Abstract
Intraventricular haemorrhage (IVH) and bronchopulmonary dysplasia (BPD) are major complications of premature birth. We tested the hypotheses that prematurely born infants who developed an IVH or BPD would have high expiratory tidal volumes (VTE) (VTE > 6 ml/kg) and/or low-end tidal carbon dioxide (ETCO2) levels (ETCO2 levels < 4.5 kPa) as recorded by respiratory function monitoring or hyperoxia (oxygen saturation (SaO2) > 95%) during resuscitation in the delivery suite. Seventy infants, median gestational age 27 weeks (range 23–33), were assessed; 31 developed an IVH and 43 developed BPD. Analysis was undertaken of 31,548 inflations. The duration of resuscitation did not differ significantly between the groups. Those who developed an IVH compared to those who did not had a greater number of inflations with a high VTE and a low ETCO2, which remained significant after correcting for differences in gestational age and birth weight between groups (p = 0.019). Differences between infants who did and did not develop BPD were not significant after correcting for differences in gestational age and birth weight. There were no significant differences in the duration of hyperoxia between the groups.
Conclusions: Avoidance of high tidal volumes and hypocarbia in the delivery suite might reduce IVH development.
What is known • Hypocarbia on the neonatal unit is associated with the development of intraventricular haemorrhage (IVH) and bronchopulmonary dysplasia (BPD). | |
What is new • Infants who developed an IVH compared to those who did not had significantly more inflations with high expiratory tidal volumes and low ETCO2s. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intraventricular haemorrhage (IVH) and bronchopulmonary dysplasia (BPD) are major complications of premature birth. Studies from infants receiving neonatal intensive care have demonstrated that hypocarbia is associated with the development of IVH [8] and BPD [9]. In a study of 314 infants born at less than 29 weeks of gestation, hypocarbia increased the risk of severe IVH and BPD, particularly the latter when the hypocarbia was prolonged [9]. In a three-centre study of VLBW infants all born less than 34 weeks of gestation, risk factors for IVH were determined. Four factors were independently associated with IVH: gestational age, use of nitric oxide, a base deficit greater than ten and hypocarbia [2]. Both extremes of arterial carbon dioxide pressure were associated with severe IVH in preterm infants [8]. A secondary exploratory data analysis of data from the SUPPORT study (surfactant, positive pressure and oxygenation randomised trial) which included 1316 infants born between 24 and 28 weeks of gestation demonstrated severe IVH and BPD were both associated with hypercapnia and fluctuations in PaCO2 (both hypercarbia and AGRhypocarbia) [1].
Hypocarbia can result from excessive mechanical ventilation. High tidal volumes immediately after delivery, particularly before the administration of surfactant, have been demonstrated in animal models to result in inflammatory changes within the lung and chronic lung damage [4, 6]. Respiratory function monitoring has demonstrated that the tidal volumes delivered can vary widely even during the initial resuscitation of prematurely born infants [17]. It is likely that infants who receive high tidal volumes during resuscitation would suffer from hypocarbia, as indicated by low end-tidal carbon dioxide (ETCO2) levels. Whether high tidal volumes and low ETCO2 levels in the delivery suite are associated with the development of BPD and IVH have rarely been assessed. Tracey et al. reported that 26% of surfactant-treated preterm infants born less than 34 weeks of gestation were hypocarbic on NICU admission, and 20% were both hypocarbic and hyperoxic likely reflecting events in the delivery suite [25], but they did not report whether this influenced their outcome. Kong et al. reported median cord PCO2 values of 50 mmHg and a wide range of PCO2 values after NICU admission [13], but again did not relate this to outcomes such as IVH and BPD. In a prospective study of 170 infants all less than 33 weeks of gestation, arterial or venous blood gases were obtained within the first hour after birth. Hypocarbia and hyperoxia were uncommon, but hypercarbia (57%) occurred frequently. Multivariate logistic regression analysis, however, showed no significant association with a low or high PaCO2 or high PaO2 with death or major inpatient morbidities including IVH and BPD [11]. A recent study of infants less than 29 weeks of gestational age [15] showed an association between high tidal volumes (> 6 mls/kg) at resuscitation and the development of IVH.
