Abstract
Purpose
Although immune checkpoint inhibitor monotherapy has been used as a second-line treatment in advanced non-small cell lung cancer (NSCLC), the improvement in progression-free survival (PFS) remains unsatisfactory. We investigated the feasibility of sintilimab plus chemotherapy as a second-line treatment in advanced NSCLC.
Methods
This was a phase II, single-arm, prospective study in advanced NSCLC patients who had failed standard platinum-based chemotherapy (ChiCTR1900027634, Registered 22 November 2019). Eligible patients received docetaxel 75 mg/m2 (day 1) plus sintilimab 200 mg (day 3) Q3W. Those did not progress after 4–6 cycles received sintilimab 200 mg Q3W as maintenance treatment. The primary endpoint was PFS.
Results
Forty patients were enrolled between October 2019 and October 2020. With a median follow-up of 12.2 months, the median PFS was 5.8 months, and the PFS rates at 6 and 12 months were 48% and 30%, respectively. The median overall survival (OS) was 12.6 months, with a 12-month OS rate of 62.0%. The overall response rate was 32.4%, and the disease control rate was 89.2%. The incidence of all and ≥ grade 3 treatment-related adverse events (TRAEs) were 65% (26/40) and 17.5% (7/40), respectively. No TRAEs-related permanent treatment discontinuation or death occurred. bTMB reduction at 6 weeks was associated with a longer PFS (NR vs 3.0 months, P < 0.0001).
Conclusion
This prospective phase II study in China suggested that sintilimab plus docetaxel might improve PFS and tumor response with good tolerability for Chinese patients with previously treated advanced NSCLC. bTMB reduction at 6 weeks could serve as a potential predictive biomarker for this regimen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer is the leading cause of cancer-related mortality in China, and non-small cell lung cancer (NSCLC) accounts for approximately 80–85% of all lung cancer cases (Ettinger et al. 2021; Siegel et al. 2021). More than 60% of patients with NSCLC are diagnosed with locally advanced or metastatic disease (Adizie et al. 2019; Ettinger et al. 2021) and fail to receive curative treatments. The advent of immunotherapy, immune checkpoint inhibitors (ICIs) in particular, has revolutionized the approach to NSCLC (Gandhi et al. 2018; Paz-Ares et al. 2020; Socinski et al. 2021; Reck et al. 2016). However, ICIs has not yet been widely accepted as the initial treatment of NSCLC, with approximately only 40% patients receiving first-line ICIs (Afzal et al. 2018). For later line settings, ICI monotherapy has become a new standard treatment for patients after progression on chemotherapy based on its significant overall survival benefits (Borghaei et al. 2015, 2021; Wu et al. 2019; Rittmeyer et al. 2017). However, compared with docetaxel, mono-immunotherapy did not significantly improve the median progression-free survival (mPFS) (Borghaei et al. 2015, 2021; Wu et al. 2019; Rittmeyer et al. 2017).
Recent data have highlighted the ability of chemotherapy to enhance immunogenicity and/or to break immune-resistance of the tumor and its microenvironment (Bruno et al. 2017; Wanderley et al. 2018; Suzuki et al. 2005; Welters et al. 2016; Galluzzi et al. 2020), and the potential synergistic antitumor effects of programmed death-1 (PD-1)/programmed death ligand-1 (PD-L1) inhibitors in combination with chemotherapy have been confirmed in a variety of solid tumors(Gandhi et al. 2018; Paz-Ares et al. 2020; Burtness et al. 2019; Janjigian et al. 2021). Besides, the order of administration of combination therapy has been recognized as an important factor influencing clinical outcomes. Preclinically, administration of cyclophosphamide 1 day before treatment with anticytotoxic T lymphocyte antigen 4 (CTLA-4) inhibitor achieved a favorable antitumor response, whereas reversing the order of drug administration led to the apoptosis in CD8+ T lymphocytes and attenuated the effects of anti-CTLA-4 (Iida et al. 2017). Furthermore, a biomarker analysis in breast cancer revealed that the immune-related genes that involved in PD-1/PD-L1 and T cell-mediated cytotoxicity pathways were upregulated after chemotherapy (Voorwerk et al. 2019). Altogether, these results suggested that the preceding administration of chemotherapy might improve the synergistic antitumor activity with subsequent ICIs.
