Abstract
Peste des petits ruminants (PPR) is a highly contagious, economically important viral disease of small ruminants, targeted for global eradication by the year 2030. The recent geographic surge in PPR virus distribution, economic implications, the success of the rinderpest eradication campaign, and ongoing national/regional efforts convinced the FAO and OIE to initiate a global PPR control and eradication strategy. Since its discovery, a series of diagnostic tools have been developed for detecting PPR virus and virus-specific antibodies. Furthermore, it is understood that diagnostic and vaccine-monitoring tools are inevitable components of the four-stage strategy of global PPR eradication from assessment to the post-eradication phase. However, these tools may not be suitable for all stages of PPR control and eradication. For instance, diagnostics such as ELISA could be used for mass screening of clinical and serum samples, whereas immunochromatographic tests can be used at the field level as a pen-side test. Yet, assays with higher sensitivity, such as RT-PCR, RT-PCR ELISA, real-time RT-PCR and LAMP are important for early diagnosis of PPR and also, theoretically, during the late stages of eradication or when sampling non-natural hosts. Moreover, during the later stages of any control program, suspected/doubtful outbreaks will have to be reconfirmed using multiple laboratory tests. Hence, diagnostics can and should be efficiently applied at different stages of the PPR control and eradication campaign based on available resources and the number of samples to be tested. This article provides an overview of the various PPR diagnostic tools and suggests where and how they should be logically applied during the different phases of global PPR control and eradication.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Peste des petits ruminants (PPR) is primarily a disease of sheep and goats; however, it may also infect cattle, buffalo, pigs and wild animal species [1, 2]. The disease in small ruminants is characterized by pyrexia, necrotic stomatitis, pneumonia and enteritis. In cattle and pigs, PPR virus (PPRV) causes an apparently asymptomatic infection, whereas in wild animals such as gazelle, ibex, gemsbok, deer, bushbuck and wild goat, the disease severity varies from asymptomatic to severe clinical signs [3]. PPRV can cause up to 100 % morbidity and significant mortality amongst sheep and goats. Importantly, small ruminants are often reared by poorer farmers; therefore, PPR is a considerable threat to livelihood and food security in large parts of Africa, the Middle East and Asia. This region is also home to approximately 80 % of world’s sheep and goat population [4]. In addition, PPR also has indirect effects on the economies of endemically infected countries such as vaccination costs, sanitary measures and control measures. Altogether, PPR is estimated to cause global economic losses of US$ 1.5 to 2 billion every year [4].
PPRV is known to have four lineages (I, II, III, and IV) with, until recently, geographically defined distributions. Lineages I to III were common in Africa, and IV in the Middle East and Asia [5]. However, during the past decade, realignment in lineage distribution of PPRV has been observed, wherein lineage IV has spread into Africa [6]. In addition, the spread of PPRV has extended beyond Africa, the Middle East and Asia into Europe [7, 8]. Of note, this altered lineage distribution might not pose a problem for diagnosis and control, since there is only one serotype of PPRV. However, the occurrence of PPR in previously uninfected geographical areas, together with the replacement of lineages in endemically infected countries, highlights the dynamic and transboundary nature of this disease [6, 8].
Uncontrolled animal movement between PPR-prevalent countries and porous borders between neighbouring endemic countries makes disease control a global priority. Since PPR is a priority disease for livelihood security, it was included in the Global Framework for the progressive control of Transboundary Animal Diseases (GF-TADs), an initiative of the World Organization for Animal Health (OIE) and the Food and Agriculture Organization (FAO) of the United Nations. Based on the recommendations of a GF-TADs Global Steering Committee held in Paris in October 2012, the PPR GF-TADs working group was established to formulate a “global strategy” for PPR eradication, aiming for global eradication by the year 2030 [4]. The technical cornerstones of the global PPR eradication strategy are i) diagnostics, ii) surveillance, iii) prevention and control, iv) develo** a legal framework including veterinary services, and v) stakeholder involvement [4]. It is estimated that an investment of US$ 7.1 billion on Global PPR eradication could be recovered within 5 years of successful eradication (http://www.oie.int/eng/PPR2015/doc/PPR-Advocacy-EN.pdf). The FAO and OIE’s international conference for the control and eradication of peste des petits ruminants was held at Abidjan, Côte d’Ivoire, from 31 March to 2 April 2015. The conference participants noted with interest that other approaches to costing the eradication campaign might also be needed and recommended that an expert meeting be held to discuss the cost of the strategy including ensuring cost effectiveness of veterinary services, compliance with OIE standards on quality, prevention and control of other diseases of small ruminants [4].
For PPR control, cell culture attenuated vaccine strains such as “PPRV-Nigeria75/1”, “PPRV-Sungri/96”, and other strains are available for sheep and goats [9]. Among them, “PPRV-Nigeria75/1” is commonly used in Africa, the Middle East, and parts of Asia, whilst “PPRV-Sungri/96” is used in India and some of the countries in the Middle East and South Asia [2, 10–12]. These vaccines have established efficacy and protect sheep and goats life-long against disease [13]. However, they do not facilitate differentiation of infected and vaccinated animals (DIVA). Development of these marker vaccines, accompanied by DIVA-enabled diagnostic tests for PPR, would represent an excellent tool during the final phases of PPR eradication. Such efforts are in progress within various PPR-research groups, but their successful application in the field has yet to be properly determined [14, 15].
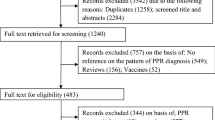
Diagnostic assays are very important tools to verify the impact of PPR control and eradication [12]. A number of diagnostic assays have been developed for the diagnosis of PPR by targeting virus and virus-specific antibodies [16, 17]. During clinical and serological surveys of disease, testing a large number of clinical samples is a necessary endeavour [4]. The main criteria for diagnostic assays during a control and eradication campaign are high sensitivity, specificity, early detection ability, rapidity in diagnosis, and suitability for large-scale applications. Tests such as immunocapture/sandwich-ELISA, competitive-ELISA, immunochromatographic techniques, and RT-PCR can be efficiently applied on very large sample sizes for routine diagnosis of PPR [18–22]. However, during the later stages of PPR eradication, critical screening of suspected samples from PPR-like diseases as well as samples from wild animals might require the use of highly sensitive, multiple diagnostic tools. Under these situations, sensitive and reliable diagnostics such as RT-PCR-ELISA [23] could also be applied, in spite of the expenses and time involved.
There is already an extensive literature on PPR vaccines and their application for immunization against PPR [9, 13]. However, to our knowledge, a comprehensive overview of PPR diagnostics and their advancement and application is not available. Therefore, this review was prepared to provide a summary of PPR diagnostics and diagnosis in light of the OIE-FAO global control and eradication campaign and its 2030 target.
