Abstract
Purpose
Synthetic prosthetic materials that are fully absorbable seek to reduce the host foreign body reaction and promote host tissue regeneration. This preclinical trial was designed to analyse, in the long term, the behaviour of two prosthetic meshes, one synthetic and one composed of porcine collagen, in abdominal wall reconstruction.
Methods
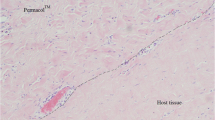
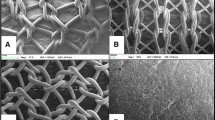
Partial defects were created in the abdominal walls of New Zealand rabbits and repaired using a synthetic absorbable mesh (Phasix™) or a non-crosslinked collagen bioprosthesis (Protexa™). After 3, 6, 12 and 18 months, specimens were recovered for light microscopy and collagen expression analysis to examine new host tissue incorporation, macrophage response and biomechanical strength.
Results
Both materials showed good host tissue incorporation in line with their spatial structure. At 18 months postimplant, Protexa™ was highly reabsorbed while the biodegradation of Phasix™ was still incomplete. Collagenization of both materials was good. Macrophage counts steadily decreased over time in response to Phasix™, yet persisted in the collagen meshes. At 18 months, zones of loose tissue were observed at the implant site in the absence of herniation in both implant types. The stress–stretch behaviour of Phasix™ implants decreased over time, being more pronounced during the period of 12–18 months. Nevertheless, the abdominal wall repaired with Protexa™ became stiffer over time.
Conclusion
Eighteen months after the implant both materials showed good compatibility but the biodegradation of Phasix™ and Protexa™ was incomplete. No signs of hernia were observed at 18 months with the stress–stretch relations being similar for both implants, regardless of the more compliant abdominal wall repaired with Protexa™ at short term.










Similar content being viewed by others
References
Kigsnorth A, LeBlanc K (2003) Hernias: inguinal and incisional. Lancet 362:1561–1571
Read RC (2004) Milestones in the history of hernia surgery: prosthetic repair. Hernia 8:8–14
Klosterhalfen B, Klinge U (2013) Retrieval study at 623 human mesh explants made of polypropylene- impact of mesh class and indication for mesh removal on tissue reaction. J Biomed Mater Res B Appl Biomater 101:1393–1399
Lichtenstein IL, Shulman AG, Amid PK (1990) Use of mesh to prevent recurrence of hernias. Postgrad Med 87:155–158
Luijendijk RW, Hop WC et al (2000) A comparison of suture repair with mesh repair for incisional hernia. N Eng J Med 343:392–398
Cobb WS, Burns JM, Peindl RD, Carbonell AM, Matthews BD (2006) Textile analysis of heavy-weight, mid-weight and light-weight polypropylene mesh in a porcine ventral hernia model. J Surg Res 136:1–7
Badylak SF (2007) The extracellular matrix as biologic matrix as a biologic scaffold material. Biomaterials 28:3587–3593
Bellows CF, Smith A, Malsbury HWS (2013) Repair of incisional hernias with biological prosthesis: a systematic review of current evidence. Am J Surg 205:85–101
Liang HC, Chang Y, Hsu CK, Lee MH, Sung HW (2004) Effects of crosslinking degree an acellular biological tissue on its tissue regeneration pattern. Biomaterials 25:3541–3552
De Castro-Bras LE, Shurey S, Sibbons PD (2012) Evaluation of crosslinked and non-crosslinked biologic prostheses for abdominal hernia repair. Hernia 16:77–89
Deeken CR, Eliason BJ, Picher MD, Grant SA, Frisella MM, Mattews BD (2012) Differentiation of biologic scaffold materials through physicomechanical, thermal, and enzymatic degradation techniques. Ann Surg 255:595–604
Smart NJ, Bloor S (2012) Durability of biologic implants for use in hernia repair: a review. Surg Innov 19:221–229
GORE BIO-A product brochure (2011) Available from: https://www.goremedical.com/resources/dam/assets/AQ3037-EN2.pdf
TIGR® Matrix: long-term resorbable mesh. Novus world (2018) Available from: https://novusscientific.com/us/products/tigr-matrix/
Bard Davol. Phasix TM mesh fully resorbable scaffold for hernia repair (2016) Available from: https://www.crbard.com/davol/en-US/products/Phasix-Mesh.