Sintilimab is a recombinant fully human immunoglobulin G4 monoclonal antibody that blocks the interaction between PD-1 and PD-L1 (Gao et al. 2020; Shi et al. 2019). Previous clinical study evidence showed that sintilimab monotherapy had promising antitumor activities in patients with previously treated advanced NSCLC (Li et al. 2018). Herein, we conducted a phase II study to evaluate the efficacy and safety of a subsequent-line regimen in patients with advanced NSCLC, in which sintilimab would be administered 2 days after docetaxel.
Materials and methods
Study design and patients
This was a prospective, single-arm, phase II study investigating the efficacy and safety of sintilimab in combination with docetaxel in Chinese patients with previously treated advanced NSCLC. This trial was conducted in Shandong Cancer Hospital and Institute, China and was registered with chictr.org.cn (ChiCTR1900027634). The protocol was approved by the institutional Ethics Board and all patients provided written informed consent before enrollment.
Key inclusion criteria were: age 18–75 years; histologically or cytologically confirmed NSCLC with locally advanced, metastatic, or recurrent disease that was unresectable or unsuitable for radical concurrent chemoradiotherapy; progressed on first-line platinum-based chemotherapy; and an Eastern Cooperative Oncology Group (ECOG) performance status score ≤ 1. Patients harboring EGFR-sensitive mutations or ALK alterations must have had at least one-line of tyrosine kinase inhibitor (TKI) treatment.
Key exclusion criteria included mixed non-small cell and small cell pathological components, previous treatment with ICIs or taxanes and symptomatic brain metastasis.
Treatments
Eligible patients received docetaxel 75 mg/m2 on day 1 and sintilimab 200 mg on day 3 every three weeks (Q3W) for up to 4–6 cycles. Patients who did not progress after 4–6 cycles received sintilimab (200 mg, Q3W) as maintenance therapy until progressive disease (PD), intolerance, or up to 35 cycles. Patients with first documented PD were permitted to continue study treatment if the investigators determined that the patient could benefit from continuous treatment until PD was confirmed in subsequent examinations.
Assessment
Tumor response was assessed by investigators per the Response Evaluation Criteria for Solid Tumors (RECIST) v1.1 at baseline and every six weeks until PD. For patients who received at least one dose of the study treatment, safety was monitored continuously starting from the first dose until 30 days after the last dose of the study treatment. AEs were graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events version 5.0.
Endpoints
The primary endpoint was PFS, defined as the time from the first dose of study treatment to the first documented PD or death from any cause, whichever came first. The secondary endpoints included overall response rate (ORR), disease control rate (DCR), duration of response (DOR), time to response (TTR), OS, and safety. OS was defined as the time from the first dose of study treatment to death from any cause.
Biomarker analysis
Peripheral blood samples were collected at baseline and 6 weeks after treatment initiation for comprehensive circulating tumor DNA (ctDNA) profiling. All samples were subjected to next-generation sequencing (NGS) with a panel of 448 cancer-related genes panel (Amoy Diagnostics, **amen, China) on an Illumina NovaSeq 6000 platform (Illumina, San Diego, USA). For bTMB assessment, the total number of substitutions and indels detected was divided by the length of sequenced ctDNA (1.16 Mb). At week 6, patients who had ≥ 2 somatic variants (bTMB ≥ 1.72 mutations/Mb) were defined as ctDNA residual, while those who had ≤ 1 somatic variant (bTMB ≤ 0.86 mutations/Mb) were defined as non-ctDNA residual. Testing for PD-L1 was not mandatory in this study, and no particular agent was required.
Statistical analysis
Continuous variables were presented by medians with minimum and maximum values. Categorical variables were described by frequencies and percentages. Median PFS and OS were calculated with corresponding two-sided 95% confidence interval (CI) using Kaplan–Meier method. ORR and DCR with 95% CIs were calculated with Clopper–Pearson method. All comparisons were two-sided at the 0.05 level of significance (multiplicity was not adjusted). Data were analyzed with R, version 4.0.3 (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient characteristics
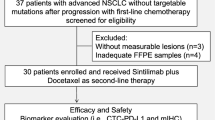
Between October 2019 and October 2020, 40 patients were enrolled and received at least one cycle of the study treatment (Supplementary Fig. 1). The median age was 55 years (range 31–71 years) and 7 (17.5%) were older than 65 years. Of all, 10 (25%) had brain metastases at baseline, and 4 (10%) had EGFR mutations and 6 (15%) had KRAS mutations. Twenty-two (55%) patients received prior chemotherapy, while 18 (45%) patients received prior chemotherapy plus anti-angiogenesis agents (17 patients received chemotherapy plus bevacizumab, including 4 patients with EGFR mutations who failed on first-line EGFR-TKI, and one received chemotherapy plus recombinant human endostatin) (Table 1).