We hypothesised that infants who developed an IVH or BPD would have high tidal volumes and/or low ETCO2 levels as documented by respiratory function monitoring during resuscitation in the labour suite. In addition, those who developed an IVH or BPD would be more likely to have been hyperoxic as indicated by an oxygen saturation (SaO2) greater than 95%. An aim of this study was to test those hypotheses. A second aim was to determine whether infants who developed a severe IVH would have higher tidal volumes or lower ETCO2 levels than those who developed a non-severe IVH.
Patients and methods
Respiratory recordings of infants born at 33 weeks or less gestational age requiring resuscitation in the delivery suite between March 2010 and March 2014 were retrospectively reviewed. Ethical approval was given by the Outer London Ethics Committee. The committee required parental consent only for the analysis of the data. This was obtained once the mother was transferred to the postnatal ward. This study was approved by the King’s College Hospital NHS Foundation Trust Research and Audit Department.
Resuscitation protocol
The clinicians attending the resuscitations had all been trained in newborn life support and had received the Resuscitation Council, UK NLS (Newborn Life Support) provider certificate and followed the Council’s recommendations on whether to commence face mask resuscitation [23]. They had also been trained to operate the respiratory function monitor. During the resuscitation, the respiratory function monitor was set to display tidal volume, flow, inflation pressures and ETCO2 levels. The research team was available for help and advice in operating the recording equipment.
Positive pressure ventilation was delivered via a t-piece device (Neopuff Infant resuscitator, Fisher & Paykel Healthcare, Auckland, New Zealand). The pressure relief valve was to be set at 30 cm H2O. The local policy, which followed national and international guidelines was to start with a peak inflation pressure of 20 cm H2O maintained for 2 to 3 s for five breaths before reassessing the condition of the infant. Subsequently, ventilator breaths (inflation breaths) of up to 1 s are used. If there is an inadequate response, further inflation breaths are given. The inflation pressure was to be increased if the chest wall rise was considered inadequate. The continuous flow, pressure-limiting device had a built-in manometer and a positive end expiratory pressure (PEEP) valve. A PEEP of 4–5 cm H2O and a flow of 5 l/min were used during all resuscitations. The t-piece was attached to a round face mask (Marshall Infant, Bath, UK). A size 0 or 1 mask was selected by the clinician according to which mask size they felt would be most likely to achieve an adequate seal. Oxygen saturation monitoring was routinely used during the resuscitation of prematurely born infants; the probe was attached to the right hand. The local policy was that resuscitation was commenced using an inspired oxygen fraction (FiO2) of 0.21, which was to be increased to maintain an oxygen saturation of between 85 and 92%.
Respiratory function monitoring was undertaken as part of a research study and levels of VT and ETCO2 were not prescribed. During the study, there were no changes in the resuscitation guidelines that were used.
Monitoring equipment
A NM3 respiratory profile monitor (RPM) (Philips, Respironics), connected to a Laptop (Dell latitude) with customised software (3.0.1.4) (Grove medical, London, UK), was used to obtain respiratory waveform and record mainstream end tidal CO2. The NM3 respiratory profile monitor has a combined pressure, flow and carbon dioxide (CO2) sensor which was inserted between the T-piece and the face mask or endotracheal tube. The flow and pressure measurements were made using a fixed orifice differential pressure pneumotachograph. The NM3 monitor was automatically calibrated for flow, pressure and CO2 according to the factory-stored calibration inside the monitor. The pressure transducer was automatically “zeroed” to correct for changes in ambient temperature. According to the manufacturer’s information, the accuracy of the flow sensor was ± 3% and the airway pressure was ± 2%. These have been previously confirmed by in vitro studies in our laboratory [17]. The monitoring was commenced at the onset of positive pressure inflations; the time after delivery when positive pressure inflations were commenced was not recorded.