Differential diagnosis
Confirmatory diagnosis of PPR under field conditions is not always possible due to the prevalence of PPR-like diseases and the frequent occurrence of PPR as a mixed infection in sheep and goats. The common clinical manifestations of PPR in sheep and goats are pyrexia, oculo-nasal discharges, erosive stomatitis (involving the lips, tongue and gums), anorexia, diarrhea, and dehydration, followed by either recovery or death [6]. Further, secondary infections result in a change in the clinical picture of the original disease. This again complicates differential diagnosis based on clinical signs typical of PPR. Therefore, other diseases of small ruminants causing PPR-like signs can cause problems in clinical diagnosis [24, 25]. Important diagnostic differences include the following: i) foot and mouth disease (FMD can be excluded by signs of lameness, ii) bluetongue does not cause diarrhea, iii) capripox can be differentiated by pock lesions, iv) contagious ecthyma would lack necrotic stomatitis, and v) pneumonic pasteurellosis and vi) caprine pleuropneumonia are characterized by respiratory illness alone (ftp://ftp.fao.org/docrep/FAO/003/X1703E/X1703E00.PDF). However, differential diagnosis may not always be possible, because at times, PPR-infected animals might not present all of the clinical signs. As a result, laboratory confirmation of PPR is necessary for definitive diagnosis and assessment of the epidemiological status of a country. Similarly, the use of antibody detection techniques is necessary for sero-surveillance and broader impact assessments of vaccination campaigns. Since, the first PPR report in 1942, a series of diagnostic assays have been developed and introduced (Fig. 1 and Table 1) for the detection of PPRV and virus-specific antibody. A simple categorization of these diagnostics based on the specific molecular target for detection is shown in Fig. 2. A more detailed discussion of these diagnostics is presented below.
PPR virus detection
Direct virus isolation and immunological methods are the commonly used virus-detection techniques for the diagnosis of PPR. These assays, especially virus isolation, demand proper collection of samples at appropriate stages of disease to ensure quality clinical samples. Clinical specimens such as ocular, nasal, oral and rectal swabs, and lymphoid tissues exhibiting lesions (i.e., mesenteric, bronchial lymph nodes and spleen) from animals are collected in phosphate-buffered saline (pH 7.2-7.4). For virus isolation, ocular and nasal swabs as well as blood in EDTA/heparin collected at early stages of disease are the samples of choice [26]. The cold chain for these samples must be maintained during transit to a diagnostic laboratory to ensure robust and reliable detection of the virus.
Virus isolation
Virus isolation is a gold standard test for PPR diagnosis, wherein primary goat/sheep kidney cells, Vero cells [27], or marmoset B-lymphoblastoid (B95a) cell lines [28] can be employed. Despite the high sensitivity of primary cell cultures for virus isolation, they are not commonly used due to the risks of contamination, batch-to-batch variation and animal ethics issues. Although B95a cells are more sensitive to PPRV infection and support virus replication to a high titre, the Vero cell line is commonly used for virus isolation from clinical samples and for infectivity assays [28–31]. Normally, during virus isolation in Vero cells, several sequential blind passages are required before an appreciable cytopathic effect (CPE) can be observed. PPRV-specific CPE is characterized by cell rounding and grape-like clustering, followed by fusion of cells and the formation of syncytia [28, 32]. Cell lines stably expressing the cellular receptors for PPRV, such as signalling lymphocyte activation molecule (SLAM)-expressing CV-1, Vero and B95a cells can obviate blind passages [33] and therefore enhance the success rate of virus isolation. However, in general, virus isolation is time consuming, requires cell culture facilities, and is relatively cumbersome to perform as a routine technique.
Conventional immunological methods
Unlike virus isolation, PPRV detection by immunological methods does not require live virus in the clinical samples. During the 1980s, when both rinderpest and PPR diseases were present, popular techniques like agar gel immunodiffusion (AGID) and counter immunoelectrophoresis (CIE) were used for laboratory diagnosis. In AGID, soluble antigens and antibodies diffuse passively in the agar medium, but in CIE, the antigen and antibody move in opposite direction in the electric field to form the line of precipitation at the point of interaction. Due to the presence of cross-reacting epitopes in both PPRV and rinderpest virus, AGID and CIE could not differentiate the two viruses. AGID is a simple test applied for PPR diagnosis from swabs and tissues of infected animals that is performed using PPRV-specific antibodies [34]. Simultaneously, the comparatively quick and relatively sensitive CIE was also developed [34, 35]. These tests are less sensitive at the early stages of infection and with mild forms of the disease. Hence, efforts were made to replace them with assays that are more sensitive and specific, such as ELISA, immunochromatographic tests and nucleic-acid-based tests.
Immunohistochemistry techniques were used to detect PPRV antigen in tissues. Monoclonal antibody (MAb)-based fluorescent antibody test (FAT) was developed to detect antigen from conjunctival smears. FAT has higher sensitivity than simple staining of conjunctival smears with 10 % Giemsa stain, a method for visualizing syncytial cells [36]. Although FAT is simple and quick to perform, it requires a fluorescent microscope and technical expertise. Therefore, a similar assay, namely the immunoperoxidase test (IPT), was developed that required only a light microscope and available was even to resource-poor laboratories [37].
Alternatively, the haemagglutination property of the “H” protein of PPRV [38] was explored to develop haemagglutination (HA) tests using human blood group “O” and chicken red blood cells (RBCs) for the detection of PPRV antigen from clinical specimens [39, 40]. The HA test is simple to perform and does not need sterility nor sophisticated instruments [41]. These tests, even though they are not sensitive enough to detect early stages of disease and mild forms of disease, can be used to confirm CPE during virus infectivity titrations, similar to the cell-ELISA techniques [42, 43]. However, it is known that members of many families of animal viruses possess ability to agglutinate red blood cells. Hence, this test cannot be used as the sole diagnostic tool for the confirmation of field samples suspected of PPR.
Enzyme-linked immunosorbent assays (ELISAs)
ELISA employs an enzyme-substrate reaction for the detection of antigen-antibody interactions. These popular diagnostic tools are user-friendly with a desirable level of sensitivity and specificity. In addition, they are suitable for handling large sample sizes. Moreover, ELISA techniques enable better documentation and automation for evidence-based recording of the status of clinical samples. There are different formats of ELISA available based on sensitivity and specificity requirements. An immunocapture ELISA using MAbs raised against the nucleoprotein of PPRV and applied as capture and detection antibodies was developed at the World Reference Laboratory for PPR [21]. This ELISA has a diagnostic sensitivity of 100.6 TCID50 and is available as a commercial kit for PPRV antigen detection. Later, a sandwich ELISA was also developed in India using polyclonal sera for antigen capture and MAb (4G6) raised to the N protein of PPRV as a detection antibody [44]. This ELISA has 88.9 % relative diagnostic sensitivity and 92.8 % diagnostic specificity when compared to a commercial immunocapture ELISA kit [22]. Since the year 2002, the sandwich ELISA has been used for the routine diagnosis of PPR throughout India [11, 45]. Similarly, dot-ELISAs were described for PPRV antigen detection from clinical samples using anti-matrix protein and anti-nucleoprotein MAbs [46, 47]. Although the sensitivity of the dot-ELISAs is lower, they can be used as diagnostic tools in laboratories where resources are limited. Unfortunately, the dot-ELISA is prone to giving false-positive results; therefore, using known positive and negative specimens is advisable. In addition, an indirect ELISA, namely, cell-ELISA, for the detection of antigen in infected cells (in a microtitre plate format) was developed using the anti-nucleoprotein MAb 4G6 [43]. This assay has a relative sensitivity and specificity of more than 97 % when compared to virus the infectivity titrations scored by visual observation of CPE. During the determination of infectivity titre using cell culture, there might be ambiguity in the observation of CPE, especially at higher dilutions. Theoretically, this variation could be avoided through the use of the cell-ELISA technique. Further, it could be used as a vaccine quality control tool, as both infectivity assays and specific detection of PPRV can be performed simultaneously using this assay [43].
