Abstract
Purpose
The aim of this study is to evaluate the factors that affect health-related quality of life (HRQoL) in untreated adolescent idiopathic scoliosis (AIS) patients in adulthood. We investigate the effect of clinical and radiological parameters on the SRS-22 results.
Methods
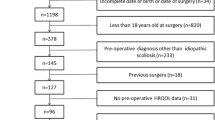
A total of 286 untreated adolescent idiopathic scoliosis patients at adult age between April 2021 and April 2022 who were admitted to our clinic were included in the study. Rotational deformities were evaluated with a scoliometer. Cobb angles, coronal balance, clavicle angle, coronal pelvic tilt, trunk shift, and apical vertebral translation were measured in standing anteroposterior X-rays. The effect of each clinical and radiological parameter on SRS-22 results was evaluated.
Results
No correlation was found between gender, age, curve type, presence of gibbosity or diagnosis time, and SRS-22 scores. A negative correlation was found between the BMI of the patients and the self-image scores (r = − 0.246, p < 0.01) and function scores (r = − 0.193, p < 0.05). Main thoracic (MT) gibbosity negatively correlates with self-image and total SRS-22 scores. Also, negative correlations were found between lumbar/thoracolumbar (LTL) gibbosity, function, and pain scores. MT Cobb angle magnitude was negatively correlated with self-image, mental health, and total SRS-22 scores. There were negative correlations between clavicle angle and mental health score, coronal pelvic tilt and self-image score, and apical vertebral translation and pain score.
Conclusion
BMI, MT gibbosity, LTL gibbosity, MT Cobb angle, clavicle angle, coronal pelvic tilt, and apical vertebral translation were negatively correlated with SRS-22 domains in untreated AIS patients in adulthood.




Similar content being viewed by others
Availability of data and material
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request. Code availability Statistics code is available upon request.
References
Weinstein SL (2019) The natural history of adolescent idiopathic scoliosis. J Pediatr Orthop 39(Issue 6, Suppl 1):S44–S46. https://doi.org/10.1097/BPO.0000000000001350
Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA (2008) Adolescent idiopathic scoliosis. Lancet 371(9623):1527–1537. https://doi.org/10.1016/S0140-6736(08)60658-3
Haberal B, Yaradılmıs YU (2021) Adolescent idiopathic scoliosis: a bibliographic analysis of the most 50 cited articles. J Turk Spinal Surg 32(1):1–7. https://doi.org/10.4274/jtss.galenos.2021.376
Tambe AD, Panikkar SJ, Millner PA, Tsirikos AI (2018) Current concepts in the surgical management of adolescent idiopathic scoliosis. Bone Joint J 100-B (4):415–424. https://doi.org/10.1302/0301-620X.100B4.BJJ-2017-0846.R2
Ohashi M, Watanabe K, Hirano T, Hasegawa K, Katsumi K, Shoji H, Mizouchi T, Endo N (2018) Predicting factors at skeletal maturity for curve progression and low back pain in adult patients treated nonoperatively for adolescent idiopathic scoliosis with thoracolumbar/lumbar curves: a mean 25-year follow-up. Spine (Phila Pa 1976) 43(23):E1403–E1411. https://doi.org/10.1097/BRS.0000000000002716
