Abstract
Introduction
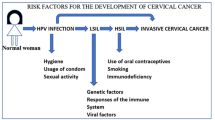
Persistent Human Papillomavirus (HPV) infection is linked to 99% of cervical cancer (CC) cases. HPV types 16 and 18 alone result in 75% of CC cases and thus are considered to be high-risk types (HR-HPV). CC is the third most common cancer among women globally. Approximately, 7000 patients die from it yearly. It is worthy to note that not every patient with HPV precancerous lesions will progress to CC.
Objectives
The objectives of this review is to explore the utilization of molecular and viral biomarkers as a tool for early detection and prediction of HPV-induced cervical lesions that might progress to CC.
Methods
The data bases PubMed, Google Scholar, EBSCO were searched using keywords CC screening, HPV, and recent molecular biomarkers. The search time frame was within the last 7 years. Studies on HPV-induced cancers other than CC were excluded; a total of 200 eligible articles were retrieved.
Results
In this review we explored the current literature about HPV virology, virulence genes and early diagnostic/prognostic molecular biomarkers in CC. The oncogenic property of HPV is attributed to viral expression of various early proteins (E5, E6, E7). The interaction between viral oncoproteins and the cellular genetic apparatus alters the expression of many genes at different phases of the disease. There was an association between cervical lesions induced by HR-HPV and the overexpression of markers of oxidative DNA damage and other proteins. The markers p16INK4a, programmed cell death-1 (PD-1)/programmed cell death ligand 1, mismatch repair enzymes (MMR), miRNA-377, claudin family (CLDN) are dysregulated and are associated with high risk lesions. Furthermore, advanced older cervical lesions were associated with high methylation levels and higher risk to progress to CC.
Conclusion
Adding different the above markers to the CC screening program scheme might offer a triage for prioritizing patient management.




Similar content being viewed by others
Data availability
No data are available.
References
Al-Awadhi R, Chehadeh W, Jaragh M, Al-Shaheen A, Sharma P, Kapila K (2011) Distribution of human papillomavirus among women with abnormal cervical cytology in Kuwait. Diagn Cytopathol 41:107–114. https://doi.org/10.1002/dc.21778
Albert E, Laimins L (2020) Regulation of the human papillomavirus life cycle by DNA damage repair pathways and epigenetic factors. Viruses 12:744. https://doi.org/10.3390/v12070744
Arbyn M, Weiderpass E, Bruni L, de Sanjosé S, Saraiya M, Ferlay J, Bray F (2019) Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health 8:E191–E203. https://doi.org/10.1016/s2214-109x(19)30482-6
Bhat AA, Syed N, Therachiyil L, Nisar S, Hashem S, Macha MA, Yadav SK, Krishnankutty R, Muralitharan S, Al-Naemi H, Bagga P, Reddy R, Dhawan P, Akobeng A, Uddin S, Frenneaux MP, El-Rifai W, Haris M (2020) Claudin-1, a double-edged sword in cancer. Int J Mol Sci 21:569. https://doi.org/10.3390/ijms21020569
Bonde J, Floore A, Ejegod D, Vink FJ, Hesselink A, Ven PM, Valenčak AO, Pedersen H, Doorn S, Quint WG, Petry KU, Poljak M, Stanczuk G, Cuschieri K, Sanjosé S, Bleeker M, Berkhof J, Meijer CJLM, Heideman DAM (2020) Methylation markers FAM19A4 and miR124-2 as triage strategy for primary human papillomavirus screen positive women: a large European multicenter study. Int J Cancer 148:396–405. https://doi.org/10.1002/ijc.33320
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J Clin 68:394–424. https://doi.org/10.3322/caac.21492
CDC , HPV Vaccine Information For Young Women. https://www.cdc.gov/std/hpv/stdfact-hpv-vaccine-young-women.htm. Accessed 26 June 2021
Chrysostomou A, Stylianou D, Constantinidou A, Kostrikis L (2018) Cervical cancer screening programs in Europe: the transition towards HPV vaccination and population-based HPV testing. Viruses 10:729. https://doi.org/10.3390/v10120729