Immunochromatographic test
Advances in the field of application of nanotechnology for disease diagnosis have paved the way for the development of immunochromatographic tests for rapid diagnosis of PPR. These assays are simple, cost effective and easy to perform, and they give results within a matter of minutes. In addition, technical expertise is not required to carry out the test. This test detects antigen-antibody interactions on a nitrocellulose membrane (NCM) platform by trap** the unknown antigen/antibody with known antibody/antigen pre-spotted on the NCM. For PPRV antigen detection, this test was developed by employing an anti-H-protein MAb (C77) both as a capture antibody on the test line and also as the detection antibody [19, 48]. This test detects upwards of 103TCID50/mL of PPRV and has a relative sensitivity of 84 % and specificity of 95 % compared to RT-PCR. It also detects all four lineages of PPRV from different geographical origins. Currently, this lateral flow device kit, a promising tool for field-level diagnosis of PPR, is being manufactured by Foresite Diagnostics Ltd, Sand Hutton, York, UK [19]. Simultaneously, a lateral flow assay was also developed in competitive assay format using an anti-N protein MAb (4G6) and partially purified PPRV antigen with a detection limit of 104 TCID50 of PPRV per ml [49]. MAbs specific for the M protein (4H4), N protein (4G6) and H protein (4B11) of PPRV [44] were also employed for the development of an immunochromatographic test [50]. However, these assays have to be evaluated extensively using clinical samples, especially ocular and nasal swabs, which would be the samples of choice in the field. Although, these “pen-side” tests are less sensitive than immunocapture/sandwich ELISA and nucleic-acid-based diagnostics, their direct application on herds in the field effectively negates this issue. This is because even if only some animals are positive for PPR, the entire herd/flock would be classed as infected or at risk for disease, which remains the overarching aim of in-field surveillance.
For contagious diseases like PPR, if diagnosis is made at the field level, control measures could be adopted at early stage to prevent the spread of PPRV to neighbouring herds/flocks. Without these tests, transportation of samples to diagnostic laboratories and diagnosis can take a few days, by which time the virus might have already spread throughout the surrounding area. Moreover, effective transportation of clinical samples to diagnostic laboratories may be difficult in develo** and less-developed countries due to poor infrastructure.
PPRV nucleic-acid-based detection
Several nucleic-acid-based molecular tests have been developed for the specific diagnosis of PPR. PPRV has a single-stranded negative-sense RNA genome with six transcription units (N-P/C/V-M-F-H-L) encoding eight proteins (nucleoprotein, phosphoprotein, C protein, V protein, matrix, fusion, haemagglutinin and a large RNA dependent RNA polymerase) [51]. Nucleic-acid-based diagnostic techniques include hybridization, RT-PCR and its variants, PCR-ELISA and LAMP, etc. Even though these assays are very sensitive, they require a level of training in order to avoid generation of false positive results.
Nucleic acid hybridization
Initially, N-gene-based radioisotope-labelled cDNA probes were developed for the detection and differentiation of PPRV from rinderpest virus [53]. This tool was used for the detection of an outbreak of PPR in India in the year 1987 [52]. Although cDNA probes were sensitive and specific, the use of radioisotope (32P)-based probes was discontinued for regular diagnosis due to the short half-life and hazardous nature of this isotope [53]. Biotin- and digoxigenin-labelled probes were developed subsequently [54], but these had lower sensitivity. To overcome this, nucleic acid amplification techniques such as polymerase chain reaction (PCR) were developed for PPR diagnosis.
Reverse transcription PCR and its variants
Morbillivirus-specific RT-PCRs targeting the phosphoprotein (P) gene and fusion protein (F) gene were developed [55]. Subsequently, an RT-PCR targeting the 3’ end of the mRNA encoding the nucleoprotein (N) of PPRV was also developed. This is routinely being applied for research and clinical diagnosis of PPR with good sensitivity, partly because the N gene is transcribed more than other genes during viral replication [20, 56]. However, conventional RT-PCR assays may not necessarily be applicable (laborious and unaffordable) for routine clinical diagnosis in resource-poor laboratories, when the sample size is very large. Furthermore, these techniques are sensitive to cross-contamination (false-positives) often because of previous samples from collection, processing and testing. The diagnostic sensitivity of nucleic-acid-based tests in the field can also be affected by unforeseen variation in the primer binding site, RNA degradation, and PCR inhibitors in the sample, resulting in false negatives. As a result, diagnostic PCR must be performed with utmost care. False negatives in RT-PCR due to mutations in the primer-binding site can be avoided using multiplex PCR. In multiplex PCR, multiple primer pairs are used to amplify different but specific regions of genes. Two-step and single-step multiplex RT-PCRs targeting the N and M genes were developed for the detection and differentiation of PPRV and rinderpest virus [18, 57]. This multiplex RT-PCR has higher sensitivity than sandwich ELISA. In single-step assays, the reverse transcription and PCR steps are performed in the same micro-tube, thus minimizing the cross-contamination. Recently, a single-step multiplex RT-qPCR was developed for the detection and differentiation of respiratory diseases of small ruminants, namely, PPRV, capripoxvirus, Pasteurella multocida and Mycoplasma capricolum ssp. Capripneumoniae [58]. This test could be used for syndromic surveillance for the control of these diseases in sheep and goats.
SYBR Green and TaqMan probe-based real-time RT-PCR based on N [59–62] and M genes [63, 64] have also been developed for PPRV detection. Although real time RT-PCR assays are sensitive (low detection limit), they are not time- and cost-effective for routine diagnosis in develo** countries where the disease is mostly prevalent. Nevertheless, this test could be used for quantification of PPRV. The window for potential PPRV detection has been determined based on experimentally infected animal samples. The nucleic-acid-based assays, such as multiplex RT-PCR, SYBR Green–based real-time RT-PCR, and RT-PCR-ELISA have a window of detection of 7-15 days postinfection (dpi), 3-20 dpi, and 6-17 dpi, respectively [18, 23, 63, 64]. Although, virus shedding may vary between natural and experimental infections, these tests show high sensitivity (Table 1). These tests can add value through specific virus quantification or diagnosis of PPR during early and late phases of a disease outbreak when the virus load in clinical samples may be low and antigen detection techniques may not effectively detect the virus. Also, these highly sensitive tests would be useful for the confirmation of disease if other tests present unclear results.
PCR-ELISA
PCR-ELISA uses a combination of nucleic acid amplification and ELISA techniques for amplification and detection, respectively. In this assay, digoxigenin-labelled primers are used for nucleic acid amplification. Subsequently, biotinylated N-gene-specific probes are hybridized to these PCR amplicons and detected by ELISA [23, 65]. Hence, it can be used for the diagnosis of PPR during early and late phases of disease, when low viral loads mean sandwich ELISA [22] cannot always detect the infection. It is prone to cross-contamination of samples, like PCR assays, and is time-consuming, but it would be worthwhile to use it for samples that yield doubtful results in sandwich ELISA or other laboratory tests. The high sensitivity of this assay might be useful during the later phases of PPR eradication, when even a single case of PPR needs confirmation by multiple confirmatory tests. The test may also help to exclude PPR-like diseases and mixed infection of PPRV with other diseases.