Efficacy
As of the data cutoff date of June 30, 2021, 6 patients were still on study treatment, and the median follow-up time was 12.2 months (range 1.6–20.6 months). A total of 28 patients (70%) had PFS events, with a median PFS of 5.8 months (95% CI 4.1–8.4 months). The PFS rates at 6 and 12 months were 48% and 30%, respectively (Fig. 1a). The median OS (mOS) was 12.6 months (95% CI 5.8–16.1 months), with a 12 months OS rate of 62% (Fig. 1b).
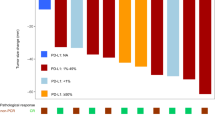
Among 37 (92.5%) patients who received at least one tumor assessment, the ORR was 32.4% (95% CI 18.0–49.8%), including 1 (2.7%) CR and 11 (29.7%) PR, and the DCR was 89.2% (95% CI 74.6–97.0%) (Supplementary Table 1, Fig. 2a). The median DOR was not reached (NR) (95% CI 4.4 months–NR), and the median TTR was 3.9 months (95% CI 1.6–5.0 months). There was a statistically significant improvement in mPFS [NR (95% CI 5.5 months–NR) vs. 4.9 months (95% CI 3.6–8.3 months); P = 0.0017) in patients who achieved CR or PR on the study drugs versus those who achieved SD (Table 2).
The clinical outcomes were further analyzed in subgroups defined by baseline characteristics. Patients with KRAS mutation had a significantly longer mPFS than those with EGFR mutations (16.1 vs. 1.6 months, P = 0.0017). Patients ≥ 65 years of age and with baseline brain metastasis had a mPFS of 6.0 months and 4.9 months, respectively (Table 2). The mPFS was 8.3 months (95% CI 3.6 months–NR) and 5.6 months (95% CI 1.8–8.8) for patients who received prior chemotherapy and prior chemotherapy plus bevacizumab, respectively. For patients who achieved PR, SD, and PD with their prior treatments, the mPFS was 5.2 months (95% CI 2.3 months–NR), 8.4 months (95% CI 4.3 months–NR), and 8.3 months (95% CI 1.6 months–NR), respectively (Table 2). Regarding ORR, there was no significant difference among patients with different baseline characteristics, except for the PD-L1 status (ORR = 66.7% in PD-L1-positive vs. 40% in PD-L1-negative) (Fig. 2b).
Thirteen patients were suspended on treatment or tumor assessment due to the coronavirus disease 2019 pandemic, with a median treatment suspension time of 17 days (range 8–49 days). Among, two patients withdrew from the study, including one who achieved SD at the time of withdrawal, and one died 7 months later. For those 11 patients who continued the treatment, 4 achieved PR and 7 achieved SD.
Safety
As of June 30, 2021, the median treatment duration was 5.9 months (range 0.7–19.1 months). The median treatment cycles was 4 (range 1–6) and 8 (range 1–23) for docetaxel and sintilimab, respectively. Two patients received only one cycle of study regimen, including one received 2 cycles of docetaxel during the study period. Among, two were negative for driver mutation, and one harbored EGFR-sensitive mutations.
