Abstract
Purpose
We studied the effectiveness of biomechanically calculated abdominal wall reconstructions for incisional hernias of varying complexity in an open, prospective observational registry trial.
Methods
From July 1st, 2017 to December 31st, 2020, four hospitals affiliated with the University of Heidelberg recruited 198 patients with complex incisional hernias. Hernias were repaired using biomechanically calculated reconstructions and materials classified on their grip** force towards cyclic load. This approach determines the required strength preoperatively based on the hernia size, using the Critical Resistance to Impacts related to Pressure. The surgeon is supported in reliably determining the Gained Resistance, which is based on the mesh-defect-area-ratio, as well as other mesh and suture factors, and the tissue stability. Tissue stability is defined as a maximum distension of 1.5 cm upon a Valsalva maneuver. In complex cases, a CT scan of the abdomen can be used to assess unstable tissue areas both at rest and during Valsalva’s maneuver.
Results
Larger and stronger grip** meshes were required for more complex cases to achieve a durable repair, especially for larger hernia sizes. To achieve durable repairs, the number of fixation points increased while the mesh-defect area ratio decreased. Performing these repairs required more operating room time. The complication rate remained low. Less than 1% of recurrences and low pain levels were observed after 3 years.
Conclusions
Biomechanical stability, defined as the resistance to cyclic load, is crucial in preventing postoperative complications, including recurrences and chronic pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many people worldwide require surgical treatment for an abdominal incisional hernia every year [1]. Recurrence and chronic pain are significant risks. Around 25% recur within five years. Ten percent of chronic pain is observed [2]. Patients with complex incisional hernias experience more recurrences and higher pain levels. Biomechanically calculated reconstruction (BCR) offers superior outcomes [3].
BCR determines the required strength (critical resistance to impacts related to pressure—CRIP). The surgeon calculates the strength of the designed repair preoperatively (gained resistance—GRIP). The GRIP considers the mesh-defect-area-ratio (MDAR), mesh, suture and other factors [3,4,5].
We investigated the effectiveness of BCR for incisional hernias of varying complexity. Our analysis is based on a cohort of patients observed prospectively.
Materials and methods
Patients
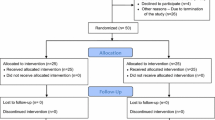
From July 1st, 2017 to December 31st, 2020, four hospitals affiliated with the University of Heidelberg recruited 198 patients for an open observational prospective registry study on complex incisional hernia repair. These patients were included in the Stronghold chapter of the Herniamed® Registry [3].
The Stronghold study is an extension of the Herniamed® registry. Stronghold started in 2017. The aim of the registry is to improve the quality of patient care by monitoring procedures and analysing outcome data. All interested surgeons can easily enter data according to a scientifically validated standard procedure. Patient consent is required [6]. STRONGHOLD follows the same principles as any Herniamed® subset. But it collects seven additional items for biomechanically calculated reconstruction: form of mesh implanted, minimal overlap, number and kind of fixation, pull-out or adapting sutures, type of peritoneal closure and MDAR.
We excluded seven deceased patients from the analysis. The only recurrence is presented and discussed separately. The remainder of 190 patients were classified for complexity. The complexity of incisional hernia repair was evaluated using the Herniamed® approach published in 2021 [2]. The complexity of incisional hernia increases with a defect width above 10 cm, a lateral defect site, a recurrent hernia, age over 80, BMI over 30, comorbidities with adverse metabolic consequences (such as diabetes mellitus), elevated intraabdominal pressure (such as chronic obstructive airways disease), increased risk of bleeding (such as genetic or iatrogenic clot reduction), reduced wound healing (such as concomitant chemotherapy), abnormal gait (for example after a stroke or an amputation), concomitant stoma or intra-abdominal bowel repair (e.g. for the relief of obstruction) and intensified surgery such as component separation. We developed the incisional hernia complexity score by awarding one point for each category. If multiple comorbidity-related risk factors were present, they were combined into a single point.
