425-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10143-024-02425-w