Twenty-six patients (65%) experienced treatment-related AEs (TRAEs) and the most common TRAEs were leukopenia (n = 13, 32.5%), neutropenia (n = 7, 17.5%), and alopecia (n = 5, 12.5%). Grade 3 TRAEs occurred in 7 patients (17.5%), including 3 of leucopenia (7.5%), 3 of neutropenia (7.5%) and one of pain (2.5%). Among the patients who experienced grade 3 leucopenia, one (2.5%) developed grade 4 leukopenia after the first cycle, and it was the only grade 4 TRAE during the study period. There were no TRAEs-related permanent treatment discontinuation or death (Table 3). Immune-related AEs occurred in eleven patients (27.5%). Three patients experienced grade 2 pneumonitis, including one who had pneumonia at baseline. The median onset time of pneumonitis was 84 days (range 16–92 days). All three patients were negative for driver mutations and had no history of EGFR-TKI or ALK-TKI treatment. At first-line treatment, one patient received pemetrexed plus carboplatin, one had bevacizumab in combination with pemetrexed plus cisplatin, and one was treated with gemcitabine combined with cisplatin. Pneumonitis resolved after sintilimab suspension and treatments of corticosteroids. Two patients continued treatment with sintilimab after recovery and did not develop recurrent pneumonitis. One achieved a sustained PR till the data cutoff date.
Exploratory biomarker analysis
ctDNA profiling was performed in samples from 32 patients at baseline and after two treatment cycles (at week 6) for 23 patients. In total, 34 cancer-related gene alterations were detected in 27 samples obtained at baseline (Supplementary Fig. 2). Although, the bTMB level at baseline did not significantly differ among the patients with different tumor response (P = 0.898), it was significantly lower in patients with CR + PR compared with patients with SD or PD at week six (P = 0.0427) (Supplementary Fig. 3). Moreover, the change in bTMB level was positively correlated with that of tumor size (Supplementary Fig. 4).
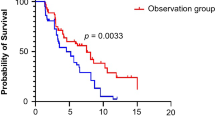
Compared to the patients with ctDNA residual (n = 11, 47.8%), patients with non-ctDNA residual (12, 52.2%) had a significantly longer mPFS (NR vs. 3.0 months, P < 0.0001), an improved ORR (75 vs. 0%, P = 0.0003), and a numerically higher DCR (100 vs. 72.7%, P = 0.09) (Fig. 3).
Discussion
This is the first prospective phase II study that explored the combination of an ICI with chemotherapy in Chinese NSCLC patients who progressed on prior chemotherapies. Sintilimab plus docetaxel conferred favorable survival benefits in terms of mPFS (5.8 months) and mOS (12.6 months), encouraging tumor response (ORR = 32.4%, DCR = 89.2%) and a tolerable safety profile in the study population.
Although ICI monotherapy has become the standard second-line treatment in advanced NSCLC patients who failed first-line chemotherapy, the efficacy of ICI monotherapy remains unsatisfactory. The ORR ranges from 10 to 20% and the PFS is approximately 3 months (Wu et al. 2019; Borghaei et al. 2015, 2021; Rittmeyer et al. 2017). Recently, ICI-containing combination regimens at second-line were developed to enhance its therapeutic effect. In the PROLUNG phase II study (Arrieta et al. 2020), pembrolizumab plus docetaxel has demonstrated a prolonged PFS and improved tumor response in Mexican NSCLC patients compared to docetaxel monotherapy. In China, retrospective studies (Huang et al. 2021; Zhai et al. 2020; Mao et al. 2021) revealed that ICIs combined with chemotherapy or antiangiogenic therapy conferred survival benefits in patients who failed first-line treatment. However, study bias may arise from the small sample size or physician preference for ICIs and chemotherapeutic agents in these studies. In this study, the PFS benefit (5.8 months) appeared superior with sintilimab plus docetaxel when compared with ICI monotherapies, including sintilimab. Despite that, a much longer follow-up time is required to confirm the benefits in OS, our findings supported the second-line strategy of utilizing ICIs in combination with chemotherapy in patients with advanced NSCLC.
Of note, our study has expanded treatment options to broader patient populations in NSCLC. First, our subgroup analysis revealed that the regimen of sintilimab plus docetaxel provided clinical advantages in PFS and tumor remission, regardless of the baseline characteristics, such as baseline brain metastasis, older than 65, and poor response to previous treatment. Second, although bevacizumab plus chemotherapy remains an important first-line treatment option for patients with advanced NSCLC (Socinski et al. 2021), the patients failed on this regimen had limited subsequent treatment options. In our study, a PFS benefit (5.6 months) was observed in patients who progressed on bevacizumab plus chemotherapy, providing a new therapeutic option for this specific population. Finally, mutations in KRAS accounts for approximately 10% of the Chinese NSCLC patients (Liu et al. 2020) and is related to poor prognosis with limited targeted therapy options. Consistent to a meta-analysis (Landre et al. 2021) that has demonstrated the benefits of ICI therapy in NSCLC patients harboring KRAS mutations, a significant benefit in mPFS (16.1 months) was observed in patients with KRAS mutations (n = 6) in this study. It is noteworthy that all six patients had TP53 co-mutation, which together with KRAS, is now considered a potential predictive biomarker for ICI therapy outcomes (Dong et al. 2017). Therefore, our findings suggested that ICIs plus chemotherapy could be a novel option for patients with concurrent KRAS/TP53 mutations.