Surgical procedures
Our hernia repair is based on the concept of biomechanically calculated reconstruction (BCR). The concept is guided by three questions to be answered during the evaluation process (as illustrated in Fig. 1).
The clinical pathway for biomechanically calculated repair (BCR) involves clinical assessment, abdominal CT with Valsalva if necessary, and calculation of MDAR, CRIP and GRIP values as previously described in references [3,4,5] and [10]. The process is guided by three questions (Q 1–3). The arrow shows the iteration process to reach GRIP > CRIP. The following calculations are included: CRIP = (0.5 * hernia size + 15) * tissue distension [3]. GRIP = MDAR * coefficients for mesh adhesiveness, mesh position in the abdominal wall, number and type of fixation plus factors for peritoneal and fascial closure [3]. For a durable reconstruction, GRIP should be above CRIP
BCR yields CRIP and GRIP to guide the design of the surgical procedure. BCR preoperatively determines the required strength, depending on the hernia size, using Critical Resistance to Impacts related to Pressure (CRIP). Mesh-defect-area-ratio, CRIP and GRIP values were calculated as previously described (Fig. 1) [3,4,5]. GRIP is based on the mesh-defect-area-ratio, mesh and suture factors. The distension of the hernia size and/or the unstable area of the abdominal wall as a measure of tissue stability influences CRIP. Calculating CRIP and GRIP involves four divisions, six multiplications, and one to two additions. It takes approximately five minutes with a pocket calculator. We used a conventional Excel® sheet to determine the hernia and mesh sizes, the number and type of fixation, and the position within the abdominal wall.
Tissue stability was defined as a maximum distension of 1.5 cm during the Valsalva maneuver. In complex cases, unstable tissue areas can be assessed with a CT scan of the abdomen at rest and during Valsalva’s maneuver. To evaluate by hand, three observers must take at least four independent readings of the hernia's width, length, and height. This ensures an interobserver variation of less than 5% [7]. To speed up the process, we developed HEDI [9]. Most procedures were performed with an open access but MILOS or laparoscopic approaches were also used [4, 5].
The number of intraoperative complications may include bowel lacerations that do not open the internal lining and may be closed with simple sutures. It may also include bleeding requiring hemostatic sutures and unwanted events of any kind. Postoperative complications may include wound or mesh infection or seroma formation, deep vein thrombosis, pulmonary embolism, pneumonia, bleeding, urinary infection, transient or prolonged myocardial or brain ischemia and stroke. Any re-operation within 30 days was recorded.
Hernia repair was embedded into a pre- and rehabilitation program (Fig. 3).
Pre- and rehabilitation before and after BCR. CTAV computed tomography at rest and during a Valsalva maneuver, CRIP critical resistance to impacts related to pressure, GRIP gained resistance to impacts related to pressure. Wounds typically heal within two weeks. To promote stable scar formation, the authors recommend to wear an abdominal binder during wound healing, both day and night, and during physical activity afterwards
Follow up procedures
Patients were regularly followed-up via telephone interviews with themselves, known relatives, or family physicians. During these interviews, patients were asked about any unwanted effects, such as pain at rest or during exercise, that required medication. All re-operations, including imaging and a review of the OR report, were assessed. Patients with bulges on the body were asked to come to the hospital for clinical examination and, if necessary, ultrasonography, magnetic resonance imaging or computed tomography. No patient was lost to follow-up.
Statistics
Key descriptive statistics were calculated as given in Tables 1–5. As the data were skewed, non-parametric tests (group homogeneity with Kruskal–Wallis, then u-tests if necessary) were evaluated.
Results
In the study group without recurrences, 95 women and 95 men had a median age of 64 years (mean ± SD: 63 ± 12, range: 27–92 years). The only recurrence occurred in May 2020, eight months after the initial repair, in a female recipient of liver transplant.
After classification to the new Herniamed® approach, 18 patients no longer underwent a complex incisional hernia repair. Each remaining patient had between one and five risk factors (refer to Table 1).