A similar assay, RT-PCR (simple and aqueous phase) SNAP-ELISA for differentiation of rinderpest virus from PPRV was developed by targeting the F gene of PPRV [66]. In line with PCR-ELISA, this test also uses ELISA for the detection of PCR amplicons; therefore, it is easy to perform for large sample sizes. Such assays may be developed for specific diagnosis of PPR as well.
Loop-mediated isothermal amplification (LAMP)
The LAMP assay is an isothermal amplification technique that uses at least four primers for the amplification of a desired gene sequence. In contrast to PCR, LAMP uses Bst polymerase with strand displacement activity to enable denaturation during amplification [67]. The technique can be performed using a water bath, dry bath, heat block at isothermal conditions, and amplicons can be detected visually, either by change of colour or formation of precipitate, and also via conventional agarose gel electrophoresis. Being a simple, quick and sensitive technique, the LAMP assay has become a popular diagnostic platform for many viruses of veterinary importance [68, 69], including PPRV [70, 71]. LAMP assays have been developed for the diagnosis of PPR based on M and N genes of PPRV and has been shown in limited validation studies to have higher sensitivity than RT-PCR [70, 71]. These tests need to be evaluated extensively on various clinical samples and different lineages of PPRV globally. As the LAMP assay does not require a sophisticated thermocycler, it can be performed without much technical expertise and equipment. It could therefore be used for sensitive diagnosis of PPR even in less-well resourced laboratories [70, 71], i.e., in develo** countries where PPR is endemic. Moreover, the single-step LAMP assay minimizes the risk of sample cross-contamination and will be a promising tool in resource-poor laboratories [71].
Detection of PPRV antibodies
PPRV antigen and nucleic acid detection techniques can be used when sampling is performed during active outbreaks of disease, i.e., for diagnosis or clinical surveillance. However, many of these PPRV antigen and nucleic acid detection techniques can only be applied between 4 and 17 days postinfection. In addition, the quality of the sample needs to be transported carefully for antigen and genome detection. In contrast, antibodies elicited by PPRV, either during infection or after vaccination, can be detected for a much longer duration (at least three years after vaccination) [13]. Thus, antibody detection methods aid in monitoring of vaccination as well as sero-surveillance and sero-epidemiology to understand PPR disease status [11].
Conventional antibody detection assays
For antibody detection, the virus neutralization test (VNT) is considered the gold-standard, OIE-accepted diagnostic tool for international trade. In the VNT, 100 to 1000 TCID50 of PPRV is mixed with 100 µL of twofold dilutions of serum (de-complemented) and incubated at 37 °C prior to inoculation in cell culture in a 96-well microplate [72]. The development of a cytopathic effect (CPE) in wells containing a specific dilution of antibody indicate the absence of virus neutralization. The VN titre of a serum is expressed as the highest dilution that yields 50 % inhibition of CPE. This test detects virus-neutralizing antibody, which might be an indication of protection in vivo in the case of morbilliviruses. Due to the requirements for cell culture facilities and sterile serum, VNT is difficult to perform for routine sero-surveillance or sero-monitoring, especially where a large number of samples need to be screened. Thus, over a period of time, VNT has been replaced by competitive and blocking ELISA techniques. However, VNT is sometimes a good choice, e.g., when screening animals for experimental challenge studies, as the presence of a low antibody titre (1:4-16) in the serum may not always be reliably detected by competitive ELISA [73]. Occasionally, VNT can be used for disease diagnosis through the use of paired serum samples collected during the disease outbreak or the time when clinical signs are present and after 21 days of outbreak from the same animal. A significant four-fold increase in antibody titre is indicative of specific disease outbreak [73].
A haemagglutination inhibition (HI) test can also be used to quantify virus-neutralizing antibodies as an alternative to VNT. For performing HI, fresh RBCs are required, and the HA property of PPRV has been shown to vary in cell-culture-cultivated virus [42]. Similar to antigen detection, the CIE technique has been developed for the detection of antibodies from infected animals [74]. Although both of these simple to perform tests, HI and CIE, could be used in less-well-resourced laboratories, they are not as sensitive as other antibody detection techniques.
ELISAs
Blocking and competitive ELISAs using anti-H MAbs were developed for PPR sero-surveillance and sero-monitoring [75, 76]. The blocking ELISA had 90.4 % diagnostic sensitivity and 98.9 % diagnostic specificity when compared to the VNT [75]. Meanwhile, a competitive ELISA based on a baculovirus-expressed, recombinant N protein antigen, which also has high sensitivity (94.5 %) and specificity (99.4 %), was developed at the World Reference Laboratory [77]. Both anti-N and anti-H protein MAbs-based competitive ELISAs are available as commercial kits for the detection of antibodies against PPRV [75, 77]. Similarly, we developed a competitive ELISA based on an anti-H protein MAb using partially purified PPRV [73]. The diagnostic sensitivity (92.4 %) and diagnostic specificity (98.4 %) of this test were comparable to those of VNT and commercial ELISA kits [73, 78]. Owing to the non-infectious nature of the antigen, the N-protein-based competitive ELISA kit has potential for use in wider geographical areas, including PPR-free countries [77, 79]. However, in PPR-free countries, virus could be handled only under strict bio-security conditions and therefore would not be used for regular diagnosis. These ELISAs are, in general, simple and convenient and are both time- and cost-effective when large-scale sample screening is needed, and they are popular assays for the routine diagnosis of PPR.
Based on the global strategy, which is targeting PPR for eradication by the year 2030, it may be difficult to use the infectious virus as antigen in the near future. Before a country can achieve the PPR-free status, handling of infectious PPRV, even in laboratories, must be stopped, and intensive monitoring of disease must be carried out. There is therefore a need to replace native virus antigen with either recombinant or synthetic peptide antigen [73, 75]. To this end, an H protein was expressed in Vero cells [80] and insect cells [81]. However, currently, recombinant H protein of PPRV is not available for routine use in competitive ELISA. Amongst the antibody-based diagnostics of PPR, VNT might be the best test for sero-monitoring. However, it requires quality serum samples. The competitive ELISAs based on neutralizing MAbs (C77 and 4B11) could be used for both sero-surveillance and sero-monitoring [73, 75] of a large number of serum samples, even ones of poor quality. Although synthetic-peptide-based competitive ELISA has been developed for PPR antibody detection [50], it has not been validated for diagnostic use with field samples. Recently, another anti-H protein, MAb C4F3, and a blocking ELISA based on inactivated crude PPRV antigen were developed (currently under validation by AU-PANVAC; FAO/AU-PANVAC unpublished validation report).
An indirect ELISA, as a valuable alternative to competitive ELISA, was developed for PPR antibody detection [82] with a relative diagnostic specificity of 95.09 % and diagnostic sensitivity of 90.81 % when compared to competitive ELISA [73]. Although a species-specific conjugated secondary antibody is required, this indirect ELISA could be used if the MAb clone used in competitive ELISA is lost due to some unavoidable situations or in laboratories where competitive ELISA is not available. However, under the current circumstances, competitive ELISA might be the best choice for sero-surveillance of various species of domesticated and wild animals [56, 83].
