Abstract
Background
No international consensus has been reached regarding delineation of postoperative intensity-modulated radiotherapy (PO-IMRT) clinical target volumes (CTV) for major salivary gland carcinoma (SGC). The purpose of this article was to report our experience according to surgical principles.
Methods
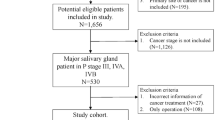
Between June 2010 and June 2018, 54 consecutive patients were enrolled. Reserved tissues around the margin of resection that were less than 5 mm from the invasive tumour edge before surgery were defined as high-risk clinical target volumes (CTV-HD), those less than 10 mm away were defined as medium-risk CTV (CTV1), and those 10–20 mm away were defined as low-risk CTV (CTV2), and were irradiated with 63–65 Gy, 59.5–61 Gy, and 45–54 Gy, respectively. Target volume distributions of reserved tissues were analysed and actuarial estimates of overall survival (OS), recurrence-free survival (RFS) and distant metastasis-free survival (DMFS) were obtained with the Kaplan–Meier method.
Results
In parotid gland tumours, the percentages of defined CTV-HD in the styloid process, mandibular ramus, posterior venter of the digastric muscle, carotid sheath and stylomastoid foramen reached 34.29%, 25.71%, 54.29%, 40.00%, and 37.10%, respectively. The median follow-up was 33 months (range, 5–98 months). The 3-year and 5-year Kaplan–Meier estimates of OS, RFS and DMFS were 85.4% and 77.8%, 97.4%, and 97.4%, and 82.0% and 82.0%, respectively.
Conclusions
It is feasible to delineate CTVs according to distances between various reserved tissues and the primary tumour edge before operation.



Similar content being viewed by others
References
Allisy B, Kellerer AM: International Commission on Radiation Units and Measurements (1993) Report 50. Prescribing, recording and reporting photon beam therapy. ICRU
Al-Mamgani A, van Rooij P, Verduijn GM, Meeuwis CA, Levendag PC (2012) Long-term outcomes and quality of life of 186 patients with primary parotid carcinoma treated with surgery and radiotherapy at the Daniel den Hoed Cancer Center. Int J Radiat Oncol Biol Phys 84(1):189–195
Byers RM, Bland KI, Borlase B, Luna M (1978) The prognostic and therapeutic value of frozen section determinations in the surgical treatment of squamous carcinoma of the head and neck. Am J Surg 136(4):525–528
Campbell S, Poon I, Markel D, Vena D, Higgins K, Enepekides D et al (2012) Evaluation of microscopic disease in oral tongue cancer using whole-mount histopathologic techniques: implications for the management of head-and-neck cancers. Int J Radiat Oncol Biol Phys 82(2):574–581
Cheng W (2015) Clinical target volume delineation of intensity-modulated radiotherapy for head and neck squamous cell carcinoma. In: The 12th national congress of radiation oncology and CSTRO-SANTRO seminar on MRI application in radiation oncology, Chengdu, China
David G, Pfister SS, Adelstein D, Adkins D, Brizel DM, Burtness B et al (2018) NCCN guidelines version 1.2018 panel members head and neck cancers. NCCN Clin Practice Oncol 6(1):17–84
Evans M, Beasley M (2018) Target delineation for postoperative treatment of head and neck cancer. Oral Oncol 86:288–295
Fleury B, Thariat J, Barnoud R, Buiret G, Lebreton F, Bancel B et al (2014) Approche anatomopathologique de l’extension microscopique des carcinomes épidermoïdes ORL : implications pour la définition du volume cible anatomoclinique. Cancer/Radiothérapie 18(7):666–671
Gomez DR, Katabi N, Zhung J, Wolden SL, Zelefsky MJ, Kraus DH et al (2009) Clinical and pathologic prognostic features in acinic cell carcinoma of the parotid gland. Cancer 115(10):2128–2137
Gregoire V, Evans M, Le QT, Bourhis J, Budach V, Chen A et al (2018) Delineation of the primary tumour Clinical Target Volumes (CTV-P) in laryngeal, hypopharyngeal, oropharyngeal and oral cavity squamous cell carcinoma: AIRO, CACA, DAHANCA, EORTC, GEORCC, GORTEC, HKNPCSG, HNCIG, IAG-KHT, LPRHHT, NCIC CTG, NCRI, NRG Oncology, PHNS, SBRT, SOMERA, SRO, SSHNO. TROG Cons Guide Rad Oncol 126(1):3–24
Hansen CR, Johansen J, Samsoe E, Andersen E, Petersen JBB, Jensen K et al (2018) Consequences of introducing geometric GTV to CTV margin expansion in DAHANCA contouring guidelines for head and neck radiotherapy. Radiother Oncol 126(1):43–47
Hosni A, Huang SH, Goldstein D, Xu W, Chan B, Hansen A et al (2016) Outcomes and prognostic factors for major salivary gland carcinoma following postoperative radiotherapy. Oral Oncol 54:75–80