Watanabe K, Ohashi M, Hirano T, Katsumi K, Mizouchi T, Tashi H, Minato K, Hasegawa K, Endo N (2020) Health-related quality of life in nonoperated patients with adolescent idiopathic scoliosis in the middle years: a mean 25-year follow-up study. Spine (Phila Pa 1976) 45(2):E83–E89. https://doi.org/10.1097/BRS.0000000000003216
Erwin J, Carlson BB, Bunch J, Jackson RS, Burton D (2020) Impact of unoperated adolescent idiopathic scoliosis in adulthood: a 10-year analysis. Spine Deform 8(5):1009–1016. https://doi.org/10.1007/s43390-020-00142-0
Ersen O, Ozyurek S, Ekinci S, Bilgic S, Koca K, Oguz E, Sehirlioglu A (2013) Are distal fusion level and quality of life related in adolescent scoliosis? J Turk Spinal Surg 24:111–116
Asher M, Min Lai S, Burton D, Manna B (2003) The reliability and concurrent validity of the scoliosis research society-22 patient questionnaire for idiopathic scoliosis. Spine (Phila Pa 1976) 28(1):63–69. https://doi.org/10.1097/00007632-200301010-00015
Alanay A, Cil A, Berk H, Acaroglu RE, Yazici M, Akcali O, Kosay C, Genc Y, Surat A (2005) Reliability and validity of adapted Turkish Version of Scoliosis Research Society-22 (SRS-22) questionnaire. Spine (Phila Pa 1976) 30(21):2464–2468. https://doi.org/10.1097/01.brs.0000184366.71761.84
Danielsson AJ, Hasserius R, Ohlin A, Nachemson AL (2010) Health-related quality of life in untreated versus brace-treated patients with adolescent idiopathic scoliosis: a long-term follow-up. Spine (Phila Pa 1976) 35(2):199–205. https://doi.org/10.1097/BRS.0b013e3181c89f4a
Baldus C, Bridwell KH, Harrast J, Edwards C 2nd, Glassman S, Horton W, Lenke LG, Lowe T, Mardjetko S, Ondra S, Schwab F, Shaffrey C (2008) Age-gender matched comparison of SRS instrument scores between adult deformity and normal adults: are all SRS domains disease specific? Spine (Phila Pa 1976) 33(20):2214–2218. https://doi.org/10.1097/BRS.0b013e31817c0466
Bridwell KH, Cats-Baril W, Harrast J, Berven S, Glassman S, Farcy JP, Horton WC, Lenke LG, Baldus C, Radake T (2005) The validity of the SRS-22 instrument in an adult spinal deformity population compared with the Oswestry and SF-12: a study of response distribution, concurrent validity, internal consistency, and reliability. Spine (Phila Pa 1976) 30(4):455–461. https://doi.org/10.1097/01.brs.0000153393.82368.6b
Bridwell KH, Berven S, Glassman S, Hamill C, Horton WC 3rd, Lenke LG, Schwab F, Baldus C, Shainline M (2007) Is the SRS-22 instrument responsive to change in adult scoliosis patients having primary spinal deformity surgery? Spine (Phila Pa 1976) 32(20):2220–2205. https://doi.org/10.1097/BRS.0b013e31814cf120
Ascani E, Bartolozzi P, Logroscino CA, Marchetti PG, Ponte A, Savini R, Travaglini F, Binazzi R, Di Silvestre M (1986) Natural history of untreated idiopathic scoliosis after skeletal maturity. Spine (Phila Pa 1976) 11(8):784–789. https://doi.org/10.1097/00007632-198610000-00007.