Miscellaneous tools for PPR diagnosis
In addition to the conventional assays, improved understanding of biosensors and nanotechnology has facilitated the use of surface plasmon resonance (SPR) principles for disease diagnosis. This assay does not require labelling of antigen and antibody; however, one of the components needs to be immobilized on the chip surface. SPR-based biosensor assays for the detection of PPR antibodies are currently being explored by using recombinant N protein or synthetic peptide antigen of PPRV. Similarly, development of an SPR biosensor based on PPR monoclonal antibodies for the detection of PPRV has also been explored [84]. It is likely that these assays may be used in the future for PPR diagnosis by measuring antigen and antibody interactions in real time [84]. SPR-based assays may not be cost-effective for regular diagnosis; however, they could be applied for the research on antigen-antibody interactions.
A gold-nanoparticle-based strip assay for the detection of PPR antibodies was developed using a truncated recombinant N protein of PPRV. This strip test could be applied to detect antibodies to PPRV from goat, sheep, cattle and buffalo [85]. Additionally, a rapid visual test for the detection of PPRV was developed using PPRV-specific ligand-peptide-labelled gold nanoparticles, wherein a change of colour from red to blue indicates the presence of virus. With extensive clinical validation, this test might be useful for field diagnosis of PPR. A similar visual detection test has also been explored for PPR antibody detection [86]. Nucleic acid hybridization using probe-coupled gold nanoparticles and magnetic microparticles obviates the need for a thermocycler. It is also a rapid, sensitive, and time- and cost effective test [87]. Another nucleic acid detection method, namely, nanoparticle amplified immuno-PCR (NPA-IPCR) developed for respiratory syncytial virus (RSV) detection also has very high sensitivity in terms of detection limits [88], and similar assays could also be developed for sensitive detection of PPRV in the future.
Microarray techniques could be a feasible option for multi-disease screening for small ruminants. There are a few reports on the development of microarrays for PPR diagnosis, but this still needs to be explored for sensitive and specific detection of PPRV nucleic acid [89, 90]. Such assays may be important for syndromic surveillance for diseases of sheep and goats, especially mixed infections with similar clinical signs, as already described.
Disease diagnosis: perspectives on PPR control and eradication
The specific characteristics of PPRV such as antigenic stability, a single serotype, and the requirement for close contact for virus transmission, combined with the availability of potent vaccines, long-lasting immunity, and sensitive diagnostics support the prediction that eradication can be achieved. The diagnostic tools, which are rapid to perform and can detect virus at the early stages of disease are critical to support this endeavour. Although conventional and real-time RT-PCR are more sensitive than immunocapture/sandwich ELISA, the former tests are time-consuming and might not be economical when sample sizes are large during active clinical surveillance. They may also be difficult to implement in laboratories located in PPR-endemic areas. In contrast, ELISA is simple to perform on large numbers of samples and is a popular test for diagnosis of PPR during mass campaigns. Furthermore, immunochromatographic tests and one-step LAMP assays might be useful in laboratories with poor resources and therefore need to be validated to a higher degree [19, 71]. Diagnostic tests such as RT-PCR-ELISA would be useful to confirm clinical samples with marginal positivity [23], especially during the late phase of eradication, when each sample will likely need to be tested with a high level of stringency. A tentative, suggested pathway for PPR diagnosis during the eradication phase of the global eradication strategy is provided in which the diagnostics developed in different geographical areas are used (Fig. 3 and Fig. 4). We understand that the PPRV lineages are being repositioned now, and the lineage-differentiating nucleic-acid-based diagnostics may be important for detailed epidemiological investigations.
Currently, the use of live attenuated PPR vaccines prevent the differentiation of infected animals from vaccinated animals (DIVA). Development of these marker vaccines and suitable companion diagnostic tests will be helpful in assessing the impact of the control program as well as vaccine efficacy. During sero-surveillance in the later stages of PPR control and eradication, the use of a DIVA-enabled vaccine may avoid an unnecessary delay of eradication due to the presence of PPR antibodies. Because the detection of antibodies against PPRV might be due to infection or vaccination, this may help to achieve eradication earlier, in contrast to cases of rinderpest, which took a long time for elimination from the environment (http://rea.au.int/ar/sites/default/files/Eradication_of_Rinderpest_from_Africa_A_great_milestone.pdf). In view of this, attempts have been made to develop a 4B11 MAb-based escape mutant of PPRV in India [14] with the aim of using an available competitive ELISA as a DIVA companion test [73]. However, this 4B11 escape mutant of PPRV was unable to facilitate the serological DIVA strategy in vivo in spite of a lack of reactivity to the 4B11 MAb in ELISA (unpublished data). Similarly, a mutant PPRV with a mutation in the C77 MAb binding site in H was also rescued using reverse genetics techniques at the Pirbright Institute, UK, but this also lacked DIVA potential [15]. Another PPRV-specific anti-N MAb, 4G6, was raised against an immunodominant linear epitope of PPRV [91], and therefore, efforts to develop a 4G6 MAb-based marker vaccine and competitive ELISA could lead to a DIVA strategy.
Conclusion
From among the series of tests available for PPR diagnosis, each one has its own merits and disadvantages. These diagnostics could be applied at different time points and stages of PPR diagnosis, control and eradication in different geographical regions, based on existing levels of expertise and the resources available. Rapid tests such as the immunochromatographic test can be used for field-level diagnosis of PPR, whereas immunocapture and sandwich ELISA are useful for laboratory diagnosis. If these tests fail to detect PPRV, sensitive methods such as RT-PCR and RT-PCR-ELISA can be used to confirm the disease. Rapid diagnostics are helpful for flock-level diagnosis rather than on individual animals, because when one or few animals are positive for infection in an immunochromatographic test, the flock is considered positive. Likewise, immunocapture/sandwich ELISA is a user-friendly test for routine clinical surveillance and diagnosis of PPR. For the detection of PPRV during early phases of disease and for samples that gave ambiguous results in other tests and require re-confirmation, highly sensitive nucleic-acid-based tests such as RT-PCR and RT-PCR-ELISA could be used. For antibody detection during sero-surveillance and sero-monitoring, tests such as competitive/blocking ELISA can be used for routine diagnosis, and VNT, on specified samples. To ensure the availability of DIVA through a suitable marker vaccine and companion diagnostic tests, different approaches (reverse genetics, mAr mutants, recombinant protein/viruses) are being explored. The four stages of FAO-OIE’s PPR global control and eradication strategy, viz. Assessment, Control, Eradication and Post eradication, involve the extensive use of diagnostics with variable sensitivity and specificity. Therefore, countries with self-sufficiency and validated PPR diagnostics need to extend help to resource-poor countries of the world across the national, regional and continental boundaries in order to support PPR control and eradication. In fact, if a multivalent vaccine is available for economically important diseases of small ruminants, such as bluetongue, capripox, and others, control strategies (by national authorities) could be merged without any compromise of PPR eradication. Development of a multivalent vaccine and multi-disease discriminatory diagnostic assays would also facilitate poverty alleviation through improvement of small-ruminant production. However, during the final stages of PPR eradication, more-focused approaches may be required to finally eliminate the virus from the environment.
