Abstract
Purpose
This study was aimed at exploring the type and role of relationships between sexual function, sense of coherence (SOC), and well-being in a sample of Iranian breast cancer survivors.
Methods
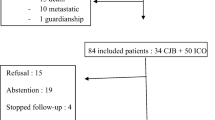
In this cross-sectional study with correlational design, data were collected from 181 survivors by consecutive sampling. They answered demographic and clinical information sheet, the SOC scale, the Female Sexual Function Index (FSFI), and the Health Index (HI). The data were analyzed using SPSS version 20.
Results
The mean age of survivors was 47.04 ± 9.05 years. Most survivors were menopausal (51.9%) and underwent mastectomy (69.1%), and 12 months or more had passed since their treatment ended (71.2%). Sexual function was positively correlated with the level of SOC (r = 0.20) and the HI (r = 0.33). Also, there was a positive correlation between the level of SOC and the HI (r = 0.51). The results of logistic regression analyses showed the protective role of the SOC (OR: 0.95; 95% CI: 0.92–0.97) and the HI (OR: 0.87; 95% CI: 0.79–0.96) for women’s sexual function. According to these results, the mediating role of the SOC was assessed between the variables of the HI and the FSFI. The SOC revealed a complete mediating effect in this relationship.
Conclusions
The mediator role of the SOC between survivors’ well-being and their sexual function helps nurses and clinicians to understand how the SOC can be used as a screening test to detect survivors who are at risk of sexual problems and to plan for salutogenic interventions.
Similar content being viewed by others
References
WHO. Breast cancer: prevention and control. Available: https://www.who.int/cancer/detection/breastcancer/en/index1.html. Accessed 20 Sept 2020
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Parks R, Derks M, Bastiaannet E, Cheung K. Breast cancer epidemiology. Breast cancer management for surgeons: Springer; 2018. p. 19–29
Boquiren VM, Esplen MJ, Wong J, Toner B, Warner E, Malik N (2016) Sexual functioning in breast cancer survivors experiencing body image disturbance. Psycho-Oncology. 25(1):66–76
Dow J, Kennedy SL (2015) Breast cancer survivors and sexuality: a review of the literature concerning sexual functioning, assessment tools, and evidence-based interventions. Clin J Oncol Nurs 19(4)
Rosen CB, Heiman J, Leiblum S, Meston C, Shabsigh R, Ferguson D, D’Agostino R (2000) The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther 26(2):191–208
Boehmer U, Ozonoff A, Timm A, Winter M, Potter J (2014) After breast cancer: sexual functioning of sexual minority survivors. J Sex Res 51(6):681–689
Cobo-Cuenca AI, Martín-Espinosa NM, Sampietro-Crespo A, Rodríguez-Borrego MA, Carmona-Torres JM (2018) Sexual dysfunction in Spanish women with breast cancer. PLoS One 13(8):e0203151
Gandhi C, Butler E, Pesek S, Kwait R, Edmonson D, Raker C, Clark MA, Stuckey A, Gass J (2019) Sexual dysfunction in breast cancer survivors. Am J Clin Oncol 42(6):500–506
Hummel SB, Hahn DE, van Lankveld JJ, Oldenburg HS, Broomans E, Aaronson NK (2017) Factors associated with specific diagnostic and statistical manual of mental disorders, sexual dysfunctions in breast cancer survivors: a study of patients and their partners. J Sex Med 14(10):1248–1259
Panjari M, Bell RJ, Davis SR (2011) Sexual function after breast cancer. J Sex Med 8(1):294–302
Masjoudi M, Keshavarz Z, Akbari ME, Kashani FL (2019) Evaluation of sexual function in breast cancer survivors using female sexual function index: a systematic review. Int J Women’s Health Reprod Sci 7(4):434–441
Carroll AJ, Baron SR, Carroll RA (2016) Couple-based treatment for sexual problems following breast cancer: a review and synthesis of the literature. Support Care Cancer 24(8):3651–3659
Kvillemo P, Bränström R (2014) Co** with breast cancer: a meta-analysis. PLoS One 9(11):e112733
Antonovsky A (1987) Unraveling the mystery of health: how people manage stress and stay well. Jossey-Bass Publishers, San Francisco
