Abstract
Introduction
Convalescence after hernia repair is one of the main focuses for hernia surgeons. We analyzed our prospectively collected data to identify possible predictive factors for post-operative acute and chronic pain.
Materials and methods
We prospectively collected the demographic data and peri-operative findings. Post-operative acute pain was evaluated with Visual Analog Pain Scale. The chronic pain (pain persists for > 6 months since operation) was also recorded.
Results
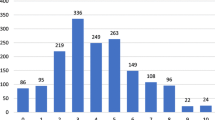
From June 2008 to August 2018, there were 807 patients with 1029 sites of inguinal hernia enrolled in our analysis. Pain before operation was associated with the severity of acute pain on OP (operation) day, POD 1 (post-operative day 1), and POD 7 (post-operative day 7). Younger patients had significantly higher post-operative acute pain on OP day, POD 1, and POD 7. The staple mesh fixation method resulted in a higher pain score at OP day and POD 1. The predictive factors for chronic pain were sex (female), young age (< 65 years), having no past history of hypertension, pain before operation, and mesh material.
Conclusion
A younger age and inguinal pain before operation were the main predictive factors for higher post-operative pain. Younger patients, females, having inguinal pain before surgery, and using heavy weight mesh have a higher risk of chronic pain.

Similar content being viewed by others
References
(2018) International guidelines for groin hernia management. Hernia 22:1–165
Perkins FM, Kehlet H (2000) Chronic pain as an outcome of surgery. A review of predictive factors. Anesthesiology 93:1123–1133
Racine M, Tousignant-Laflamme Y, Kloda LA, Dion D, Dupuis G, Choiniere M (2012) A systematic literature review of 10 years of research on sex/gender and experimental pain perception—part 1: are there really differences between women and men? Pain 153:602–618
Chan MS, Teoh AY, Chan KW, Tang YC, Ng EK, Leong HT (2014) Randomized double-blinded prospective trial of fibrin sealant spray versus mechanical stapling in laparoscopic total extraperitoneal hernioplasty. Ann Surg 259:432–437
Olmi S, Scaini A, Erba L, Guaglio M, Croce E (2007) Quantification of pain in laparoscopic transabdominal preperitoneal (TAPP) inguinal hernioplasty identifies marked differences between prosthesis fixation systems. Surgery 142:40–46
Taylor C, Layani L, Liew V, Ghusn M, Crampton N, White S (2008) Laparoscopic inguinal hernia repair without mesh fixation, early results of a large randomised clinical trial. Surg Endosc 22:757–762
Ip HY, Abrishami A, Peng PW, Wong J, Chung F (2009) Predictors of postoperative pain and analgesic consumption: a qualitative systematic review. Anesthesiology 111:657–677
Ferzli GS, Edwards E, Al-Khoury G, Hardin R (2008) Postherniorrhaphy groin pain and how to avoid it. Surg Clin N Am 88:203–216
Tolver MA, Rosenberg J, Bisgaard T (2012) Early pain after laparoscopic inguinal hernia repair. A qualitative systematic review. Acta Anaesthesiol Scand 56:549–557
Lau H, Patil NG (2004) Acute pain after endoscopic totally extraperitoneal (TEP) inguinal hernioplasty: multivariate analysis of predictive factors. Surg Endosc 18:92–96
Tolver MA, Strandfelt P, Rosenberg J, Bisgaard T (2013) Female gender is a risk factor for pain, discomfort, and fatigue after laparoscopic groin hernia repair. Hernia 17:321–327
Bartley EJ, Fillingim RB (2013) Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth 111:52–58
Niesters M, Dahan A, Kest B, Zacny J, Stijnen T, Aarts L, Sarton E (2010) Do sex differences exist in opioid analgesia? A systematic review and meta-analysis of human experimental and clinical studies. Pain 151:61–68
Chowbey PK, Garg N, Sharma A, Khullar R, Soni V, Baijal M, Mittal T (2010) Prospective randomized clinical trial comparing lightweight mesh and heavyweight polypropylene mesh in endoscopic totally extraperitoneal groin hernia repair. Surg Endosc 24:3073–3079
Arora S, Chhabra A, Subramaniam R, Arora MK, Misra MC, Bansal VK (2016) Transversus abdominis plane block for laparoscopic inguinal hernia repair: a randomized trial. J Clin Anesth 33:357–364
Takebayashi K, Matsumura M, Kawai Y, Hoashi T, Katsura N, Fukuda S, Shimizu K, Inada T, Sato M (2015) Efficacy of transversus abdominis plane block and rectus sheath block in laparoscopic inguinal hernia surgery. Int Surg 100:666–671
Mughal A, Khan A, Rehman J, Naseem H, Waldron R, Duggan M, Khan W, Barry K, Khan IZ (2018) Laparoscopic-assisted transversus abdominis plane block as an effective analgesic in total extraperitoneal inguinal hernia repair: a double-blind, randomized controlled trial. Hernia 22:821–826