In the remaining 172 patients, the complexity of the incisional hernia ranged from one to five, as shown in Table 2. Otherwise, the cohorts are comparable.
Uncomplicated cases with a complexity score of 0 consisted of primary incisional hernias treated electively. As complexity increases, the number of male patients increases, while age and BMI remain constant. The increase in preoperative pain levels tended to coincide with higher complexity. No significant trends were found.
Hernia sizes increased significantly as the complexity increased (p < 0.00001). Larger meshes are required to achieve durable repair for larger hernia sizes (p < 0.00001; see Table 3). The number of fixation points increased while the mesh-defect area ratio decreased (p < 0.00001) to achieve a GRIP value above CRIP. Additional OR time is required to perform durable repair for larger or more complex herniae (p < 0.00001).
HEDI was not necessary for less complex repairs. The HEDI output is related to abdominal wall instability. The distorsion field is calculated using a symmetric diffeomorphic registration method [8]. It was first applied in 2% of cases with a complexity score of 2, 6% in group 3, and 9% in group 4. In the most complex cases, one-third of cases were assessed using HEDI. However, since HEDI became available in 2020, the last year of recruitment for this report, this does not reflect the true need. Today, every complex case is evaluated with HEDI before elective repair. This is done to gain insight into biomechanical parameters [8].
In the highest-complexity group, 94% of patients underwent transversus abdominis release augmented with a DIS class A mesh with non-resorbable suture fixation. Furthermore, half of the patients underwent a single crown tack fixation using absorbable tacks. In addition, 44% had a second mesh in the intraperitoneal underlay repair (IPUM as a sandwich, usually with a biosynthetic Phasix® mesh). To counteract a jump of tissue compliance at fascial or bony edges, transmural fully absorbable pull-out sutures and Arthrex® bone anchors were used in 11% and 9% of cases. Area bonding with fibrin glue was used to dissipate the energy of cyclic loading in 6%. The patient with over 80% domain loss and tissue distension exceeding 10 cm was treated with progressive pneumoperitoneum. No botulinum toxin or Fasciotens® was necessary in any case. The calculated GRIP increased from no complexity to complexity level 4 (p = 0.00203) and remained constant thereafter because the GRIP coefficients of these combined procedures for complexity class 5 cases have not yet been determined. Surgical access was open for retromuscular, TAR, and sandwich repair in 82%, MILOS in 11%, and laparoscopic eTAR in 7% of all cases. No robotic procedures were performed in this study. The increase in operation time reflects the increasing complexity of the surgical requirements.
Patients with increasingly complex abdominal wall repairs required a longer hospital stay (p = 0.00031, Table 4). There was a tendency for more intra- and postoperative complications with increasing complexity. The rate of reoperations remained constant. Pain at discharge was comparable in all groups and diminished thereafter (Table 5). At the 3-year follow-up, only one patient occasionally took an analgesic, while 189 patients did not take any. All patients under the age of 62 were able to return to work after 14 weeks of rehabilitation. Some of these patients had been on and off work for up to 20 years prior to BCR.
Discussion
In an open prospective observational registry trial, we studied the effectiveness of biomechanically calculated abdominal wall reconstructions for incisional hernias of varying complexity. This report expands previous knowledge on biomechanical stability of herniated abdominal walls on a larger patient base [3, 10]. Our study provides insight into complexity-related biomechanical aspects of incisional hernia repair. Our results are positive.
The human abdominal wall consists of different layers of polymers, including the aponeurosis, fascia, and musculature [11]. BCR repairs a defect with a DIS class A textile [3]. Similar to engineering and materials science, cyclic loading is crucial to test the behavior of structural composite. It refers to the application of repeated or fluctuating stresses, strains or stress intensities at specific locations on structural elements. In complex incisional hernia repair as well as in aerospace, automotive, civil engineering, and orthopedics, cyclic loading can cause degradation over time [12].