In previous studies, combination therapy was commonly administered on the same day, and ICIs preceded chemotherapeutic agents. However, several studies have emerged to investigate alternative administration schedules. It is hypothesized that chemotherapy may induce a favorable tumor microenvironment and potentially enhance the response to subsequent PD-1 blockade. In the present study, patients received sintilimab two days after docetaxel. Similarly, the PROLONG study (Arrieta et al. 2020) has evaluated the efficacy of docetaxel on day 1 followed by pembrolizumab on day 8. Additional studies are warranted to study the underlying mechanisms and conduct head-to-head comparisons to optimize the dosing schedule.
In adverse event terms, sintilimab plus docetaxel did not have any unexpected AEs and had a similar irAEs profile to sintilimab or other ICIs. The main grade ≥ 3 AEs were considered related to chemotherapy. There were no grade 5 TRAEs, nor any TRAE-related permanent treatment discontinuation.
Although the OAK study suggested bTMB could be a potential predictive biomarker for PFS in patients treated with atezolizumab, bTMB status in predicting ICI efficacy remains controversial (Gandara et al. 2018). In this study, bTMB reduction at week six was associated with better response and longer PFS, suggesting that the dynamic change in bTMB status, rather than the baseline bTMB status, could be a predictor of the clinical outcomes of ICI-based therapies. Similar to our findings, a phase II study (NCT02644369) evaluating pembrolizumab in advanced solid tumors addressed the importance of monitoring the dynamic changes in bTMB (Bratman et al. 2020).
This study has several limitations worth noting, such as single arm and a small sample size, which may affect the power and significance of the finding. Although our study suggested ICIs plus chemotherapy could be a novel option for patients with concurrent KRAS/TP53 mutations (n = 6) but not for those with EGFR mutations (n = 4), studies with larger cohort size are needed to confirm our findings. Besides, there were no sufficient PD-L1 expression data to determine the association of PD-L1 expression with treatment outcomes. Furthermore, this study did not include the patients who had failed first-line ICIs. Given the increasing applications of immunotherapy in clinical practice, a high medical need exists for the development of salvage therapies for patients who have failed immunotherapy. As reported by a previous phase II study, pembrolizumab combined with docetaxel or pemetrexed showed potential benefits on PFS and OS in patients who failed previous immunotherapy (Shukla et al. 2021). Therefore, further studies are warranted to investigate whether late-line immune combined chemotherapy could provide benefits for this population. Finally, the underlying mechanisms by which dosing orders improve efficacy remain unclear, and dosing schedule need to be optimized.