Sajid MS, Ladwa N, Kalra L, McFall M, Baig MK, Sains P (2013) A meta-analysis examining the use of tacker mesh fixation versus glue mesh fixation in laparoscopic inguinal hernia repair. Am J Surg 206:103–111
Lo CW, Tsai YC, Yang SS, Hsieh CH, Chang SJ (2019) Comparison of short- to mid-term efficacy of nonfixation and permanent tack fixation in laparoscopic total extraperitoneal hernia repair: a systematic review and meta-analysis. Ci Ji Yi Xue Za Zhi 31:244–253
Niebuhr H, Wegner F, Hukauf M, Lechner M, Fortelny R, Bittner R, Schug-Pass C, Kockerling F (2018) What are the influencing factors for chronic pain following TAPP inguinal hernia repair: an analysis of 20,004 patients from the Herniamed Registry. Surg Endosc 32:1971–1983
Andresen K, Fenger AQ, Burcharth J, Pommergaard HC, Rosenberg J (2017) Mesh fixation methods and chronic pain after transabdominal preperitoneal (TAPP) inguinal hernia surgery: a comparison between fibrin sealant and tacks. Surg Endosc 31:4077–4084
Currie A, Andrew H, Tonsi A, Hurley PR, Taribagil S (2012) Lightweight versus heavyweight mesh in laparoscopic inguinal hernia repair: a meta-analysis. Surg Endosc 26:2126–2133
Li J, Ji Z, Cheng T (2012) Lightweight versus heavyweight in inguinal hernia repair: a meta-analysis. Hernia 16:529–539
Fortelny RH, Petter-Puchner AH, May C, Jaksch W, Benesch T, Khakpour Z, Redl H, Glaser KS (2012) The impact of atraumatic fibrin sealant vs. staple mesh fixation in TAPP hernia repair on chronic pain and quality of life: results of a randomized controlled study. Surg Endosc 26:249–254
Kaul A, Hutfless S, Le H, Hamed SA, Tymitz K, Nguyen H, Marohn MR (2012) Staple versus fibrin glue fixation in laparoscopic total extraperitoneal repair of inguinal hernia: a systematic review and meta-analysis. Surg Endosc 26:1269–1278
Shah NS, Fullwood C, Siriwardena AK, Sheen AJ (2014) Mesh fixation at laparoscopic inguinal hernia repair: a meta-analysis comparing tissue glue and tack fixation. World J Surg 38:2558–2570
Shi Z, Fan X, Zhai S, Zhong X, Huang D (2017) Fibrin glue versus staple for mesh fixation in laparoscopic transabdominal preperitoneal repair of inguinal hernia: a meta-analysis and systematic review. Surg Endosc 31:527–537
Bugada D, Lavand'homme P, Ambrosoli AL, Cappelleri G, Saccani Jotti GM, Meschi T, Fanelli G, Allegri M (2016) Effect of preoperative inflammatory status and comorbidities on pain resolution and persistent postsurgical pain after inguinal hernia repair. Mediators Inflamm 2016:5830347
Nukada H, Baba M, Ogasawara S, McMorran D, Yagihashi S (2016) Neuropathy in the spontaneously hypertensive rat: an electrophysiological and histological study. Muscle Nerve 54:756–762
Fontanesi LB, Fazan FS, Dias FJ, Schiavoni MCL, Marques W Jr, Fazan VPS (2019) Sensory and motor conduction velocity in spontaneously hypertensive rats: sex and aging investigation. Front Syst Neurosci 13:62
Sacco M, Meschi M, Regolisti G, Detrenis S, Bianchi L, Bertorelli M, Pioli S, Magnano A, Spagnoli F, Giuri PG, Fiaccadori E, Caiazza A (2013) The relationship between blood pressure and pain. J Clin Hypertens (Greenwich) 15:600–605
Emdin CA, Anderson SG, Callender T, Conrad N, Salimi-Khorshidi G, Mohseni H, Woodward M, Rahimi K (2015) Usual blood pressure, peripheral arterial disease, and vascular risk: cohort study of 4.2 million adults. BMJ 351:h4865
Edwards L, Ring C, McIntyre D, Winer JB, Martin U (2008) Cutaneous sensibility and peripheral nerve function in patients with unmedicated essential hypertension. Psychophysiology 45:141–147
Franneby U, Sandblom G, Nordin P, Nyren O, Gunnarsson U (2006) Risk factors for long-term pain after hernia surgery. Ann Surg 244:212–219
Hoffmann H, Walther D, Bittner R, Kockerling F, Adolf D, Kirchhoff P (2018) Smaller inguinal hernias are independent risk factors for develo** chronic postoperative inguinal pain (CPIP): a registry-based multivariable analysis of 57, 999 patients. Ann Surg. https://doi.org/10.1097/sla.0000000000003065
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Chi-Wen Lo, Yung-Tai Chen, Fu-Shan Jaw, Chih-Chin Yu, and Yao-Chou Tsai have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lo, CW., Chen, YT., Jaw, FS. et al. Predictive factors of post-laparoscopic inguinal hernia acute and chronic pain: prospective follow-up of 807 patients from a single experienced surgeon. Surg Endosc 35, 148–158 (2021). https://doi.org/10.1007/s00464-020-07373-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07373-2