Pascual G, Sotomayor S, Rodríguez M, Pérez-Khöler B, Bellón JM (2012) Repair of abdominal wall defects with biodegradable laminar prostheses: polymeric or biological? PLoS One 7:e52628
Symeonidis D, Efthimiou M, Koukoulis G, Athanasiou E, Mamaloudis I, Tzovaras G (2013) Open inguinal hernia repair with the use of polyglycolic acid/trimethylene carbonate absorbable mesh: a critical update of the long-term results. Hernia 17:85–87
Hjort H, Mathisen T, Alves A, Clermont G, Boutrand JP (2012) Three-year results form a preclinical implantation study of a long-term resorbable surgical mesh with time-dependent mechanical characteristics. Hernia 16:191–197
Ruiz-Jasbon F, Norrby J, Ivarsson ML, Bjork S (2014) Inguinal hernia repair using a synthetic long-term resorbable mesh: results from a 3-year prospective safety and performance study. Hernia 18:723–730
Kilkenny C, Browne WJ, Cuthill IC, Emerson M, Altman DG (2010) Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. PLoS Biol 29:e1000412
Pascual G, Pérez-Khöler B, Rodríguez M, Sotomayor S, Bellón JM (2014) Postimplantation host tissue response and biodegradation of biologic versus polymer meshes implanted in an intraperitoneal position. Surg Endosc 28:559–569
Abdelfatah MM, Rostambeigi N, Podgaetz E, Sarr MG (2015) Long-term outcomes (%3e5-year follow-up) with porcine acellular dermal matrix (Permacol™) in incisional hernias at risk for infection. Hernia 19:135–140
Carbonell AM, Criss CN, Cobb WS, Novitsky YW, Rosen MJ (2013) Outcomes of synthetic mesh in contaminated ventral hernia repairs. J Am Coll Surg 21:991–998
Martin DP, Williams SF (2003) Medical applications of poly-4-hydroxybutyrate: a strong flexible absorbable biomaterial. Bioch Eng J 16:97–105
Adams WP Jr, Moses AC (2017) Use of poly-hydroxybutyrate mesh to optimize soft-tissue support in mastopexy: a single-study. Plast Reconstr Surg 139:67–75
Williams SF, Rizk S, Martin DP (2013) Poly-4-hydroxybutyrate (P4HB): a new generation of resorbable medical devices for tissue repair and regeneration. Biomed Tech (Berl) 58:439–452
Miserez M, Jairam AP, Boersema GSA, Bayon Y, Jeekel J, Lange JF (2019) Resorbable synthetic meshes for abdominal wall defects in preclinical setting: a literature review. J Surg Res 237:67–75
Bellón JM, Rodríguez M, Pérez-Khöler B, Pérez-López P, Pascual G (2017) The New Zealand white rabbit as a model preclinical studies addressing tissue repair at the level of the abdominal wall. Tissue Eng Part C Methods 23:863–880
Martin DP, Badhwar A, Shah DV, Rizk S, Eldridge SN, Gagne DH, Ganatra A, Darois RE, Williams SF, Tai HC, Scott JR (2013) Characterization of poly-4-hydroxybutyrate mesh for hernia repair applications. J Surg Res 184:766–773
Mulier KE, Nguyen AH, Delaney JP, Marquez S (2011) Comparison of Permacol™ and Strattice™ for the repair of abdominal wall defects. Hernia 15:315–319
Gupta A, Zahriya K, Mullens PL, Salmassi S, Keshishian A (2006) Ventral herniorraphy: experience with two different biosynthetic mesh materials. Hernia 10:419–425
Bellón JM, Buján J, Contreras L, Hernando A (1995) Integration of biomaterials implanted into abdominal wall: process of scar formation and macrophage response. Biomaterials 16:381–387
Deeken CR, Matthews BD (2013) Characterization of the mechanical strength, resorption properties, and histologic characteristics of a fully absorbable material Poly-4-hydroxybutyrate-PHASIX mesh in a porcine model of hernia repair. ISRN Surg 181:160–169
Catalán V, Peña MJ, Sáez P, García G, Cabeza JJ, Anula R, Torres AJ (2019) Estudio histológico de la prótesis biosintética de poli-4hidroxibutirato (Phasix™) en el humano y revisión de la literatura. Rev Hispanoam Hernia 7:66–71
Peeters E, Van Barneveld KWY, Schreinemacher MH, De Hertogh F, Ozog Y, Bouvy N, Miserez M (2013) One-year outcome of biological and synthetic bioabsorbable meshes for augmentation of large abdominal wall defects in a rabbit model. J Surg Res 180:274–283
Bellón JM, Buján J, Contreras L, Hernando A, Jurado F (1994) Macrophage response to experimental implantation of polypropylene prostheses. Eur Surg Res 26:46–53
Plymale MA, Davenport DL, Dugan A, Zachem A, Roth JS (2018) Ventral hernia repair with poly-4-hydroxybutyrate mesh. Surg Endosc 32:1689–1694
Roth JS, Anthone GJ, Selzer DJ, Poulose BK, Bittner JG, Hope WW, Dunn RM, Martindale RG, Goldblatt MI, Earle DB, Romanelli JR, Mancini GJ, Greenberg JA, Linn JG, Parra-Davila E, Sandler BJ, Deeken CR, Voeller GR (2018) Prospective evaluation of poly-4-hydroxybutyrate mesh in CDC class I/high-risk ventral and incisional hernia repair: 18-month follow-up. Surg Endosc 32:1929–1936
Montori G, Coccolini F, Manfredi R, Ceresoli M, Campanati L, Magnone S, Pisano M, Poiasina E, Nita G, Catena F, Ansaloni L (2015) One year experience of swine dermal non-crosslinked collagen prostheses for abdominal wall repairs in elective and emergency surgery. World J Emerg Surg 10:28
Acknowledgements
The study was supported by Grant “SAF2017-89481-P” from the Spanish Ministry of Economy and Competitiveness.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no conflicts of interest to disclose.
Ethical approval
The study protocol was approved by the Committee on the Ethics of Animal Experiments of the Universidad de Alcalá, Madrid, Spain.The study protocol was approved by the Committee on the Ethics of Animal Experiments of the Universidad de Alcalá, Madrid, Spain.
Human and animal rights
The up-keep and handling of animals throughout the study was in accordance with the Guide for the Care and Use of Laboratory Animals of the National and European Institutes of Health (Spanish Law 6/2013, Spanish Royal Decree 53/2013, European Directive 2010/63/UE and European Convention of the Council of Europe ETS123). All procedures were performed at the Animal Research Centre of the Universidad de Alcalá (Madrid, Spain), which is registered with the Directorate General for Agriculture of the Ministry of Economy and Technology Innovation of the Community of Madrid (ES280050001165) ensuring all facilities legally cover the needs and requirements of the research.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pascual, G., Rodríguez, M., Pérez-Köhler, B. et al. Long term comparative evaluation of two types of absorbable meshes in partial abdominal wall defects: an experimental study in rabbits. Hernia 24, 1159–1173 (2020). https://doi.org/10.1007/s10029-020-02201-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-020-02201-x