Abstract
Background
This study evaluated the safety, effectiveness, and feasibility of indocyanine green (ICG) tracing in guiding lymph-node (LN) dissection during laparoscopic D2 radical gastrectomy in patients with advanced gastric cancer (AGC) after neoadjuvant chemotherapy (NAC).
Method
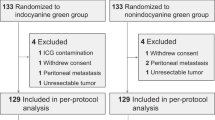
We retrospectively analyzed data on 313 patients with clinical stage of cT1-4N0-3M0 who underwent laparoscopic radical gastrectomy after NAC between February 2010 and October 2020 from two hospitals in China. Grouped according to whether ICG was injected. For the ICG group (n = 102) and non-ICG group (n = 211), 1:1 propensity matching analysis was used.
Results
After matching, there was no significant difference in the general clinical pathological data between the two groups (ICG vs. non-ICG: 94 vs. 94). The average number of total LN dissections was significantly higher in the ICG group and lower LN non-compliance rate than in the non-ICG group. Subgroup analysis showed that among patients with LN and tumor did not shrink after NAC, the number of LN dissections was significantly more and LN non-compliance rate was lower in the ICG group than in the non-ICG group. Intraoperative blood loss was significantly lesser in the ICG group than in the non-ICG group, while the recovery and complications of the two groups were similar.
Conclusion
For patients with poor NAC outcomes, ICG tracing can increase the number of LN dissections during laparoscopic radical gastrectomy, reduce the rate of LN non-compliance, and reduce intraoperative bleeding. Patients with AGC should routinely undergo ICG-guided laparoscopic radical gastrectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is the fifth most common malignant tumor worldwide and the third highest cause of cancer mortality. Although the 5-year survival rate of patients with early gastric cancer exceeds 90%, for patients with locally advanced gastric cancer (AGC), the 5-year survival rate is low even with radical surgery [1,2,3,4]. In 1994, Kitano et al. [5] reported laparoscopic radical gastrectomy, with the development of minimally invasive equipment and technology, the safety and effectiveness of laparoscopic radical gastrectomy are gradually being recognized [6]. Since the MAGIC trial in 2006, which proved for the first time that preoperative neoadjuvant chemotherapy (NAC) combined with surgery can significantly improve the 5-year overall survival rate of patients with AGC [7], NAC has gradually become an indispensable part of treatment for AGC patients. However, for patients receiving NAC, fibrosis of lymphatic tissue caused by NAC and loss of normal anatomical planes caused by cytotoxicity are technical challenges for laparoscopic lymph-node (LN) dissection [8,9,10]. Although studies have confirmed the safety and feasibility of laparoscopic distal gastrectomy for patients with neoadjuvant gastric cancer, for more technically difficult whole-stomach resections and for inexperienced surgeons, neoadjuvant standard gastric cancer radical resection after chemotherapy is a challenge. In contrast, Taylor et al. [11] found that, due to reasons including tumor downgrading, patients receiving NAC require more LN dissections to truly reflect the prognosis of patients. Therefore, for patients with gastric cancer who have undergone NAC and plan to undergo laparoscopic surgery, surgeons should focus on how to safely complete the operation and complete the standardized and precise LN dissection.
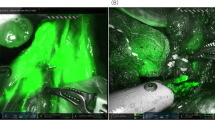
Indocyanine green (ICG) near-infrared light imaging technology, as a new surgical navigation technology, has achieved relatively positive results in sentinel LN dissection and in detecting the location of tumors such as breast cancer and non-small cell lung cancer [11,12,13,14]. Furthermore, in gastric cancer research, prospective studies have reported that ICG can significantly increase the number of LN dissections during laparoscopic radical gastrectomy [28,29,30,31]. However, in neoadjuvant patients with AGC, fibrosis reaction or cytotoxicity caused by chemotherapy can cause loss of the normal tissue plane. However, evidence regarding whether it will affect LN visualization or tissue discrimination by ICG in these patients is lacking. This study included patients with AGC who underwent laparoscopic radical resection after NAC in two centers in China and analyzed the relationship between ICG injection and the number of LNs dissected and LN non-compliance in detail. Our study shows that ICG can reduce intraoperative blood loss without increasing the operation time and number of complications, and it can guide the surgeon to dissected more LNs during laparoscopic radical gastrectomy after neoadjuvant therapy and reduce the LN non-compliance rate. In particular, for surgical patients with poor chemotherapy effects, the effect is obvious.