To develop BCR, two new technologies were necessary [3, 9, 15].
Complex surgeries result in longer surgery times and hospital stays. They require better materials, ultimately resulting in more investment. However, the investment is balanced by the benefit of doing the correct repair the first time around. BCR can help achieve this. Additionally, pain, which increases with complexity, decreases after a biomechanically calculated repair.
Conclusions
Preoperative calculations of biomechanical stability can guide the surgical design of complex hernia repair. Complexity can be scored related to biomechanics. Durable repairs require materials and OR time that are significantly related to increasing complexity of incisional hernia. Complex incisional hernia can be repaired at very low recurrence and chronic pain rates considering biomechanical and cyclic loading principles. Randomized trials are needed to confirm the advances possible with BCR, as this study provides the first promising long-term results.
Data availability
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation considering restrictions by national and European data protection laws. All data supporting the findings of this study are available within the paper.
Abbreviations
- BCR:
-
Biomechanically calculated reconstruction
- CRIP:
-
Critical resistance to impacts related to pressure
- GRIP:
-
Gained resistance to impacts related to pressure
- BMI:
-
Body mass index
- NAS:
-
Numerical-analog scale
- MDAR:
-
Mesh-to-defect-area-ratio
- HEDI:
-
Hernia evaluation, detection and imaging
- AI:
-
Artificial intelligence
- MILOS:
-
Mini- or less-open sublay operation
- OR:
-
Operation room
- DIS:
-
Dynamic intermittent strain
- IPUM:
-
Intraperitoneal underlay mesh
- CT:
-
Computed tomography
- CEDAR:
-
Carolina estimate of disease adjusted risk
- HbA1c:
-
Glycosylated hemoglobin type A1c
- CTAV:
-
CT abdomen at rest and during a Valsalva maneuver
References
Deerenberg EB, Henriksen NA, Antoniou GA, Antoniou SA, Bramer WM, Fischer JP, Fortelny RH, Gök H, Harris HW, Hope W, Horne CM, Jensen TK, Köckerling F, Kretschmer A, López-Cano M, Malcher F, Shao JM, Slieker JC, de Smet GHJ, Stabilini C, Torkington J, Muysoms FE (2022) Updated guideline for closure of abdominal wall incisions from the European and American Hernia Societies. Br J Surg 109:1239–1250. https://doi.org/10.1093/bjs/znac302
Hoffmann H, Köckerling F, Adolf D, Mayer F, Weyhe D, Reinpold W, Fortelny R, Kirchhoff P (2021) Analysis of 4,015 recurrent incisional hernia repairs from the Herniamed registry: risk factors and outcomes. Hernia 25:61–75. https://doi.org/10.1007/s10029-020-02263-x
Lesch C, Nessel R, Adolf D, Hukauf M, Köckerling F, Kallinowski F, STRONGHOLD, Herniamed-Collaborators GROUP; Willms A, Schwab R, Zarras K, (2024) STRONGHOLD first-year results of biomechanically calculated abdominal wall repair: a propensity score matching. Hernia 28:63–73. https://doi.org/10.1007/s10029-023-02897-7
Kallinowski F, Ludwig Y, Löffler T, Vollmer M, Lösel PD, Voß S, Görich J, Heuveline V, Nessel R (2021) Biomechanics applied to incisional hernia repair - Considering the critical and the gained resistance towards impacts related to pressure. Clin Biomech (Bristol, Avon) 82:105253. https://doi.org/10.1016/j.clinbiomech.2020.105253
Nessel R, Löffler T, Rinn J, Lösel P, Voss S, Heuveline V, Vollmer M, Görich J, Ludwig YM, Al-Hileh L, Kallinowski F (2021) Primary and recurrent repair of incisional hernia based on biomechanical considerations to avoid mesh-related complications. Front Surg 8:764470. https://doi.org/10.3389/fsurg.2021.764470