Conclusion
Sintilimab plus docetaxel has the potential to become a new second-line treatment option for patients with advanced NSCLC, and future studies with larger sample sizes are warranted. More so, the dynamic changes in on-treatment bTMB levels could be considered as a new predictive biomarker in patients treated with ICIs and chemotherapy.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Adizie JB, Khakwani A, Beckett P, Navani N, West D, Woolhouse I, Harden SV (2019) Stage III non-small cell lung cancer management in England. Clin Oncol 31:688–696
Afzal MZ, Dragnev K, Shirai K (2018) A tertiary care cancer center experience with carboplatin and pemetrexed in combination with pembrolizumab in comparison with carboplatin and pemetrexed alone in non-squamous non-small cell lung cancer. J Thorac Dis 10:3575–3584
Arrieta O, Barrón F, Ramírez-Tirado LA, Zatarain-Barrón ZL, Cardona AF, Díaz-García D, Ramos MY, Mota-Vega B, Carmona A, Álvarez MPP (2020) Efficacy and safety of pembrolizumab plus docetaxel vs docetaxel alone in patients with previously treated advanced non-small cell lung cancer: the PROLUNG phase 2 randomized clinical trial. JAMA Oncol 6:856–864
Barbara B, Harrington KJ, Greil R, Soulières D, Tahara M, Castro G Jr, Psyrri A, Basté N, Neupane P, Bratland Å (2019) Pembrolizumab alone or with chemotherapy versus cetuximab with chemotherapy for recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-048): a randomised, open-label, phase 3 study. Lancet 394:1915–28
Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE, Chow LQ, Vokes EE, Felip E, Holgado E (2015) Nivolumab versus docetaxel in advanced nonsquamous non–small-cell lung cancer. N Engl J Med 373:1627–1639
Borghaei H, Gettinger S, Vokes EE, Chow LQM, Burgio MA, de Castro J, Carpeno AP, Arrieta O, Frontera OA, Chiari R (2021) Five-year outcomes from the randomized, phase III trials checkmate 017 and 057: nivolumab versus docetaxel in previously treated non–small-cell lung cancer. J Clin Oncol 39:723–733
Bratman SV, Cindy Yang SY, Iafolla MAJ, Liu Z, Hansen AR, Bedard PL, Lheureux S, Spreafico A, Razak AA, Shchegrova S (2020) Personalized circulating tumor DNA analysis as a predictive biomarker in solid tumor patients treated with pembrolizumab. Nature Cancer 1:873–881
Bruno PM, Liu Y, Park GY, Murai J, Koch CE, Eisen TJ, Pritchard JR, Pommier Y, Lippard SJ, Hemann MT (2017) A subset of platinum-containing chemotherapeutic agents kills cells by inducing ribosome biogenesis stress. Nat Med 23:461–471
Dong Z-Y, Zhong W-Z, Zhang X-C, Jian Su, **e Z, Liu S-Y, Hai-Yan Tu, Chen H-J, Sun Y-L, Zhou Q (2017) Potential predictive value of TP53 and KRAS mutation status for response to PD-1 blockade immunotherapy in lung adenocarcinoma. Clin Cancer Res 23:3012–3024
Ettinger DS, Wood DE, Aisner DL, Akerley W, Bauman JR, Bharat A, Bruno DS, Chang JY, Chirieac LR, D’Amico TA, Dilling TJ, Dowell J, Gettinger S, Gubens MA, Hegde A, Hennon M, Lackner RP, Lanuti M, Leal TA, Lin J, Loo BW Jr, Lovly CM, Martins RG, Massarelli E, Morgensztern D, Ng T, Otterson GA, Patel SP, Riely GJ, Schild SE, Shapiro TA, Singh AP, Stevenson J, Tam A, Yanagawa J, Yang SC, Gregory KM, Hughes M (2021) NCCN guidelines insights: non-small cell lung cancer, version 2.2021. J Natl Compr Canc Netw 19:254–266
Galluzzi L, Humeau J, Buqué A, Zitvogel L, Kroemer G (2020) Immunostimulation with chemotherapy in the era of immune checkpoint inhibitors. Nat Rev Clin Oncol 17:725–741
Gandara DR, Paul SM, Kowanetz M, Schleifman E, Zou W, Li Y, Rittmeyer A, Fehrenbacher L, Otto G, Malboeuf C (2018) Blood-based tumor mutational burden as a predictor of clinical benefit in non-small-cell lung cancer patients treated with atezolizumab. Nat Med 24:1441–1448
Gandhi L, Rodríguez-Abreu D, Gadgeel S, Esteban E, Felip E, De Angelis F, Domine M, Clingan P, Hochmair MJ, Powell SF (2018) Pembrolizumab plus chemotherapy in metastatic non–small-cell lung cancer. N Engl J Med 378:2078–2092