Berven S, Deviren V, Demir-Deviren S, Hu SS, Bradford DS (2003) Studies in the modified Scoliosis Research Society Outcomes Instrument in adults: validation, reliability, and discriminatory capacity. Spine (Phila Pa 1976) 28(18):2164–2169; discussion 2169. https://doi.org/10.1097/01.BRS.0000084666.53553.D6
De La Rocha A, McClung A, Sucato DJ (2014) Increased body mass index negatively affects patient satisfaction after a posterior fusion and instrumentation for adolescent idiopathic scoliosis. Spine Deform 2(3):208–213. https://doi.org/10.1016/j.jspd.2013.12.005
Lonner BS, Toombs CS, Husain QM, Sponseller P, Shufflebarger H, Shah SA, Samdani AF, Betz RR, Cahill PJ, Yaszay B, Newton PO (2015) Body mass index in adolescent spinal deformity: comparison of Scheuermann’s Kyphosis, adolescent idiopathic scoliosis, and normal controls. Spine Deform 3(4):318–326. https://doi.org/10.1016/j.jspd.2015.02.004
Pérez-Prieto D, Sánchez-Soler JF, Martínez-Llorens J, Mojal S, Bagó J, Cáceres E, Ramírez M (2015) Poor outcomes and satisfaction in adolescent idiopathic scoliosis surgery: the relevance of the body mass index and self-image. Eur Spine J 24(2):276–280. https://doi.org/10.1007/s00586-014-3486-5
Smith JS, Shaffrey CI, Glassman SD, Carreon LY, Schwab FJ, Lafage V, Arlet V, Fu KM, Bridwell KH (2013) Spinal deformity study group. Clinical and radiographic parameters that distinguish between the best and worst outcomes of scoliosis surgery for adults. Eur Spine J 22(2):402–410. https://doi.org/10.1007/s00586-012-2547-x
Kieser DC, Wyatt MC, Boissiere L, Hayashi K, Cawley DT, Yilgor C, Larrieu D, Fujishiro T, Alanay A, Acaroglu E, Kleinstueck F, Pellisé F, Perez-Grueso FJS, Bourghli A, Vital JM, Gille O, Obeid I; European Spine Study Group (2019) The effect of increasing body mass index on the pain and function of patients with adult spinal deformity. J Spine Surg 5(4):535–540. https://doi.org/10.21037/jss.2019.11.12
Heuch I, Heuch I, Hagen K, Zwart JA (2013) Body mass index as a risk factor for develo** chronic low back pain: a followup in the Nord-Trøndelag Health Study. Spine (Phila Pa 1976) 38:133–139. https://doi.org/10.1097/BRS.0b013e3182647af2
Li J, Tseng C, Yuan Y, Jiang D, Qian Z, Hu Z, Zhu Z, Qiu Y, Liu Z (2021) Determining the association between the radiographic parameters and the SRS-22 scores in Chinese female patients with adolescent idiopathic scoliosis: does curve pattern matter? Br J Neurosurg 25:1–7. https://doi.org/10.1080/02688697.2021.1875396
Fortin C, Grunstein E, Labelle H, Parent S, Ehrmann Feldman D (2016) Trunk imbalance in adolescent idiopathic scoliosis. Spine J 16(6):687–693. https://doi.org/10.1016/j.spinee.2016.02.033
Ward WT, Friel NA, Kenkre TS, Brooks MM, Londino JA, Roach JW (2017) SRS-22r scores in nonoperated adolescent idiopathic scoliosis patients with curves greater than forty degrees. Spine (Phila Pa 1976) 42(16):1233–1240. https://doi.org/10.1097/BRS.0000000000002004
Misterska E, Glowacki M, Latuszewska J, Adamczyk K (2013) Perception of stress level, trunk appearance, body function and mental health in females with adolescent idiopathic scoliosis treated conservatively: a longitudinal analysis. Qual Life Res 22(7):1633–1645. https://doi.org/10.1007/s11136-012-0316-2
Matamalas A, Bagó J, D’Agata E, Pellisé F (2016) Does patient perception of shoulder balance correlate with clinical balance? Eur Spine J 25(11):3560–3567. https://doi.org/10.1007/s00586-015-3971-5
Ono T, Bastrom TP, Newton PO (2012) Defining 2 components of shoulder imbalance: clavicle tilt and trapezial prominence. Spine (Phila Pa 1976) 37(24):E1511–E1516. https://doi.org/10.1097/BRS.0b013e31826e2bbb
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by OE and UY. The first draft of the manuscript was written by OE and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Erşen, Ö., Yüzügüldü, U., Başak, A.M. et al. Effect of clinical and radiological parameters on the quality of life in adult patients with untreated adolescent idiopathic scoliosis: a cross-sectional study. Eur Spine J 32, 1196–1203 (2023). https://doi.org/10.1007/s00586-023-07571-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07571-1