Herniamed Qualitätssicherungsstudie. Datenschutzrechtliche Aufklärung und Einwilligung inkl. Information gem. Art.13 DS-GVO und Information über die wesentlichen Inhalte der Vereinbarung über die gemeinsame Verantwortlichkeit nach Art. 26 Abs. 2 S.2 der DS-GVO (2022). Available at https://www.herniamed.de/sites/default/files/Einwilligungserklaerung.pdf
Kallinowski F, Nessel R, Gorich J, Grimm A, Loffler T (2020) CT Abdomen with Valsalva’s maneuver facilitates grip-based incisional hernia repair. J Abdom Wall Reconstr. 2:1006
Relle JJ, Voß S, Raschidi R, Nessel R, Görich J, Wielpütz MO, Löffler T, Heuveline V, Kallinowski F, Lösel PD (2023) HEDI: First-Time Clinical Application and Results of a Biomechanical Evaluation and Visualisation Tool for Incisional Hernia Repair. Preprint at ar**v.2307.01502
Kallinowski F, Harder F, Gutjahr D, Raschidi R, Silva TG, Vollmer M, Nessel R (2018) Assessing the GRIP of ventral hernia repair: How to securely fasten dis classified meshes. Front Surg 4:78. https://doi.org/10.3389/fsurg.2017.00078
Deeken CR, Lake SP (2017) Mechanical properties of the abdominal wall and biomaterials utilized for hernia repair. J Mech Behav Biomed Mater 74:411–427. https://doi.org/10.1016/j.jmbbm.2017.05.008
Karrech A, Ahmad H, Hamdorf JM (2023) Biomechanical stability of hernia-damaged abdominal walls. Sci Rep 13:4936. https://doi.org/10.1038/s41598-023-31674-w
Kallinowski F, Ludwig Y, Gutjahr D, Gerhard C, Schulte-Hörmann H, Krimmel L, Lesch C, Uhr K, Lösel P, Voß S, Heuveline V, Vollmer M, Görich J, Nessel R (2021) Biomechanical influences on mesh-related complications in incisional hernia repair. Front Surg 8:763957. https://doi.org/10.3389/fsurg.2021.763957
Münster S, Jawerth LM, Leslie BA, Weitz JI, Fabry B, Weitz DA (2013) Strain history dependence of the nonlinear stress response of fibrin and collagen networks. Proc Natl Acad Sci USA 110:12197–12202. https://doi.org/10.1073/pnas.1222787110
Ristaniemi A, Torniainen J, Stenroth L, Finnilä MAJ, Paakkonen T, Töyräs J, Korhonen RK (2020) Comparison of water, hydroxyproline, uronic acid and elastin contents of bovine knee ligaments and patellar tendon and their relationships with biomechanical properties. J Mech Behav Biomed Mater 104:103639. https://doi.org/10.1016/j.jmbbm.2020.103639
Nessel R, Lesch C, Vollmer M, Kallinowsk F (2023) Biomechanical principles of a permanently durable abdominal wall reconstruction: current status and potential future development. Mini-invasive Surg 7:21. https://doi.org/10.20517/2574-1225.2023.21
Chittajallu SNSH, Richhariya A, Tse KM, Chinthapenta V (2022) A Review on damage and rupture modelling for soft tissues. Bioengineering 9:26. https://doi.org/10.3390/bioengineering9010026
Aly OE (2023) Addressing parastomal herniation through biomechanical simulation. Hernia 27:565–573. https://doi.org/10.1007/s10029-022-02704-9
Roth JS, Anthone GJ, Selzer DJ, Poulose BK, Bittner JG, Hope WW, Dunn RM, Martindale RG, Goldblatt MI, Earle DB, Romanelli JR, Mancini GJ, Greenberg JA, Linn JG, Parra-Davila E, Sandler BJ, Deeken CR, Voeller GR (2018) Prospective evaluation of poly-4-hydroxybutyrate mesh in CDC class I/high-risk ventral and incisional hernia repair: 18-month follow-up. Surg Endosc 32:1929–1936. https://doi.org/10.1007/s00464-017-5886-1
Petersson P, Montgomery A, Petersson U (2020) Modified peritoneal flap hernioplasty versus retromuscular technique for incisional hernia repair: a retrospective Cohort study. Scand J Surg 109:279–288. https://doi.org/10.1177/1457496919863943