Gao S, Li N, Gao S, Xue Q, Ying J, Wang S, Tao X, Zhao J, Mao Y, Wang B, Shao K, Lei W, Wang D, Lv F, Zhao L, Zhang F, Zhao Z, Su K, Tan F, Gao Y, Sun N, Wu D, Yu Y, Ling Y, Wang Z, Duan C, Tang W, Zhang L, He S, Wu N, Wang J, He J (2020) Neoadjuvant PD-1 inhibitor (sintilimab) in NSCLC. J Thorac Oncol 15:816–826
Huang Di, Cui P, Huang Z, Zhaozhen Wu, Tao H, Zhang S, **ang R, Yi Hu (2021) Anti-PD-1/L1 plus anti-angiogenesis therapy as second-line or later treatment in advanced lung adenocarcinoma. J Cancer Res Clin Oncol 147:881–891
Iida Y, Harashima N, Motoshima T, Komohara Y, Eto M, Harada M (2017) Contrasting effects of cyclophosphamide on anti-CTL-associated protein 4 blockade therapy in two mouse tumor models. Cancer Sci 108:1974–1984
Janjigian YY, Shitara K, Moehler M, Garrido M, Salman P, Shen L, Wyrwicz L, Yamaguchi K, Skoczylas T, Bragagnoli AC (2021) First-line nivolumab plus chemotherapy versus chemotherapy alone for advanced gastric, gastro-oesophageal junction, and oesophageal adenocarcinoma (CheckMate 649): a randomised, open-label, phase 3 trial. Lancet. https://doi.org/10.1016/S0140-6736(21)00797-2
Landre T, Justeau G, Assié J-B, Chouahnia K, Taleb C, Chouaid C, Duchemann B (2021) Anti PD-(L) 1 in KRAS mutant advanced nsclcs: a meta-analysis of randomized controlled trials. Wolters Kluwer Health
Li N, Wang Z, Xu N, Ying K, Liu Y, Lu S, Yang J (2018) Evaluation of efficacy and safety of Sindilizumab in patients with advanced non-small cell lung cancer in China (in Chinese). In: Abstracts of the 21st Annual Meeting of Chinese Society of Clinical Oncology (CSCO), **amen, China, p 15
Liu S-Y, Sun H, Zhou J-Y, Jie G-L, **e Z, Shao Y, Zhang X, Ye J-Y, Chen C-X, Zhang X-C (2020) Clinical characteristics and prognostic value of the KRAS G12C mutation in Chinese non-small cell lung cancer patients. Biomark Res 8:1–7
Mao S, Zhou F, Liu Y, Yang S, Chen B, Xu J, Wu F, Li X, Zhao C, Wang W (2021) ICI plus chemotherapy prolonged survival over ICI alone in patients with previously treated advanced NSCLC. Cancer Immunol Immunother 71(1):219–28
Paz-Ares L, Vicente D, Tafreshi A, Robinson A, Parra HS, Mazières J, Hermes B, Cicin I, Medgyasszay B, Rodríguez-Cid J (2020) A randomized, placebo-controlled trial of pembrolizumab plus chemotherapy in patients with metastatic squamous NSCLC: protocol-specified final analysis of KEYNOTE-407. J Thorac Oncol 15:1657–1669
Reck M, Rodríguez-Abreu D, Robinson AG, Hui R, Csőszi T, Fülöp A, Gottfried M, Peled N, Tafreshi A, Cuffe S (2016) Pembrolizumab versus chemotherapy for PD-L1–positive non–small-cell lung cancer. N Engl J Med 375:1823–1833
Rittmeyer A, Barlesi F, Waterkamp D, Park K, Ciardiello F, Von Pawel J, Gadgeel SM, Hida T, Kowalski DM, Dols MC (2017) Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet 389:255–265
Shi Y, Hang Su, Song Y, Jiang W, Sun X, Qian W, Zhang W, Gao Y, ** Z, Zhou J (2019) Safety and activity of sintilimab in patients with relapsed or refractory classical Hodgkin lymphoma (ORIENT-1): a multicentre, single-arm, phase 2 trial. Lancet Haematol 6:e12–e19
Shukla N, Althouse SK, Perkins S, Furqan M, Leal T, Hanna NH, Durm GA (2021) A phase II trial of chemotherapy plus pembrolizumab in patients with advanced NSCLC previously treated with a PD-1 or PD-L1 inhibitor: big ten cancer research consortium BTCRC-LUN15–029. Wolters Kluwer Health
Siegel RL, Miller KD, Fuchs HE, Jemal A (2021) Cancer statistics, 2021. CA Cancer J Clin 71:7–33
Socinski MA, Nishio M, Jotte RM, Cappuzzo F, Orlandi F, Stroyakovskiy D, Nogami N, Rodríguez-Abreu D, Moro-Sibilot D, Thomas CA (2021) IMpower150 final overall survival analyses for atezolizumab plus bevacizumab and chemotherapy in first-line metastatic nonsquamous NSCLC. J Thorac Oncol. https://doi.org/10.1016/j.jtho.2021.07.009