Rohani C, Abedi H-A, Omranipour R, Langius-Eklöf A (2015) Health-related quality of life and the predictive role of sense of coherence, spirituality and religious co** in a sample of Iranian women with breast cancer: a prospective study with comparative design. Health Qual Life Outcomes 13(1):40
Antonovsky A (1996) The salutogenic model as a theory to guide health promotion. Health Promot Int 11(1):11–18
Anyfantakis D, Symvoulakis EK, Linardakis M, Shea S, Panagiotakos D, Lionis C (2015) Effect of religiosity/spirituality and sense of coherence on depression within a rural population in Greece: the Spili III project. BMC Psychiatry 15(1):173
Eriksson M, Lindström B (2006) Antonovsky’s sense of coherence scale and the relation with health: a systematic review. J Epidemiol Community Health 60(5):376–381
Drageset J, Nygaard HA, Eide GE, Bondevik M, Nortvedt MW, Natvig GK (2008) Sense of coherence as a resource in relation to health-related quality of life among mentally intact nursing home residents–a questionnaire study. Health Qual Life Outcomes 6(1):85
Quintard B, Constant A, Lakdja F, Labeyrie-Lagardère H (2014) Factors predicting sexual functioning in patients 3 months after surgical procedures for breast cancer: the role of the sense of coherence. Eur J Oncol Nurs 18(1):41–45
Jabłoński MJ, Mirucka B, Streb J, Słowik AJ, Jach R (2019) Factors predicting health-related quality of life in breast cancer survivors: the role of sense of coherence. Psychiatr Psychol Klin 19(1):25–31
Fatehi S, Maasoumi R, Atashsokhan G, Hamidzadeh A, Janbabaei G, Mirrezaie SM (2019) The effects of psychosexual counseling on sexual quality of life and function in Iranian breast cancer survivors: a randomized controlled trial. Breast Cancer Res Treat 175(1):171–179
Rosenberg SM, Tamimi RM, Gelber S, Ruddy KJ, Bober SL, Kereakoglow S, Borges VF, Come SE, Schapira L, Partridge AH (2014) Treatment-related amenorrhea and sexual functioning in young breast cancer survivors. Cancer. 120(15):2264–2271
Phillips D (2006) Quality of life: concept, policy and practice, 1st edn. Rutledge, London
Topp CW, Østergaard SD, Søndergaard S, Bech P (2015) The WHO-5 Well-Being Index: a systematic review of the literature. Psychother Psychosom 84(3):167–176
Cheung SY, Delfabbro P (2016) Are you a cancer survivor? A review on cancer identity. J Cancer Surviv 10(4):759–771
Thomas R, Gifford W, Hammond C (2017) Writing toward well-being: a qualitative study of community-based workshops with breast cancer survivors. Can Oncol Nurs J 27(2):178–185
Bazzi AR, Clark MA, Winter MR, Ozonoff A, Boehmer U (2018) Resilience among breast Cancer survivors of different sexual orientations. LGBT Health 5(5):295–302
Abu-Helalah M, Al-Hanaqta M, Alshraideh H, Abdulbaqi N, Hijazeen J (2014) Quality of life and psychological well-being of breast cancer survivors in Jordan. Asian Pac J Cancer Prev 15(14):5927–5936
Akyuz MD, Turfan EC, Oner SC, Sakar T, Aktay DM (2020) Sexual functions in pregnancy: different situations in near geography: a case study on Turkey, Iran and Greece. J Matern Fetal Neonatal Med 33(2):222–229
Runowicz CD, Leach CR, Henry NL, Henry KS, Mackey HT, Cowens-Alvarado RL, Cannady RS, Pratt-Chapman ML, Edge SB, Jacobs LA, Hurria A, Marks LB, LaMonte S, Warner E, Lyman GH, Ganz PA (2016) American Cancer Society/American Society of Clinical Oncology breast cancer survivorship care guideline. CA Cancer J Clin 66(1):43–73
Sarenmalm EK, Browall M, Persson LO, Fall-Dickson J, Gaston-Johansson F (2013) Relationship of sense of coherence to stressful events, co** strategies, health status, and quality of life in women with breast cancer. Psycho-oncology. 22(1):20–27
Wiegel M, Meston C, Rosen R (2005) The female sexual function index (FSFI): cross-validation and development of clinical cutoff scores. J Sex Marital Ther 31(1):1–20
Baser RE, Li Y, Carter J (2012) Psychometric validation of the Female Sexual Function Index (FSFI) in cancer survivors. Cancer. 118(18):4606–4618
Mohamadi KH, Heydari M, Faghihezade S (2008) The Female Sexual Function Index (FSFI): validation of the Iranian version. PAYESH. 7(3):269–278
WHO (2015) Process of translation and adaptation of instruments Available from: http://wwww.hoint/substance_abuse/research_tools/translation/e