Katzen M, Ayuso SA, Sacco J, Ku D, Scarola GT, Kercher KW, Colavita PD, Augenstein VA, Heniford BT (2023) Outcomes of biologic versus synthetic mesh in CDC class 3 and 4 open abdominal wall reconstruction. Surg Endosc 37:3073–3083. https://doi.org/10.1007/s00464-022-09486-2
Saul D, Menger MM, Ehnert S, Nüssler AK, Histing T, Laschke MW (2023) Bone healing gone wrong: pathological fracture healing and non-unions-overview of basic and clinical aspects and systematic review of risk factors. Bioengineering (Basel) 10:85. https://doi.org/10.3390/bioengineering10010085
Kallinowski F (2022) Biomechanics of mesh repair of the herniated abdominal wall: requires some knowledge of stochastic processes. https://websurg.com/doi/lt03en24558. Accessed 16 Mar 2022
Franz MG (2008) The biology of hernia formation. Surg Clin North Am 88(1–15):vii. https://doi.org/10.1016/j.suc.2007.10.007
Köckerling F, Koch A, Lorenz R, Schug-Pass C, Stechemesser B, Reinpold W (2015) How long do we need to follow-up our hernia patients to find the real recurrence rate? Front Surg 2:24. https://doi.org/10.3389/fsurg.2015.00024
Zamkowski M, Tomaszewska A, Lubowiecka I, Śmietański M (2023) Biomechanical causes for failure of the Physiomesh/Securestrap system. Sci Rep 13: 17504. https/doi.org/https://doi.org/10.1038/s41598-023-44940-8
Acknowledgements
We are grateful for the cooperation with Dr. Philipp Lösel, Department of Materials Physics at the Australian National University, and Jacob Relle, M.Sc., Engineering Mathematics and Computing Lab (EMCL), Interdisciplinary Center for Scientific Computing (IWR), Heidelberg University, for the HEDI project. We cordially thank Cristina Debellis, Personal Secretarial Assistant to the Surgical Directorate, for consistently following the patients with great enthusiasm and dedicated care who now eagerly performs the five-year recalls.
Funding
Open Access funding enabled and organized by Projekt DEAL. Heidelberger Stiftung Chirurgie grants No. 2016/22, 2017/171, 2018/215, 2019/288, 2020/376 and 2021/444
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The studies for computed tomography at rest and during Valsalva maneuver were reviewed and approved by the Ethics Committee of the Heidelberg University vote S-522/2020. STRONGHOLD as part of the HERNIAMED registry complies with the Declaration of Consent of the HERNIAMED database [amedHernie; 6]. The Herniamed Registry has ethical approval (BASEC Nr. 2016-00123, 287/2017BO2/F-2022-111). The patients/participants provided their written informed consent to participate in the respective study in accordance with the national legislation and the institutional requirements.
Informed consent
The patients/participants provided their written informed consent to participate in the respective study in accordance with the national legislation and the institutional requirements.
Conflict of interests
The institution of FK recieved honoraria for lectures or educational events from Medtronic® and Becton Dickinson®, support for attending meetings by Becton Dickinson® and Dahlhausen® and receipt of equipment and materials from Dahlhausen® and Corza® medical, Germany. The other authors have no conflict of interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Topical Collection on Complex Incisional Hernia.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nessel, R., Löffler, T., Rinn, J. et al. Three-year follow-up of the grip concept: an open, prospective, observational registry study on biomechanically calculated abdominal wall repair for complex incisional hernias. Hernia (2024). https://doi.org/10.1007/s10029-024-03064-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10029-024-03064-2