References
Munir M (2014) Role of wild small ruminants in the epidemiology of peste des petits ruminants. Transbound Emerg Dis 61:411–424. doi:10.1111/tbed.12052
Parida S, Muniraju M, Mahapatra M et al (2015) Peste des petits ruminants. Vet Microbiol 181:90–106. doi:10.1016/j.vetmic.2015.08.009
Wohlsein P, Singh RP (2015) Peste des petits ruminants in unusual hosts: epidemiology, disease, and impact on eradication. In: Munir M (ed) Peste des petits ruminants virus. Springer, Berlin, pp 95–118
Food and Agriculture Organization of United Nations, World Organization for Animal Health (2015) Global Strategy for the Control and Eradication of PPR. FAO and OIE, Ivory Coast
Dhar P, Sreenivasa BP, Barrett T et al (2002) Recent epidemiology of peste des petits ruminants virus (PPRV). Vet Microbiol 88:153–159
Albina E, Kwiatek O, Minet C et al (2013) Peste des petits ruminants, the next eradicated animal disease? Vet Microbiol 165:38–44. doi:10.1016/j.vetmic.2012.12.013
Banyard AC, Parida S, Batten C et al (2010) Global distribution of peste des petits ruminants virus and prospects for improved diagnosis and control. J Gen Virol 91:2885–2897. doi:10.1099/vir.0.025841-0
Libeau G, Kwiatek O, Lancelot R, Albina E (2011) Peste des petits ruminants, growing incidence worldwide. French Agricultural Research Centre for International Development (CIRAD), BIOS Department, Control of Exotic and Emerging Animal Diseases, Montpellier
Sen A, Saravanan P, Balamurugan V et al (2010) Vaccines against peste des petits ruminants virus. Expert Rev Vaccines 9:785–796. doi:10.1586/erv.10.74
Singh RK, Balamurugan V, Bhanuprakash V et al (2009) Possible control and eradication of peste des petits ruminants from India: technical aspects. Vet Ital 45:449–462
Singh RP (2011) Control strategies for peste des petits ruminants in small ruminants of India. Rev Sci Tech Off Int Epizoot 30:879–887
Singh RP, Bandyopadhyay SK (2015) Peste des petits ruminants vaccine and vaccination in India: sharing experience with disease endemic countries. Virus Dis 26:215–224. doi:10.1007/s13337-015-0281-9
Saravanan P, Sen A, Balamurugan V et al (2010) Comparative efficacy of peste des petits ruminants (PPR) vaccines. Biologicals 38:479–485. doi:10.1016/j.biologicals.2010.02.003
Getachew B, Haque AE, Upmanyu V et al (2014) Invitro-selection and molecular characterization of monoclonal antibody resistant mutant of an Indian strain of PPR vaccine virus. Presented In: National conference on PPR disease and promotion of national scientific forum held at NASC complex, New Delhi
Muniraju M, Mahapatra M, Buczkowski H et al (2015) Rescue of a vaccine strain of peste des petits ruminants virus: in vivo evaluation and comparison with standard vaccine. Vaccine 33:465–471. doi:10.1016/j.vaccine.2014.10.050
Balamurugan V, Hemadri D, Gajendragad MR et al (2014) Diagnosis and control of peste des petits ruminants: a comprehensive review. Virus Dis 25:39–56. doi:10.1007/s13337-013-0188-2
Libeau G (2015) Current advances in serological diagnosis of peste des petits ruminants virus. In: Munir M (ed) Peste des petits ruminants virus. Springer, Berlin, pp 133–154
Balamurugan V, Sen A, Saravanan P et al (2006) One-step multiplex RT-PCR assay for the detection of peste des petits ruminants virus in clinical samples. Vet Res Commun 30:655–666. doi:10.1007/s11259-006-3331-3
Baron J, Fishbourne E, Couacy-Hyman E et al (2014) Development and testing of a field diagnostic assay for peste des petits ruminants virus. Transbound Emerg Dis 61:390–396. doi:10.1111/tbed.12266
Couacy-Hymann E, Roger F, Hurard C et al (2002) Rapid and sensitive detection of peste des petits ruminants virus by a polymerase chain reaction assay. J Virol Methods 100:17–25. doi:10.1016/S0166-0934(01)00386-X
Libeau G, Diallo A, Colas F, Guerre L (1994) Rapid differential diagnosis of rinderpest and peste des petits ruminants using an immunocapture ELISA. Vet Rec 134:300–304
Singh RP, Sreenivasa BP, Dhar P, Bandyopadhyay SK (2004) A sandwich-ELISA for the diagnosis of peste des petits ruminants (PPR) infection in small ruminants using anti-nucleocapsid protein monoclonal antibody. Arch Virol 149:2155–2170. doi:10.1007/s00705-004-0366-z
Saravanan P, Singh RP, Balamurugan V et al (2004) Development of a N gene-based PCR-ELISA for detection of peste-des-petits-ruminants virus in clinical samples. Acta Virol 48:249–255
Malik YS, Singh D, Chandrashekar KM et al (2011) Occurrence of dual infection of peste-des-petits-ruminants and goatpox in indigenous goats of central India. Transbound Emerg Dis 58:268–273. doi:10.1111/j.1865-1682.2011.01201.x
Mondal B, Sen A, Chand K et al (2009) Evidence of mixed infection of peste des petits ruminants virus and bluetongue virus in a flock of goats as confirmed by detection of antigen, antibody and nucleic acid of both the viruses. Trop Anim Health Prod 41:1661–1667. doi:10.1007/s11250-009-9362-3
Peste des petits ruminants (2013) In: Manual of diagnostic tests and vaccines for terrestrial animals: mammals, birds, and bees. Office international des épizooties, Paris, pp 1–14
Sarkar J, Sreenivasa BP, Singh RP et al (2003) Comparative efficacy of various chemical stabilizers on the thermostability of a live-attenuated peste des petits ruminants (PPR) vaccine. Vaccine 21:4728–4735
Sreenivasa BP, Singh RP, Mondal B et al (2006) Marmoset B95a cells: a sensitive system for cultivation of peste des petits ruminants (PPR) virus. Vet Res Commun 30:103–108. doi:10.1007/s11259-005-3200-5
Balamurugan V, Sen A, Venkatesan G et al (2010) Isolation and identification of virulent peste des petits ruminants viruses from PPR outbreaks in India. Trop Anim Health Prod 42:1043–1046. doi:10.1007/s11250-010-9527-0
Brindha K, Raj GD, Ganesan PI et al (2001) Comparison of virus isolation and polymerase chain reaction for diagnosis of peste des petits ruminants. Acta Virol 45:169–172
Kumar N, Chaubey KK, Chaudhary K et al (2013) Isolation, identification and characterization of a peste des petits ruminants virus from an outbreak in Nanakpur, India. J Virol Methods 189:388–392. doi:10.1016/j.jviromet.2013.03.002
Singh RP, De UK, Pandey KD (2010) Virological and antigenic characterization of two peste des petits ruminants (PPR) vaccine viruses of Indian origin. Comp Immunol Microbiol Infect Dis 33:343–353. doi:10.1016/j.cimid.2008.12.003
Adombi CM, Lelenta M, Lamien CE et al (2011) Monkey CV1 cell line expressing the sheep–goat SLAM protein: a highly sensitive cell line for the isolation of peste des petits ruminants virus from pathological specimens. J Virol Methods 173:306–313. doi:10.1016/j.jviromet.2011.02.024
