Abstract
Background
A novel morphological classification using resected specimens predicted malignant potential and prognosis in patients with pancreatic neuroendocrine tumors (P-NETs). The aim of this study was to examine the predictive ability of morphological diagnoses made using non-invasive multi-detector computed tomography (MDCT) in P-NETs.
Methods
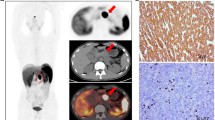
Between 2002 and 2015, 154 patients were diagnosed with P-NETs at the Tokyo Medical and Dental University, and 82 patients who underwent surgical treatment were enrolled. The primary tumors were classified by MDCT into three types: Type I, simple nodular tumor; Type II, simple nodular tumor with extra-nodular growth; and Type III, confluent multinodular tumor. Patients were stratified by 15 clinical specialists according to classification and without any other clinical or pathological information. Clinicopathological features and patient survival were reviewed retrospectively.
Results
The mean observation time was 1004 days. Forty-six, 22, and 14 patients had Type I, II, and III tumors, respectively. Morphological classification was significantly correlated with advanced features such as tumor size, Ki-67 index, and synchronous liver metastasis (p < 0.001 for all). There were significant differences between all three tumor types as judged by ENETS TNM classification (p < 0.001), AJCC TNM classification (p = 0.046), WHO 2004 classification (p < 0.001), and WHO 2010 classification (p < 0.001). Five-year progression-free survival (PFS) rates for patients with Type I, II, and III tumors were 97, 43, and 31%, respectively (I vs. II, p < 0.001; I vs. III, p < 0.001; II vs. III, p = 0.017). Multivariate analysis revealed Type II/III tumors and synchronous liver metastasis to be independent risk factors for poor PFS.
Conclusion
A novel simple morphological classification system would predict Type II and III tumors that may have higher malignant potential than Type I tumors.



Similar content being viewed by others
References
Klimstra DS, Modlin IR, Coppola D, et al. The pathologic classification of neuroendocrine tumors: a review of nomenclature, grading, and staging systems. Pancreas. 2010;39:707–12.
Yao JC, Hassan M, Phan A, et al. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008;26:3063–72.
Ito T, Igarashi H, Nakamura K, et al. Epidemiological trends of pancreatic and gastrointestinal neuroendocrine tumors in Japan: a nationwide survey analysis. J Gastroenterol. 2015;50:58–64.
Ito T, Igarashi H, Jensen RT. Therapy of metastatic pancreatic neuroendocrine tumors (pNETs): recent insights and advances. J Gastroenterol. 2012;47:941–60.
Kloppel G. Classification and pathology of gastroenteropancreatic neuroendocrine neoplasms. Endocr Relat Cancer. 2011;18(Suppl 1):S1–16.
Falconi M, Bartsch DK, Eriksson B, et al. ENETS Consensus Guidelines for the management of patients with digestive neuroendocrine neoplasms of the digestive system: well-differentiated pancreatic non-functioning tumors. Neuroendocrinology. 2012;95:120–34.
Rindi G, Arnold R, Bosman FT, et al. Nomenclature and classification of neuroendocrine neoplasms of the digestive system. In: Bosman FT, Carneiro F, Hruban RH, Theise ND, editors. WHO classification of tumours of the digestive system. Lyon: IARC Press; 2010. pp.13–14.
Katsuta E, Kudo A, Akashi T, et al. Macroscopic morphology for estimation of malignant potential in pancreatic neuroendocrine neoplasm. J Cancer Res Clin Oncol. 2016;142:1299–306.
Nakayama H, Takayama T, Okubo T, et al. Proposal of objective morphological classification system for hepatocellular carcinoma using preoperative multiphase computed tomography. J Gastroenterol. 2014;49:1430–7.
Inayoshi J, Ichida T, Sugitani S, et al. Gross appearance of hepatocellular carcinoma reflects E-cadherin expression and risk of early recurrence after surgical treatment. J Gastroenterol Hepatol. 2003;18:673–7.
Nagano Y, Shimada H, Takeda K, et al. Predictive factors of microvascular invasion in patients with hepatocellular carcinoma larger than 5 cm. World J Surg. 2008;32:2218–22.
Shimada M, Rikimaru T, Hamatsu T, et al. The role of macroscopic classification in nodular-type hepatocellular carcinoma. Am J Surg. 2001;182:177–82.
Murakata A, Tanaka S, Mogushi K, et al. Gene expression signature of the gross morphology in hepatocellular carcinoma. Ann Surg. 2011;253:94–100.
Horton KM, Hruban RH, Yeo C, Fishman EK. Multi-detector row CT of pancreatic islet cell tumors. Radiographics. 2006;26:453–64.
Rodallec M, Vilgrain V, Couvelard A, et al. Endocrine pancreatic tumours and helical CT: contrast enhancement is correlated with microvascular density, histoprognostic factors and survival. Pancreatology. 2006;6:77–85.
d’Assignies G, Couvelard A, Bahrami S, et al. Pancreatic endocrine tumors: tumor blood flow assessed with perfusion CT reflects angiogenesis and correlates with prognostic factors. Radiology. 2009;250:407–16.
Yamada S, Fujii T, Suzuki K, et al. Preoperative identification of a prognostic factor for pancreatic neuroendocrine tumors using multiphase contrast-enhanced computed tomography. Pancreas. 2016;45:198–203.
Luo G, Javed A, Strosberg JR, et al. Modified staging classification for pancreatic neuroendocrine tumors on the basis of the american joint committee on cancer and european neuroendocrine tumor society systems. J Clin Oncol. 2017;35:274–80.
Acknowledgments
This work was supported by Grant-in-Aid for Scientific Research (C) Grant Number 15K10046.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
535_2017_1349_MOESM2_ESM.tif
Supplementary figure Overall survival rates of non-surgical patients with pancreatic neuroendocrine tumors according to morphological classification. Note the significant difference between Types I and III (TIFF 6604 kb)
Rights and permissions
About this article
Cite this article
Oba, A., Kudo, A., Akahoshi, K. et al. A simple morphological classification to estimate the malignant potential of pancreatic neuroendocrine tumors. J Gastroenterol 52, 1140–1146 (2017). https://doi.org/10.1007/s00535-017-1349-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-017-1349-7