Eriksson M, Lindström B (2005) Validity of Antonovsky’s sense of coherence scale: a systematic review. J Epidemiol Community Health 59(6):460–466
Rohani C, Khanjari S, Abedi HA, Oskouie F, Langius-Eklöf A (2010) Health index, sense of coherence scale, brief religious co** scale and spiritual perspective scale: psychometric properties. J Adv Nurs 66(12):2796–2806
Nordström G, Nyman CR, Theorell T (1992) Psychosocial adjustment and general state of health in patients with ileal conduit urinary diversion. Scand J Urol Nephrol 26(2):139–147
Baron RM, Kenny DA (1986) The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 51(6):1173–1182
Preacher KJ, Hayes AF (2008) Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods 40(3):879–891
Austin PC (2008) Using the bootstrap to improve estimation and confidence intervals for regression coefficients selected using backwards variable elimination. Stat Med 27(17):3286–3300
Rohani C, Abedi H-A, Sundberg K, Langius-Eklöf A (2015) Sense of coherence as a mediator of health-related quality of life dimensions in patients with breast cancer: a longitudinal study with prospective design. Health Qual Life Outcomes 13(1):195
Brassard A, Dupuy E, Bergeron S, Shaver PR (2015) Attachment insecurities and women’s sexual function and satisfaction: the mediating roles of sexual self-esteem, sexual anxiety, and sexual assertiveness. J Sex Res 52(1):110–119
Simon J, Davis S, Althof S, Chedraui P, Clayton A, Kingsberg S et al (2018) Sexual well-being after menopause: an international menopause society white paper. Climacteric. 21(5):415–427
Nilsson KW, Leppert J, Simonsson B, Starrin B (2010) Sense of coherence and psychological well-being: improvement with age. J Epidemiol Community Health 64(4):347–352
von Humboldt S, Leal I, Pimenta F (2015) Sense of coherence, sociodemographic, lifestyle, and health-related factors in older adults’ subjective well-being. Int J Gerontol 9(1):15–19
Grevenstein D, Bluemke M (2015) Can the Big Five explain the criterion validity of Sense of Coherence for mental health, life satisfaction, and personal distress? Personal Individ Differ 77:106–111
Smith PM, Breslin FC, Beaton DE (2003) Questioning the stability of sense of coherence. Soc Psychiatry Psychiatr Epidemiol 38(9):475–484
Lindblad C, Sandelin K, Petersson L-M, Rohani C, Langius-Eklöf A (2016) Stability of the 13-item sense of coherence (SOC) scale: a longitudinal prospective study in women treated for breast cancer. Qual Life Res 25(3):753–760
Shandiz FH, Karimi FZ, Rahimi N, Abdolahi M, Khosravi Anbaran Z, Ghasemi M et al (2017) Investigating sexual function and affecting factors in women with breast cancer in Iran. Asian Pac J Cancer Prev 17(7):3583–3586
Garrido Oyarzún MF, Castelo-Branco C (2017) Use of hormone therapy for menopausal symptoms and quality of life in breast cancer survivors. Safe and ethical? Gynecol Endocrinol 33(1):10–15
Gerasimčik-Pulko V, Pileckaitė-Markovienė M, Bulotienė G, Ostapenko V (2009) Relationship between sense of coherence and quality of life in early stage breast cancer patients. Acta Med Lituanica 16(3):139–144
Acknowledgments
The present study is the result of the Master Thesis in Community Health Nursing of the first author (Fatemeh Lashani). The thesis was supervised by Dr. Camelia Rohani. The authors thank and appreciate all breast cancer survivors who participated in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Research ethics approval and consent to conduct the project were obtained. The registration code of research ethics was obtained from the Shahid Beheshti University of Medical Sciences (IR.SBMU.PHARMACY.1397.267). Informed oral and written consent was obtained from all breast cancer survivors.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lashani, F., Rohani, C., Estebsari, F. et al. Exploring the relationship between sexual function, sense of coherence, and well-being in a sample of Iranian breast cancer survivors. Support Care Cancer 29, 3191–3199 (2021). https://doi.org/10.1007/s00520-020-05831-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05831-0