Obi TU, Patrick D (1984) The detection of peste des petits ruminants (PPR) virus antigen by agar gel precipitation test and counter-immunoelectrophoresis. J Hyg 93:579–586
Majiyagbe KA, Nawathe DR, Abegunde A (1984) Rapid diagnosis of peste des petits ruminants (PPR) infection, application of immunoelectroosmophoresis (IEOP) technique [1984]. Rev Elev Méd vét Pays Trop 37:11–15
Sumption KJ, Aradom G, Libeau G, Wilsmore AJ (1998) Detection of peste des petits ruminants virus antigen in conjunctival smears of goats by indirect immunofluorescence. Vet Rec 142:421–424
Abu Elzein EME, Al-Naeem A (2009) Utilization of protein-A in immuno-histochemical techniques for detection of peste des petits ruminants (PPR) virus antigens in tissues of experimentally infected goats. Trop Anim Health Prod 41:1–4. doi:10.1007/s11250-008-9161-2
Munir M (2013) Peste des petits ruminants virus. In: Munir M (ed) Mononegaviruses of veterinary importance: pathobiology and molecular diagnosis. CAB International, Oxfordshire, pp 65–98
Ezeibe MC, Wosu L, Erumaka I (2004) Standardisation of the haemagglutination test for peste des petits ruminants (PPR). Small Ruminant Res 51:269–272. doi:10.1016/S0921-4488(03)00123-8
Wosu LO (1991) Haemagglutination test for diagnosis of peste des petits ruminants disease in goats with samples from live animals. Small Ruminant Res 5:169–172. doi:10.1016/0921-4488(91)90041-N
Ishag OM, Intisar KS, Ali YH (2015) Detection of peste des petits ruminants virus antigen by reverse passive haemagglutination test: application and evaluation. Global J Anim Sci Res 3:199–205
Dhinakar Raj G, Nachimuthu K, Mahalinga Nainar A (2000) A simplified objective method for quantification of peste des petits ruminants virus or neutralizing antibody. J Virol Methods 89:89–95
Sarkar J, Belaineh G, Sreenivasa B, Singh RP (2012) Development of a cell-ELISA using anti-nucleocapsid protein monoclonal antibody for the titration of PPR vaccine virus. Indian J Comp Microbiol Immunol Infect Dis 33:18–20
Singh RP, Bandyopadhyay SK, Sreenivasa BP, Dhar P (2004) Production and characterization of monoclonal antibodies to peste des petits ruminants (PPR) virus. Vet Res Commun 28:623–639
Balamurugan V, Saravanan P, Sen A et al (2012) Prevalence of peste des petits ruminants among sheep and goats in India. J Vet Sci 13:279–285
Obi TU, Ojeh CK (1989) Dot enzyme immunoassay for visual detection of peste-des-petits-ruminants virus antigen from infected caprine tissues. J Clin Microbiol 27:2096–2099
Saravanan P, Balamurugan V, Sen A et al (2006) Development of dot-ELISA for diagnosis of peste des petits ruminants (PPR) in small ruminants. J Appl Anim Res 30:121–124. doi:10.1080/09712119.2006.9706600
Brüning-Richardson A, Akerblom L, Klingeborn B, Anderson J (2011) Improvement and development of rapid chromatographic strip-tests for the diagnosis of rinderpest and peste des petits ruminants viruses. J Virol Methods 174:42–46. doi:10.1016/j.jviromet.2011.03.016
Verma HN (2013) Development of rapid assay for peste des petits ruminants virus based on gold label. M. V. Sc. thesis, ICAR-Indian Veterinary Research Institute, Izatnagar
Shrivastava S (2006) Development of synthetic antigens for diagnosis of peste des petits ruminants. Ph.D. thesis, ICAR-Indian Veterinary Research Institute, Izatnagar
Bailey D, Banyard A, Dash P et al (2005) Full genome sequence of peste des petits ruminants virus, a member of the Morbillivirus genus. Virus Res 110:119–124. doi:10.1016/j.virusres.2005.01.013
Shaila MS, Purushothaman V, Bhavasar D et al (1989) Peste des petits ruminants of sheep in India. Vet Rec 125:602
Diallo A, Barrett T, Barbron M et al (1989) Differentiation of rinderpest and peste des petits ruminants viruses using specific cDNA clones. J Virol Methods 23:127–136
Pandey KD, Baron MD, Barrett T (1992) Differential diagnosis of rinderpest and PPR using biotinylated cDNA probes. Vet Rec 131:199–200
Forsyth MA, Barrett T (1995) Evaluation of polymerase chain reaction for the detection and characterisation of rinderpest and peste des petits ruminants viruses for epidemiological studies. Virus Res 39:151–163. doi:10.1016/0168-1702(95)00076-3
Mahapatra M, Sayalel K, Muniraju M et al (2015) Spillover of peste des petits ruminants virus from domestic to wild ruminants in the Serengeti ecosystem, Tanzania. Emerg Infect Diseases 21:2230–2234. doi:10.3201/eid2112.150223
Aleyas AG (2002) Comparative evaluation of different gene targets for PCR diagnosis of peste des petits ruminants. MVSc. Thesis, ICAR-Indian Veterinary Research Institute, Izatnagar
Settypalli TBK, Lamien CE, Spergser J et al (2016) One-step multiplex RT-qPCR assay for the detection of peste des petits ruminants virus, Capripoxvirus, Pasteurella multocida and Mycoplasma capricolum subspecies (ssp.) capripneumoniae. PLoS One 11:e0153688. doi:10.1371/journal.pone.0153688
Abera T, Thangavelu A, Joy Chandran N, Raja A (2014) A SYBR Green I based real time RT-PCR assay for specific detection and quantitation of peste des petits ruminants virus. BMC Vet Res 10:22. doi:10.1186/1746-6148-10-22
Bao J, Li L, Wang Z et al (2008) Development of one-step real-time RT-PCR assay for detection and quantitation of peste des petits ruminants virus. J Virol Methods 148:232–236. doi:10.1016/j.jviromet.2007.12.003
Batten CA, Banyard AC, King DP et al (2011) A real time RT-PCR assay for the specific detection of peste des petits ruminants virus. J Virol Methods 171:401–404. doi:10.1016/j.jviromet.2010.11.022
Kwiatek O, Keita D, Gil P et al (2010) Quantitative one-step real-time RT-PCR for the fast detection of the four genotypes of PPRV. J Virol Methods 165:168–177. doi:10.1016/j.jviromet.2010.01.014
Balamurugan V, Sen A, Venkatesan G et al (2012) A rapid and sensitive one step-SYBR green based semi quantitative real time RT-PCR for the detection of peste des petits ruminants virus in the clinical samples. Virol Sin 27:1–9. doi:10.1007/s12250-012-3219-z
Balamurugan V, Sen A, Venkatesan G et al (2010) Application of semi-quantitative M gene-based hydrolysis probe (TaqMan) real-time RT-PCR assay for the detection of peste des petitis ruminants virus in the clinical samples for investigation into clinical prevalence of disease: M gene-based hydrolysis probe RT-PCR for PPR diagnosis. Transbound Emerg Dis 57:383–395. doi:10.1111/j.1865-1682.2010.01160.x
Senthil Kumar C, Dhinakar Raj G, Thangavelu A, Shaila MS (2007) Performance of RT-PCR-ELISA for the detection of peste des petits ruminants virus. Small Ruminant Res 72:200–208. doi:10.1016/j.smallrumres.2006.09.004
Forsyth MA, Parida S, Alexandersen S et al (2003) Rinderpest virus lineage differentiation using RT-PCR and SNAP-ELISA. J Virol Methods 107:29–36