Czogalla B, Partenheimer A, Jeschke U, von Schönfeldt V, Mayr D, Mahner S, Burges A, Simoni M, Melli B, Benevelli R, Bertini S, Casarini L, Trillsch F (2020) β-arrestin 2 is a prognostic factor for survival of ovarian cancer patients upregulating cell proliferation. Front Endocrinol. https://doi.org/10.3389/fendo.2020.554733
da Mata S, Ferreira J, Nicolás I, Esteves S, Esteves G, Lérias S, Silva F, Saco A, Cochicho D, Cunha M, del Pino M, Ordi J, Félix A (2021) P16 and HPV genotype significance in HPV-associated cervical cancer—a large cohort of two tertiary referral centers. Int J Mol Sci 22:2294. https://doi.org/10.3390/ijms22052294
Deepti P, Pasha A, Kumbhakar DV, Doneti R, Heena SK, Bhanoth S, Poleboyina PK, Yadala R, Annapurna SD, Pawar SC (2022) Overexpression of secreted phosphoprotein 1 (SPP1) predicts poor survival in HPV positive cervical cancer. Gene. https://doi.org/10.1016/j.gene.2022.146381
Deshpande M, Romanski PA, Rosenwaks Z, Gerhardt J (2020) Gynecological cancers caused by deficient mismatch repair and microsatellite instability. Cancers 12:3319. https://doi.org/10.3390/cancers12113319
Dong B, Zou H, Mao X, Su Y, Gao H, ** into real-world screening on cervical cancer screening in China: a retrospective population-based cohort study. Therapeutic Adva Med Oncol. https://doi.org/10.1177/17588359211010939
Doorbar J, Egawa N, Griffin H, Kranjec C, Murakami I (2015) Human papillomavirus molecular biology and disease association. Rev Med Virol 25:2–23. https://doi.org/10.1002/rmv.1822
Eckhardt M, Zhang W, Gross AM, Dollen JV, Johnson JR, Franks-Skiba KE, Swaney DL, Johnson TL, Jang GM, Shah PS, Brand TM, Archambault J, Kreisberg JF, Grandis JR, Ideker T, Krogan NJ (2018) Multiple routes to oncogenesis are promoted by the human papillomavirus-host protein network. Cancer Discov 8:1474–1489. https://doi.org/10.1158/2159-8290.CD-17-1018
Hallowell BD, Saraiya M, Thompson TD, Unger ER, Lynch CF, Tucker T, Copeland G, Hernandez BY, Peters ES, Wilkinson E, Goodman MT (2018) Population-based assessment of HPV genotype-specific cervical cancer survival: CDC cancer registry sentinel surveillance system. JNCI Cancer Spectrum. https://doi.org/10.1093/jncics/pky036
Hasan MdE, Matin M, Haque MdE, Aziz MdA, Millat MdS, Uddin MS, Moghal MdMR, Islam MS (2021) Polymorphic variants INSIG2 rs6726538, HLA-DRB1 rs9272143, and GCNT1P5rs7780883 contribute to the susceptibility of cervical cancer in the Bangladeshi women. Cancer Med 10:1829–1838. https://doi.org/10.1002/cam4.3782
Ishikawa M, Nakayama K, Nakamura K, Yamashita H, Ishibashi T, Minamoto T, Sawada K, Yoshimura Y, Iida K, Razia S, Ishikawa N, Nakayama S, Otsuki Y, Kyo S (2021) P16INK4A expression might be associated with a favorable prognosis for cervical adenocarcinoma via dysregulation of the RB pathway. Sci Rep. https://doi.org/10.1038/s41598-021-97703-8
Kaistha BP, Honstein T, Müller V, Bielak S, Sauer M, Kreider R, Fassan M, Scarpa A, Schmees C, Volkmer H, Gress TM, Buchholz M (2014) Key role of dual specificity kinase TTK in proliferation and survival of pancreatic cancer cells. Br J Cancer 111:1780–1787. https://doi.org/10.1038/bjc.2014.460
Kremer WW, Steenbergen RDM, Heideman DAM, Kenter GG, Meijer CJLM (2021) The use of host cell DNA methylation analysis in the detection and management of women with advanced cervical intraepithelial neoplasia: a review. Obstet Gynecol Surv 76:273–274. https://doi.org/10.1097/ogx.0000000000000922
Kumar N, Gupta R, Gupta S (2019) Glandular cell abnormalities in cervical cytology: What has changed in this decade and what has not? European J Obst Gynecol Rep Biol 240:68–73. https://doi.org/10.1016/j.ejogrb.2019.06.006
Li Y, Li Y, Chen Y, **e Q, Dong N, Gao Y, Deng H, Lu C, Wang S (2017) MicroRNA-214–3p inhibits proliferation and cell cycle progression by targeting MELK in hepatocellular carcinoma and correlates cancer prognosis. Cancer Cell Int. https://doi.org/10.1186/s12935-017-0471-1