Ju J, Li Y, Chai J, Ma C, Ni Q, Shen Z et al (2016) The role of perineural invasion on head and neck adenoid cystic carcinoma prognosis: a systematic review and meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol 122(6):691–701
Kaur J, Goyal S, Muzumder S, Bhasker S, Mohanti BK, Rath GK (2014) Outcome of surgery and post-operative radiotherapy for major salivary gland carcinoma: ten year experience from a single institute. Asian Pac J Cancer Prev 15(19):8259–8263
Langendijk JA, Slotman BJ, van der Waal I, Doornaert P, Berkof J, Leemans CR (2005) Risk-group definition by recursive partitioning analysis of patients with squamous cell head and neck carcinoma treated with surgery and postoperative radiotherapy. Cancer 104(7):1408–1417
Lee N, **a P, Fischbein NJ, Akazawa P, Akazawa C, Quivey JM (2003) Intensity-modulated radiation therapy for head-and-neck cancer: the UCSF experience focusing on target volume delineation. Int J Radiat Oncol Biol Phys 57(1):49–60
McMahon J, Hamill IPR, McNeil E, Hammersley N, Gardiner S et al (2003) Influence of condition of surgical margins on local recurrence and disease-specific survival in oral and oropharyngeal cancer. Br J Oral Maxillofac Surg 41(4):224–231
Merlotti A, Alterio D, Vigna-Taglianti R, Muraglia A, Lastrucci L, Manzo R et al (2014) Technical guidelines for head and neck cancer IMRT on behalf of the Italian association of radiation oncology - head and neck working group. Radiat Oncol 9(1):9
Morse E, Fujiwara RJT, Judson B, Prasad ML, Mehra S (2019) Positive surgical margins in parotid malignancies: Institutional variation and survival association. Laryngoscope 129(1):129–137
North CA, Lee D-J, Piantadosi S, Zahurak M, Johns ME (1990) Carcinoma of the major salivary glands treated by surgery or surgery plus postoperative radiotherapy. Int J Radiat Oncol Biol Phys 18(6):1319–1326
Nutting CM, Morden JP, Beasley M, Bhide S, Cook A, De Winton E et al (2018) Results of a multicentre randomised controlled trial of cochlear-sparing intensity-modulated radiotherapy versus conventional radiotherapy in patients with parotid cancer (COSTAR; CRUK/08/004). Eur J Cancer 103:249–258
Ord RA, Ghazali N (2017) Margin analysis: malignant salivary gland neoplasms of the head and neck. Oral Maxillofac Surg Clin North Am 29(3):315–324
Pohar S, Gay H, Rosenbaum P, Klish D, Bogart J, Sagerman R et al (2005) Malignant parotid tumors: presentation, clinical/pathologic prognostic factors, and treatment outcomes. Int J Radiat Oncol Biol Phys 61(1):112–118
Servagi-Vernat S, Tochet F (2016) Radiothérapie des tumeurs des glandes salivaires. Cancer/Radiothérapie 20:S136–S138
Rita A, Kian Ang M, Eric S, David R, Randal W, Phuc Felix N (2009) A Randomized, Phase III, Double-Blind, Placebo-controlled study to evaluate the efficacy and safety of palifermin (NSC# 740548) for the reduction of oral mucositis in patients with locally advanced head and neck cancer receiving radiation therapy with concurrent radiotherapy (followed by surgery for selected patients). https://www.nrgoncology.org/Clinical-Trials/Protocol/rtog-0522?filter=rtog-0522
Terhaard CHJ, Lubsen H, Rasch CRN, Levendag PC, Kaanders HHÀM, Tjho-Heslinga RE et al (2005) The role of radiotherapy in the treatment of malignant salivary gland tumors. Int J Radiat Oncol Biol Phys 61(1):103–111
Wang L, Wu Z, **e D, Zeng R, Cheng W, Hu J et al (2019) Reduction of target volume and the corresponding dose for the tumor regression field after induction chemotherapy in locoregionally advanced nasopharyngeal carcinoma. Cancer Res Treat 51(2):685–695
**ao WW, Huang SM, Han F, Wu SX, Lu LX, Lin CG et al (2011) Local control, survival, and late toxicities of locally advanced nasopharyngeal carcinoma treated by simultaneous modulated accelerated radiotherapy combined with cisplatin concurrent chemotherapy: long-term results of a phase 2 study. Cancer 117(9):1874–1883
**e D, Cheng W, Lv S, Zhong R, Wang L, Hu J et al (2019) Target delineation and dose prescription of adaptive replanning intensity-modulated radiotherapy for nasopharyngeal carcinoma. Cancer Commun (Lond) 39(1):18
Yuen PW, Lam KY, Chan AC, Wei WI, Lam LK (1998) Clinicopathological analysis of local spread of carcinoma of the tongue. Am J Surg 175(3):242–244
Acknowledgements
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lyu, S., Wu, Z., **e, D. et al. Clinical target volume design of postoperative intensity-modulated radiotherapy for major salivary gland tumours according to surgical principles: an innovative method. J Cancer Res Clin Oncol 148, 921–930 (2022). https://doi.org/10.1007/s00432-021-03646-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-021-03646-y