Suzuki E, Kapoor V, Jassar AS, Kaiser LR, Albelda SM (2005) Gemcitabine selectively eliminates splenic Gr-1+/CD11b+ myeloid suppressor cells in tumor-bearing animals and enhances antitumor immune activity. Clin Cancer Res 11:6713–6721
Voorwerk L, Slagter M, Horlings HM, Sikorska K, van de Vijver KK, de Maaker M, Nederlof I, Kluin RJC, Warren S, Ong SuFey (2019) Immune induction strategies in metastatic triple-negative breast cancer to enhance the sensitivity to PD-1 blockade: the TONIC trial. Nat Med 25:920–928
Wanderley CW, Colon DF, João PM, Luiz FF, Oliveira PR, Viacava CA, Leite JA, Pereira CM, Silva CR, Silva, and Rangel L. Silva. (2018) Paclitaxel reduces tumor growth by reprogramming tumor-associated macrophages to an M1 profile in a TLR4-dependent manner. Can Res 78:5891–5900
Welters MJ, van der Sluis TC, van Meir H, Loof NM, van Ham VJ, van Duikeren S, Santegoets SJ, Arens R, de Kam ML, Cohen AF (2016) Vaccination during myeloid cell depletion by cancer chemotherapy fosters robust T cell responses. Sci Transl Med 8:33452–3452
Wu Y-L, Shun Lu, Cheng Y, Zhou C, Wang J, Mok T, Zhang Li, Hai-Yan Tu, Lin Wu, Feng J (2019) Nivolumab versus docetaxel in a predominantly Chinese patient population with previously treated advanced NSCLC: CheckMate 078 randomized phase III clinical trial. J Thorac Oncol 14:867–875
Zhai X, **g X, Li J, Tian Y, Xu S, Wang M, Zhu H (2020) Clinical outcomes for PD-1 inhibitor plus chemotherapy as second-line or later therapy compared to PD-1/PD-L1 inhibitor alone in advanced non-small-cell lung cancer. Front Oncol. https://doi.org/10.3389/fonc.2020.556275
Acknowledgements
We thank the patients, their families, and all caregivers.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
HX contributed to conceptualization and methodology; ZW contributed to supervision; GJ contributed to data curation and visualization; XT, HZ, DZ, XZ, XM, YH, ZW, YZ, WH, LW, SY, PZ, HG, YS, YZ and ZL contributed to investigation; HX, GJ and ZW contributed to writing the manuscript and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
All the procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by was approved by the Ethics Board of Shandong Provincial Institute of Cancer Prevention and Treatment.
Consent to participate
Not applicable.
Consent for publish
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
432_2022_4023_MOESM2_ESM.tif
Supplementary file2 (TIF 36 KB) Mutation landscape of baseline ctDNA profiling (N=27). A total of 34 cancer-related gene alterations (occurred in ≥2 samples) detected from 27 samples were depicted
432_2022_4023_MOESM3_ESM.tif
Supplementary file3 (TIF 390 KB) The correlation between bTMB level and best overall response (BOR). a baseline bTMB level; b bTMB level at the end of the 6th week
432_2022_4023_MOESM4_ESM.tif
Supplementary file4 (TIF 184 KB) Correlation between change of bTMB level and change of tumor size. a Correlation between percentage changes in bTMB and the percentage change in SLD (sum of the longest diameters); The percentage changes between bTMB and SLD of target lesions at the end of the 6th week were positively correlated (R2 =0.4564; P = 0.0004), as well as the percentage changes of SLD at BOR (R2 =0.3977; P = 0.0013); b correlation between absolute changes in bTMB and change in SLD. Statistically significant correlation was found between absolute changes of bTMB and SLD of target lesions at 6th week (R2 =0.1732; P = 0.0482), as well as at BOR (R2 =0.1752; P = 0.0468)
Rights and permissions
About this article
Cite this article
Han, X., Guo, J., Tang, X. et al. Efficacy and safety of sintilimab plus docetaxel in patients with previously treated advanced non-small cell lung cancer: a prospective, single-arm, phase II study in China. J Cancer Res Clin Oncol 149, 1443–1451 (2023). https://doi.org/10.1007/s00432-022-04023-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-022-04023-z