The total number of LNs dissected and the LN non-compliance rate are of great significance in radical gastrectomy. Previous studies have confirmed that, regardless of whether the dissected LNs are metastasized, the perigastric LNs are thoroughly dissected during surgery, the number of LNs is detected, and the rate of LN non-conformance is reduced. Accurate staging, selection of appropriate subsequent treatment options, and improvement in prognoses are of great significance. Studies have proven that patients with NAC need more LN dissections to truly reflect the tumor stage and prognosis of patients [11]. Among patients with gastric cancer who did not receive NAC, our center concluded through randomized-controlled trial research that, in the early stage of disease, ICG can guide the surgeon to dissect more LNs and LNs during laparoscopic radical gastrectomy without increasing the operation time and complications, effectively reducing LN inconsistencies in patients undergoing total gastrectomy [ Huang CM and Yan S had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Ahn HS, Lee HJ, Hahn S, Kim WH, Lee KU, Sano T, et al. Evaluation of the seventh American Joint Committee on Cancer/International Union Against Cancer Classification of gastric adenocarcinoma in comparison with the sixth classification. Cancer. 2010;116:5592–8. Sobin LH, Wittekind CH. TNM Classification of Malignant Tumors (6th edn). New York: Wiley-Liss; 2002. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC Cancer Staging Handbook (7th edn). New York: Springer; 2010. Ahn HS, Lee HJ, Yoo MW, Jeong SH, Park DJ, Kim HH, et al. Changes in clinicopathological features and survival after gastrectomy for gastric cancer over a 20-year period. Br J Surg. 2011;98:255–60. Kitano S, Iso Y, Moriyama M, Sugimachi K. Laparoscopyassisted Billroth I gastrectomy. Surg Laparosc Endosc. 1994;4:146–8. Yu J, Huang C, Sun Y, et al. Effect of laparoscopic vs open distal gastrectomy on 3-year disease-free survival in patients with locally advanced gastric cancer: The CLASS-01 randomized clinical trial. JAMA. 2019;321(20):1983–92. https://doi.org/10.1001/jama.2019.5359. Cunningham D, Allum WH, Stenning SP, et al. MAGIC trial participants. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355(1):11–20. Li Z, Shan F, Ying X, et al. Assessment of laparoscopic distal gastrectomy after neoadjuvant chemotherapy for locally advanced gastric cancer: a randomized clinical trial. JAMA Surg. 2019;154(12):1093–101. https://doi.org/10.1001/jamasurg.2019.3473. An JY, Kim KM, Kim YM, Cheong JH, Hyung WJ, Noh SH. Surgical complications in gastric cancer patients preoperatively treated with chemotherapy: their risk factors and clinical relevance. Ann Surg Oncol. 2012;19(8):2452–8. https://doi.org/10.1245/s10434-012-2267-9. Fujisaki M, Mitsumori N, Shinohara T, et al. Short- and long-term outcomes of laparoscopic versus open gastrectomy for locally advanced gastric cancer following neoadjuvant chemotherapy. Surg Endosc. 2020. https://doi.org/10.1007/s00464-020-07552-1. Vahrmeijer AL, Hutteman M, van der Vorst JR, van de Velde CJH, Frangioni JV. Image-guided cancer surgery using near-infrared fluorescence. Nat Rev Clin Oncol. 2013;10(9):507–518. https://doi.org/10.1038/nrclinonc.2013.123 Valente SA, Al-Hilli Z, Radford DM, Yanda C, Tu C, Grobmyer SR. Near infrared fluorescent LN map** with indocyanine green in breast cancer patients: a prospective trial. J Am Coll Surg. 2019;228(4):672–8. https://doi.org/10.1016/j.jamcollsurg.2018.12.001. Yamashita S, Tokuishi K, Anami K, et al. Video-assisted thoracoscopic indocyanine green fluorescence imaging system shows sentinel LNs in non–small-cell lung cancer. J Thorac Cardiovasc Surg. 2011;141(1):141–4. https://doi.org/10.1016/j.jtcvs.2010.01.028. Brouwer OR, Klop WMC, Buckle T, et al. Feasibility of sentinel node biopsy in head and neck melanoma using a hybrid radioactive and fluorescent tracer. Ann Surg Oncol. 2012;19(6):1988–94. https://doi.org/10.1245/s10434-011-2180-7. Chen QY, **e JW, Zhong Q, et al. Safety and efficacy of indocyanine green tracer-guided LN dissection during laparoscopic radical gastrectomy in patients with gastric cancer: a randomized clinical trial. JAMA Surg. 2020;155(4):300–11. https://doi.org/10.1001/jamasurg.2019.6033. Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47. https://doi.org/10.1016/j.ejca.2008.10.026. Association JGC. Japanese gastric cancer treatment guidelines 2014 (ver 4). Gastric Cancer. 