Abstract
Background
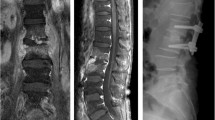
Due to the aging society, the incidence of pyogenic spondylodiscitis is still rising. Although surgical treatment for spondylodiscitis in general is increasingly accepted, an optimal surgical strategy for treatment of pyogenic spinal infection has not yet been established. The aim of this study was to investigate the suitability of percutaneous posterior pedicle screw fixation for surgical treatment in patients with spondylodiscitis of the thoracolumbar spine.
Methods
We conducted a retrospective review of a consecutive cohort of patients undergoing surgical treatment for spondylodiscitis of the thoracolumbar spine between January 2017 and December 2019. We assessed intraoperative and clinical data, comparing for the classic open and the percutaneous approach. In total, we analyzed 125 cases (39 female, 86 male). The mean age was 69.49 years ± 12.63 years.
Results
Forty-seven (37.6%) patients were operated on by a percutaneous approach for pedicle screw fixation, and 78 (62.4%) received open surgery. There was no significant difference in the mean age of patients between both groups (p= 0.57). The time of surgery for percutaneous fixation was statistically significantly shorter (p= 0.03). Furthermore, the estimated intraoperative blood loss was significantly lower in the minimally invasive group (p < 0.001). No significant difference could be observed regarding the recurrence rate of spondylodiscitis and the occurrence of surgical site infections (p= 0.2 and 0.5, respectively).
Conclusion
Percutaneous posterior pedicle screw fixation appears to be a feasible option for the surgical treatment of a selected patient group with spondylodiscitis of the thoracic and lumbar spine.





Similar content being viewed by others
Abbreviations
- ECs:
-
erythrocyte concentrates
- MISS:
-
minimal invasive spine surgery
- CRP:
-
C-reactive protein
- ICU:
-
intensive care unit
References
Akiyama T, Chikuda H, Yasunaga H, Horiguchi H, Fushimi K, Saita K (2013) Incidence and risk factors for mortality of vertebral osteomyelitis: a retrospective analysis using the Japanese diagnosis procedure combination database. BMJ Open 3. https://doi.org/10.1136/bmjopen-2012-002412
Bernard L, Dinh A, Ghout I, Simo D, Zeller V, Issartel B, Le Moing V, Belmatoug N, Lesprit P, Bru JP, Therby A, Bouhour D, Denes E, Debard A, Chirouze C, Fevre K, Dupon M, Aegerter P, Mulleman D, Duration of rreatment for spondylodiscitis study g (2015) Antibiotic treatment for 6 weeks versus 12 weeks in patients with pyogenic vertebral osteomyelitis: an open-label, non-inferiority, randomised, controlled trial. Lancet 385:875–882. https://doi.org/10.1016/S0140-6736(14)61233-2
Cheung WY, Luk KD (2012) Pyogenic spondylitis. Int Orthop 36:397–404. https://doi.org/10.1007/s00264-011-1384-6
Duan K, Qin Y, Ye J, Zhang W, Hu X, Zhou J, Gao L, Tang Y (2020) Percutaneous endoscopic debridement with percutaneous pedicle screw fixation for lumbar pyogenic spondylodiscitis: a preliminary study. Int Orthop 44:495–502. https://doi.org/10.1007/s00264-019-04456-1
Farah K, Peyriere H, Graillon T, Prost S, Dufour H, Blondel B, Fuentes S (2020) Minimally invasive posterior fixation and anterior debridement-fusion for thoracolumbar spondylodiscitis: a 40-case series and review of the literature. Neurochirurgie 66:24–28. https://doi.org/10.1016/j.neuchi.2019.10.009
Gejo R, Matsui H, Kawaguchi Y, Ishihara H, Tsuji H (1999) Serial changes in trunk muscle performance after posterior lumbar surgery. Spine (Phila Pa 1976) 24:1023–1028. https://doi.org/10.1097/00007632-199905150-00017
Gonzalvo A, Abdulla I, Riazi A, De La Harpe D (2011) Single-level/single-stage debridement and posterior instrumented fusion in the treatment of spontaneous pyogenic osteomyelitis/discitis: long-term functional outcome and health-related quality of life. J Spinal Disord Tech 24:110–115. https://doi.org/10.1097/BSD.0b013e3181dd8115
Goodnough LT, Maggio P, Hadhazy E, Shieh L, Hernandez-Boussard T, Khari P, Shah N (2014) Restrictive blood transfusion practices are associated with improved patient outcomes. Transfusion 54:2753–2759. https://doi.org/10.1111/trf.12723
Gouliouris T, Aliyu SH, Brown NM (2010) Spondylodiscitis: update on diagnosis and management. J Antimicrob Chemother 65(Suppl 3):iii11–iii24. https://doi.org/10.1093/jac/dkq303
Guerado E, Cervan AM (2012) Surgical treatment of spondylodiscitis. An update. Int Orthop 36:413–420. https://doi.org/10.1007/s00264-011-1441-1
Kandwal P, Garg B, Upendra B, Chowdhury B, Jayaswal A (2012) Outcome of minimally invasive surgery in the management of tuberculous spondylitis. Indian J Orthop 46:159–164. https://doi.org/10.4103/0019-5413.93680
Kato S, Chikuda H, Ohya J, Oichi T, Matsui H, Fushimi K, Takeshita K, Tanaka S, Yasunaga H (2016) Risk of infectious complications associated with blood transfusion in elective spinal surgery-a propensity score matched analysis. Spine J 16:55–60. https://doi.org/10.1016/j.spinee.2015.10.014
Lee BH, Park JO, Kim HS, Lee HM, Cho BW, Moon SH (2014) Transpedicular curettage and drainage versus combined anterior and posterior surgery in infectious spondylodiscitis. Indian J Orthop 48:74–80. https://doi.org/10.4103/0019-5413.125508