Lin J, Albers AE, Qin J, Kaufmann AM (2014) Prognostic significance of overexpressed p16ink4a in patients with cervical cancer: a meta-analysis. PLoS ONE. https://doi.org/10.1371/journal.pone.0106384
Liu W, Li L, Ye H, Tao H, He H (2018) Role of COL6A3 in colorectal cancer. Oncol Rep. https://doi.org/10.3892/or.2018.6331
Lund SA, Giachelli CM, Scatena M (2009) The role of osteopontin in inflammatory processes. J Cell Commun Signal 3:311–322. https://doi.org/10.1007/s12079-009-0068-0
Mendoza RP, Haidary T, Gabutan E, Zhou YY, Bukhari Z, Connelly C, Lee W-C, Lee Y-C, Wadgaonkar R, Agrawal R, Haseeb MA, Gupta R (2021) Mixed and nonvaccine high risk HPV types are associated with higher mortality in Black women with cervical cancer. Sci Rep 11:1–14. https://doi.org/10.1038/s41598-021-93485-1
Meng Y, Liang H, Hu J, Liu S, Hao X, Wong MSK, Li X, Hu L (2018) PD-L1 expression correlates with tumor infiltrating lymphocytes and response to neoadjuvant chemotherapy in cervical cancer. J Cancer 9:2938–2945. https://doi.org/10.7150/jca.22532
Mo M, Zhou M, Wang L, Qi L, Zhou K, Liu LF, Chen Z, Zu XB (2015) CCL21/CCR7 enhances the proliferation, migration, and invasion of human bladder cancer T24 cells. PLoS ONE 10:e0119506. https://doi.org/10.1371/journal.pone.0119506
Moody C (2017) Mechanisms by which HPV induces a replication competent environment in differentiating keratinocytes. Viruses 9:261. https://doi.org/10.3390/v9090261
Moore LD, Le T, Fan G (2012) DNA methylation and its basic function. Neuropsychopharmacology 38:23–38. https://doi.org/10.1038/npp.2012.112
Park IU, Introcaso C, Dunne EF (2015) Human papillomavirus and genital warts: a review of the evidence for the 2015 centers for disease control and prevention sexually transmitted diseases treatment guidelines. Clin Infect Dis 61:S849–S855. https://doi.org/10.1093/cid/civ813
Rahman A, Kobayashi M, Sugimoto K, Endo Y, Kojima M, Furukawa S, Watanabe T, Soeda S, Hashimoto Y, Fujimori K, Chiba H (2021) Reduced claudin-12 expression predicts poor prognosis in cervical cancer. Int J Mol Sci 22:3774. https://doi.org/10.3390/ijms22073774
Rai B, Bansal A, Singh M (2016) Human papillomavirus-associated cancers: a growing global problem. Int J Appl Basic Med Res 6:84. https://doi.org/10.4103/2229-516x.179027
Revathidevi S, Murugan AK, Nakaoka H, Inoue I, Munirajan AK (2021) APOBEC: a molecular driver in cervical cancer pathogenesis. Cancer Lett 496:104–116. https://doi.org/10.1016/j.canlet.2020.10.004
Ronco G, Dillner J, Elfström KM, Tunesi S, Snijders PJF, Arbyn M, Kitchener H, Segnan N, Gilham C, Giorgi-Rossi P, Berkhof J, Peto J, Meijer CJLM (2014) Efficacy of HPV-based screening for prevention of invasive cervical cancer: follow-up of four European randomised controlled trials. The Lancet 383:524–532. https://doi.org/10.1016/s0140-6736(13)62218-7
Saslow D, Solomon D, Lawson HW, Killackey M, Kulasingam SL, Cain J, Garcia FAR, Moriarty AT, Waxman AG, Wilbur DC, Wentzensen N, Downs LS, Spitzer M, Moscicki A-B, Franco EL, Stoler MH, Schiffman M, Castle PE, Myers ER (2012) American cancer society, American society for colposcopy and cervical pathology, and American society for clinical pathology screening guidelines for the prevention and early detection of cervical cancer. CA A Cancer J Clini 62:147–172. https://doi.org/10.3322/caac.21139
Sd A, Pasumarthi D, Pasha A, Doneti R, Botlagunta M, Pawar SC (2021) Identification of differentially expressed genes in cervical cancer patients by comparative transcriptome analysis. BioMed Res Int 2021:1–13. https://doi.org/10.1155/2021/8810074
Seong J, Ryou S, Lee J, Yoo M, Hur S, Choi B-S (2021) Enhanced disease progression due to persistent HPV-16/58 infections in Korean women: a systematic review and the Korea HPV cohort study. Virol J. https://doi.org/10.1186/s12985-021-01657-2
Sharmin S, Zohura FT, Islam MS, Shimonty A, Khan MA-A-K, Parveen R, Sharmin F, Ahsan CR, Islam ABMMK, Yasmin M (2021) Mutational profiles of marker genes of cervical carcinoma in Bangladeshi patients. BMC Cancer 21:289. https://doi.org/10.1186/s12885-021-07906-5