2017;20(1):1–19. https://doi.org/10.1007/s10120-016-0622-4. Huang CM, Zheng CH. Laparoscopic Gastrectomy for Gastric Cancer. Berlin: Springer; 2015. Huang CM, et al. Laparoscopic suprapancreatic LN dissection for advanced gastric cancer using a left-sided approach. Ann Surg Oncol. 2015;22:2351. Huang CM, et al. A 346 case analysis for laparoscopic spleen-preserving No.10 LN dissection for proximal gastric cancer: a single center study. Plos One 2014;9:e108480. Chen QY, et al. Strategies of laparoscopic spleen-preserving splenic hilar LN dissection for advanced proximal gastric cancer. World J Gastrointest Surg. 2016;8:402–6. Maezawa Y, et al. Priority of LN dissection for proximal gastric cancer invading the greater curvature. Gastric Cancer. 2018;21:569–72. Association JGC. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer 2011;14:101. De Steur WO, et al. Quality control of LN dissection in the Dutch Gastric Cancer Trial. Br J Surg. 2015;102:1388–93. Chen QY, et al. Laparoscopic total gastrectomy for upper-middle advanced gastric cancer: analysis based on LN noncompliance. Gastric Cancer 2019. Dindo D, et al. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205. Sabbagh C, Manceau G, Mege D, et al. Is adjuvant chemotherapy necessary for obstructing stage II colon cancer? Results from a propensity score analysis of the french surgical association database. Ann Surg. 2020. https://doi.org/10.1097/SLA.0000000000003832. Lan Y-T, Huang K-H, Chen P-H, et al. A pilot study of LN map** with indocyanine green in robotic gastrectomy for gastric cancer. SAGE Open Med. 2017;5(114):2050312117727444. https://doi.org/10.1177/2050312117727444. Kim T-H, Kong S-H, Park J-H, et al. Assessment of the completeness of LN dissection using near-infrared imaging with indocyanine green in laparoscopic gastrectomy for gastric cancer. J Gastric Cancer. 2018;18(2):161–71. https://doi.org/10.5230/jgc.2018.18.e19. Tajima Y, Murakami M, Yamazaki K, et al. Sentinel node map** guided by indocyanine green fluorescence imaging during laparoscopic surgery in gastric cancer. Ann Surg Oncol. 2010;17(7):1787–93. https://doi.org/10.1245/s10434-010-0944-0. Kwon IG, Son T, Kim H-I, Hyung WJ. Fluorescent lymphography-guided lymphadenectomy during robotic radical gastrectomy for gastric cancer. JAMA Surg. 2019;154(2):150–8. https://doi.org/10.1001/jamasurg.2018.4267. Hu X. Zhonghua wei chang wai ke za zhi. Chinese J Gastrointest Surg. 2013;16(6):509–12. Gioux S, et al. Image-guided surgery using invisible near-infrared light: fundamentals of clinical translation. Mol Imaging. 2010;9:237–55. Schaafsma BE, et al. The clinical use of indocyanine green as a near-infrared fluorescent contrast agent for image-guided oncologic surgery. J Surg Oncol. 2011;104:323–32. This work was supported by scientific and technological innovation joint capital projects of Fujian province (2017Y9011, 2017Y9004, and 2018Y9041) and the general project of Startup Fund of Fujian Medical University (2019QH1033). Conception and design: Ze-Ning Huang, Cheng-Hao Liu, Wen-Wu Qiu, Su-Yan, and Changming Huang. Provision of study materials or patients: all authors. Collection and assembly of data: all authors. Data analysis and interpretation: Ze-Ning Huang, Cheng-Hao Liu, Wen-Wu Qiu, Su-Yan, Chao-Hui Zheng, and ** Li. Manuscript writing: all authors. Final approval of manuscript: all authors. Accountable for all aspects of the work: all authors. There are no conflicts of interest or financial ties to disclose from any of author. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. Informed consent or a substitute for it was obtained from all patients for inclusion in the study. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Below is the link to the electronic supplementary material. Supplementary file7 (WMV 82843 KB) Huang, ZN., Su-Yan, Qiu, WW. et al. Assessment of indocyanine green tracer-guided lymphadenectomy in laparoscopic gastrectomy after neoadjuvant chemotherapy for locally advanced gastric cancer: results from a multicenter analysis based on propensity matching.
Gastric Cancer 24, 1355–1364 (2021). https://doi.org/10.1007/s10120-021-01211-7 Received: Accepted: Published: Issue Date: DOI: https://doi.org/10.1007/s10120-021-01211-7Data accessibility statement
References
Funding
Author information
Authors and Affiliations
Contributions
Corresponding author
Ethics declarations
Conflicts of interest
Human rights statement and informed consent
Additional information
Publisher's Note
Supplementary Information
Rights and permissions
About this article
Cite this article
Keywords