Notomi T, Mori Y, Tomita N, Kanda H (2015) Loop-mediated isothermal amplification (LAMP): principle, features, and future prospects. J Microbiol 53:1–5. doi:10.1007/s12275-015-4656-9
Mohandas SS, Muthuchelvan D, Pandey AB et al (2015) Development of reverse transcription loop mediated isothermal amplification assay for rapid detection of bluetongue viruses. J Virol Methods 222:103–105. doi:10.1016/j.jviromet.2015.06.005
Venkatesan G, Bhanuprakash V, Balamurugan V (2015) Development and comparative evaluation of loop mediated isothermal amplification (LAMP) assay for simple visual detection of orf virus in sheep and goats. Mol Cell Probes 29:193–195. doi:10.1016/j.mcp.2015.03.006
Dadas RC, Dhanavelu M, Pandey AB et al (2012) Development of loop-mediated isothermal amplification (LAMP) assay for rapid detection of peste des petits ruminants virus (PPRV) genome from clinical samples. Indian J Comp Microbiol Immunol Infect Dis 33:7–13
Li L, Bao J, Wu X et al (2010) Rapid detection of peste des petits ruminants virus by a reverse transcription loop-mediated isothermal amplification assay. J Virol Methods 170:37–41. doi:10.1016/j.jviromet.2010.08.016
Rossiter PB, Jessett DM, Taylor WP (1985) Microneutralisation systems for use with different strains of peste des petits ruminants virus and rinderpest virus. Trop Anim Health Prod 17:75–81. doi:10.1007/BF02360775
Singh RP, Sreenivasa BP, Dhar P et al (2004) Development of a monoclonal antibody based competitive-ELISA for detection and titration of antibodies to peste des petits ruminants (PPR) virus. Vet Microbiol 98:3–15
Tahir MT, Ahmad R, Hussain I, Hussain M (1998) Counter-immunoelectrophoresis—a rapid technique for the diagnosis of peste-des-petits ruminants. Pak Vet J 18:55–56
Anderson J, McKay JA (1994) The detection of antibodies against peste des petits ruminants virus in cattle, sheep and goats and the possible implications to rinderpest control programmes. Epidemiol Infect 112:225–231
Saliki JT, Libeau G, House JA et al (1993) Monoclonal antibody-based blocking enzyme-linked immunosorbent assay for specific detection and titration of peste-des-petits-ruminants virus antibody in caprine and ovine sera. J Clin Microbiol 31:1075–1082
Libeau G, Préhaud C, Lancelot R et al (1995) Development of a competitive ELISA for detecting antibodies to the peste des petits ruminants virus using a recombinant nucleoprotein. Res Vet Sci 58:50–55
Singh RP, Saravanan P, Sreenivasa BP et al (2006) Comparison of diagnostic efficacy of a monoclonal antibody-based competitive ELISA test with a similar commercial test for the detection of antibodies to peste des petits ruminants (PPR) virus. Vet Res Commun 30:325–330. doi:10.1007/s11259-006-3192-9
Couacy-Hymann E, Bodjo SC, Tounkara K et al (2007) Comparison of two competitive ELISAs for the detection of specific peste-des-petits-ruminant antibodies in sheep and cattle populations. Afr J Biotechnol 6:732–736
Balamurugan V, Sen A, Saravanan P et al (2006) Development and characterization of a stable vero cell line constitutively expressing peste des petits ruminants virus (PPRV) hemagglutinin protein and its potential use as antigen in enzyme-linked immunosorbent assay for serosurveillance of PPRV. Clin Vaccine Immunol 13:1367–1372. doi:10.1128/CVI.00273-06
Sinnathamby G, Renukaradhya GJ, Rajasekhar M et al (2001) Immune responses in goats to recombinant hemagglutinin-neuraminidase glycoprotein of peste des petits ruminants virus: identification of a T cell determinant. Vaccine 19:4816–4823. doi:10.1016/S0264-410X(01)00210-9
Balamurugan V, Singh RP, Saravanan P et al (2007) Development of an indirect ELISA for the detection of antibodies against peste-des-petits-ruminants virus in small ruminants. Vet Res Commun 31:355–364. doi:10.1007/s11259-006-3442-x
Singh RP, Saravanan P, Sreenivasa BP et al (2004) Prevalence and distribution of peste des petits ruminants virus infection in small ruminants in India. Rev Sci Tech Off Int Epizoot 23:807–819
Anonymous (2014) Annual Report. ICAR-Indian Veterinary Research Institute, Izatnagar
Venkatachalam, Shaila M, Dhinakar Raj G (2010) A test strip for qualitative detection of antibodies to peste des petits ruminant virus. Tamil Nadu Veterinary and Animal Sciences University, Chennai/Indian Institute of Science, Bangalore (Indian Patent application)
Anonymous (2015) Annual Report. ICAR-Indian Veterinary Research Institute, Izatnagar
Tao C, Li G, Wang Y, Huang H (2013) Enzymatic reporting of peste des petits ruminants virus genes ligating two specific probes on nanoparticles. Biotechnol Lett 35:613–618. doi:10.1007/s10529-012-1120-3
Perez JW, Vargis EA, Russ PK et al (2011) Detection of respiratory syncytial virus using nanoparticle amplified immuno-polymerase chain reaction. Anal Biochem 410:141–148. doi:10.1016/j.ab.2010.11.033
Jack PJM, Amos-Ritchie RN, Reverter A et al (2009) Microarray-based detection of viruses causing vesicular or vesicular-like lesions in livestock animals. Vet Microbiol 133:145–153. doi:10.1016/j.vetmic.2008.05.030
Ratta B, Pokhriyal M, Singh SK et al (2016) Detection of peste des petits ruminants virus (PPRV) genome from nasal swabs of dogs. Curr Microbiol. doi:10.1007/s00284-016-1030-z
Dechamma HJ, Dighe V, Kumar CA et al (2006) Identification of T-helper and linear B epitope in the hypervariable region of nucleocapsid protein of PPRV and its use in the development of specific antibodies to detect viral antigen. Vet Microbiol 118:201–211. doi:10.1016/j.vetmic.2006.07.023
Diallo A, Taylor WP, Lefèvre PC, Provost A (1989) Atténuation d’une souche de virus de la peste des petits ruminants: candidat pour un vaccin homologue. Rev Elev Méd vét Pays Trop 42:311–317
Choi K-S, Nah J-J, Choi C-U et al (2003) Monoclonal antibody-based competitive ELISA for simultaneous detection of rinderpest virus and peste des petits ruminants virus antibodies. Vet Microbiol 96:1–16
Acknowledgments
The authors would like to acknowledge the funding from the Department of Biotechnology (grant no. BT/IN/Indo-UK/FADH/50/GDR/2013) and the Department of Science and Technology (sanction order no. DST/INSPIRE fellowship/2013/675), Government of India. The authors are thankful to Dr. Dalan Bailey, FAO volunteer, University of Birmingham, UK, for editing the manuscript and improvement of the English language. The authors also thank Sophia and Philma for reading the manuscript for useful suggestions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Santhamani, R., Singh, R.P. & Njeumi, F. Peste des petits ruminants diagnosis and diagnostic tools at a glance: perspectives on global control and eradication. Arch Virol 161, 2953–2967 (2016). https://doi.org/10.1007/s00705-016-3009-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00705-016-3009-2