So KA, Kim MJ, Lee K-H, Lee I-H, Kim MK, Lee YK, Hwang C-S, Jeong MS, Kee M-K, Kang C, Cho CH, Kim SM, Hong SR, Kim KT, Lee W-C, Park JS, Kim TJ (2016) The impact of high-risk hpv genotypes other than HPV 16/18 on the natural course of abnormal cervical cytology: a korean hpv cohort study. Cancer Res Treat 48:1313–1320. https://doi.org/10.4143/crt.2016.013
Soheili M, Keyvani H, Soheili M, Nasseri S (2021) Human papilloma virus: a review study of epidemiology, carcinogenesis, diagnostic methods, and treatment of all HPV-related cancers. Med J Islamic Republic Iran. https://doi.org/10.47176/mjiri.35.65
Torres KL, Mariño JM, Pires Rocha DA, de Mello MB, de Melo Farah HH, Reis RD, Alves VD, Gomes E, Martins TR, Soares AC, de Oliveira CM (2018) Self-sampling coupled to the detection of HPV 16 and 18 E6 protein: a promising option for detection of cervical malignancies in remote areas. PLoS ONE 13:e0201262. https://doi.org/10.1371/journal.pone.0201262
Vink FJ, Dick S, Heideman DAM, De Strooper LMA, Steenbergen RDM, Lissenberg-Witte BI, Floore A, Bonde JH, Oštrbenk Valenčak A, Poljak M, Petry KU, Hillemanns P, Trommel NE, Berkhof J, Bleeker MCG, Meijer CJLM (2021) Classification of high-grade cervical intraepithelial neoplasia by p16 ink4a, Ki-67, HPV E4 and FAM19A4/miR12-methylation status demonstrates considerable heterogeneity with potential consequences for management. Int J Cancer 149:707–716. https://doi.org/10.1002/ijc.33566
Wang J, Chen L (2019) The role of miRNAs in the invasion and metastasis of cervical cancer. Bioscience Rep. https://doi.org/10.1042/BSR20181377
Wang W, Arcà E, Sinha A, Hartl K, Houwing N, Kothari S (2022) Cervical cancer screening guidelines and screening practices in 11 countries: A systematic literature review. Preventive Med Rep. https://doi.org/10.1016/j.pmedr.2022.101813
Warren C, Westrich J, Doorslaer K, Pyeon D (2017) Roles of APOBEC3A and APOBEC3B in human papillomavirus infection and disease progression. Viruses 9:233. https://doi.org/10.3390/v9080233
Weston G, Dombrowski C, Steben M, Popadiuk C, Bentley J, Adams EJ (2021) A health economic model to estimate the costs and benefits of an mRNA vs DNA high-risk HPV assay in a hypothetical HPV primary screening algorithm in Ontario Canada. Preventive Med. https://doi.org/10.1016/j.pmedr.2021.101448
**a C, Li S, Long T, Chen Z, Chan PKS, Boon SS (2021) Current updates on cancer-causing types of human papillomaviruses (HPVs) in East, Southeast, and South Asia. Cancers 13:2691. https://doi.org/10.3390/cancers13112691
Ye C, Hu Y, Wang J (2019) MicroRNA-377 targets zinc finger E-box-binding homeobox 2 to inhibit cell proliferation and invasion of cervical cancer. Oncol Res Featuring Preclin Clin Cancer Therap 27:183–192. https://doi.org/10.3727/096504018x15201124340860
Zhu Y, Liu B, Zhang P, Zhang J, Wang L (2019) LncRNA TUSC8 inhibits the invasion and migration of cervical cancer cells via miR-641/PTEN axis. Cell Biol Int 43:781–788. https://doi.org/10.1002/cbin.11152
Zou J, Wang C, Ma X, Wang E, Peng G (2017) APOBEC3B, a molecular driver of mutagenesis in human cancers. Cell Biosci. https://doi.org/10.1186/s13578-017-0156-4
ZurHausen H (1994) Molecular pathogenesis of cancer of the cervix and its causation by specific human papillomavirus types. Curr Top Microbiol Immunol 186:131–156. https://doi.org/10.1007/978-3-642-78487-3_8
Funding
The authors declare that no funds, Grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
FASA—conception and design. ZN—data acquisition and analysis. PSSA—draft revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Amin, F.A.S., Un Naher, Z. & Ali, P.S.S. Molecular markers predicting the progression and prognosis of human papillomavirus-induced cervical lesions to cervical cancer. J Cancer Res Clin Oncol 149, 8077–8086 (2023). https://doi.org/10.1007/s00432-023-04710-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-023-04710-5