Lin TY, Tsai TT, Lu ML, Niu CC, Hsieh MK, Fu TS, Lai PL, Chen LH, Chen WJ (2014) Comparison of two-stage open versus percutaneous pedicle screw fixation in treating pyogenic spondylodiscitis. BMC Musculoskelet Disord 15:443. https://doi.org/10.1186/1471-2474-15-443
Mikhail C, Pennington Z, Arnold PM, Brodke DS, Chapman JR, Chutkan N, Daubs MD, DeVine JG, Fehlings MG, Gelb DE, Ghobrial GM, Harrop JS, Hoelscher C, Jiang F, Knightly JJ, Kwon BK, Mroz TE, Nassr A, Riew KD, Sekhon LH, Smith JS, Traynelis VC, Wang JC, Weber MH, Wilson JR, Witiw CD, Sciubba DM, Cho SK (2020) Minimizing blood loss in spine surgery. Global Spine J 10:71S–83S. https://doi.org/10.1177/2192568219868475
Mobbs RJ, Sivabalan P, Li J (2011) Technique, challenges and indications for percutaneous pedicle screw fixation. J Clin Neurosci 18:741–749. https://doi.org/10.1016/j.jocn.2010.09.019
Pee YH, Park JD, Choi YG, Lee SH (2008) Anterior debridement and fusion followed by posterior pedicle screw fixation in pyogenic spondylodiscitis: autologous iliac bone strut versus cage. J Neurosurg Spine 8:405–412. https://doi.org/10.3171/SPI/2008/8/5/405
Rutges JP, Kempen DH, van Dijk M, Oner FC (2016) Outcome of conservative and surgical treatment of pyogenic spondylodiscitis: a systematic literature review. Eur Spine J 25:983–999. https://doi.org/10.1007/s00586-015-4318-y
Shiban E, Janssen I, Wostrack M, Krieg SM, Ringel F, Meyer B, Stoffel M (2014) A retrospective study of 113 consecutive cases of surgically treated spondylodiscitis patients. A single-center experience. Acta Neurochir (Wien) 156:1189–1196. https://doi.org/10.1007/s00701-014-2058-0
Skaf GS, Domloj NT, Fehlings MG, Bouclaous CH, Sabbagh AS, Kanafani ZA, Kanj SS (2010) Pyogenic spondylodiscitis: an overview. J Infect Public Health 3:5–16. https://doi.org/10.1016/j.jiph.2010.01.001
Styf JR, Willen J (1998) The effects of external compression by three different retractors on pressure in the erector spine muscles during and after posterior lumbar spine surgery in humans. Spine (Phila Pa 1976) 23:354–358. https://doi.org/10.1097/00007632-199802010-00014
Vcelak J, Chomiak J, Toth L (2014) Surgical treatment of lumbar spondylodiscitis: a comparison of two methods. Int Orthop 38:1425–1434. https://doi.org/10.1007/s00264-014-2360-8
Wang Y, Shi X, Wen M, Chen Y, Zhang Q (2017) Restrictive versus liberal blood transfusion in patients with coronary artery disease: a meta-analysis. Curr Med Res Opin 33:761–768. https://doi.org/10.1080/03007995.2017.1280010
Xu DS, Walker CT, Godzik J, Turner JD, Smith W, Uribe JS (2018) Minimally invasive anterior, lateral, and oblique lumbar interbody fusion: a literature review. Ann Transl Med 6:104. https://doi.org/10.21037/atm.2018.03.24
Zarghooni K, Rollinghoff M, Sobottke R, Eysel P (2012) Treatment of spondylodiscitis. Int Orthop 36:405–411. https://doi.org/10.1007/s00264-011-1425-1
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (the ethics committee of the Technical University of Munich (No. 238/17 S)) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Comments
The authors present their 3-year series of 125 spondylodiscitis patients, who were surgically treated either by an open posterior approach or percutaneous instrumentation +/- midline decompression/debridement +/- a second anterolateral debridement approach. Percutaneous surgery had advantages (MIS) and achieved comparable results. This is an important paper supporting MIS for spinal infection, which has clear advantages in suitable patients.
The main limitations, which the authors state themselves, are the selection bias, as the percutaneous group was less severe, and the fact that 68% of MIS patients received a second staged procedure. Nevertheless, it is well demonstrated that many patients can be treated in a minimally-invasive fashion, which is particularly helpful in this elderly and often comorbid population. Early and aggressive surgery for spinal infection has been repeatedly suggested recently and has been associated with decreased mortality. However, spine surgeons may still be reluctant to proceed with extensive open surgery in these cases. Using MIS and/or staging the procedure, as suggested by this distinguished group, offers a solution that can be tailored to the individual patient. Therefore, the difficult decision we were faced with in the past between less effective conservative care and an extensive surgical procedure with high perioperative morbidity and mortality is circumvented.
Decision-making in these patients has to consider (1) the presence (or absence) of an intraspinal abscess, which may require surgical drainage and direct decompression and (2) the extent of destruction of the anterior column, which may require debridement and reconstruction. As the authors nicely show, both can be achieved as an add-on to percutaneous pedicle screw instrumentation in a MIS fashion via a small midline or a lateral approach.
Claudius Thome,
Tirol, Austria
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Infection
Rights and permissions
About this article
Cite this article
Janssen, I.K., Jörger, AK., Barz, M. et al. Minimally invasive posterior pedicle screw fixation versus open instrumentation in patients with thoracolumbar spondylodiscitis. Acta Neurochir 163, 1553–1560 (2021). https://doi.org/10.1007/s00701-021-04744-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-021-04744-z