Only after the respiratory recordings were analysed (see below) were the medical records examined to determine whether the infants had developed an IVH or BPD. An IVH was diagnosed from cranial ultrasounds routinely performed. As per unit policy, cranial ultrasounds were performed on admission to unit for all infants born below 34 weeks of gestation or any infant ventilated. Cranial ultrasounds were performed as soon as possible after admission when the baby was stabilised. Subsequent ultrasound scans were performed on day three, between days 7 and 10, days 14 and 21 and days 28 and 30. All cranial ultrasounds were performed by a neonatal registrar or consultant and subsequently reviewed and reported by a neonatal consultant who was unaware of the results of the resuscitation recordings. The IVHs were reported as grades I to IV using the Papile classification [20], (grade III–IV severe and grade I to II non-severe). BPD was diagnosed if the infant required supplemental oxygen beyond 28 days [12] to maintain their oxygen saturation levels above 92%. An oxygen reduction test at 36 weeks postmenstrual age was not undertaken; hence, we did not report BPD as defined as oxygen dependency at 36 weeks PMA. Infants who died before 28 days were excluded from the BPD analysis. Other data extracted from the notes included the infant’s gestational age, birth weight and Apgar score at 5 min and whether the mother had received corticosteroids antenatally, had had chorioamnionitis or an antepartum haemorrhage.
Analysis
The recordings were analysed to determine the duration of resuscitation, the number of inflations, the inflation pressure, PEEP, inflation time (Ti), mean airway pressure (MAP) and expiratory tidal volume (VTE) of each inflation and the breath by breath minute ventilation. No initial inflation breaths (i.e. 2–3 s duration) were analysed. All inflations (ventilator breaths) were included when the infant was receiving positive pressure inflations but not CPAP. The number of inflations with tidal volumes more than 6 mls/kg (high tidal volumes) or end tidal CO2 levels of less than 4.5 kPa (low ETCO2 levels) were determined, as were the number of inflations with both high tidal volumes and low ETCO2 levels. These cut-offs were decided a priori. The VTE of 6 ml/kg was selected as this was found to be the optimal tidal volume during volume-targeted ventilation in a number of conditions, that is associated with the lowest work of breathing [5, 21, 22]. The ETCO2 of 4.5 kPa was selected as this was the lower end of the normal range of PaCO2 values used in our unit. The lowest ETCO2 and highest ETCO2 level for each recording were identified. Recordings were not analysed if throughout resuscitation the leak was greater than 30%. On other recordings, inflations with a leak greater than 30% were not analysed. The degree of leak was determined by comparing the inspiratory and expiratory volumes, e.g. the inspiratory volume was 30% greater than the expiratory volume. We did correct for leak flow at PEEP.
Statistical analysis
The data were tested for normality and found not to be normally distributed. Differences, therefore, were assessed for statistical significance using the Mann-Whitney U test or the chi-square test as appropriate. Regression analyses were performed to determine if results remained statistically significant after correcting for differences in gestational age and birth weight between the groups. Statistical analysis was performed by using SPSS Statistics Desktop, V23.0.0.
Results
During the study period, 370 infants were born less than 33 weeks of gestation. There were 150 recordings available for analysis, but 56 were excluded because of artefacts in the tidal volume or ETCO2 traces and 24 were excluded due to a large leak throughout. A total of 31,548 inflations were assessed from the recordings from the remaining 70 infants.
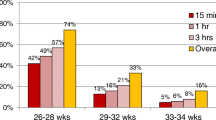
Thirty-one infants developed an IVH, and all IVHs occurred on or before day 3. Those who developed an IVH were more immature (p < 0.01) and of lower birth weight (p = 0.015) than those who did not develop an IVH, but there were no other significant differences in their demographics (Table 1). The IVH group compared to the no IVH group also had the highest ETCO2 levels (p < 0.005) and highest inflation rate (p < 0.005) after adjustment for gestational age and birth weight (Table 2). The IVH group received a greater number of inflations with a VT > 6 mls/kg (p = 0.002) and inflations with an ETCO2 < 4.5 kPa (p = 0.016) and inflations with both a VT > 6mls/kg and an ETCO2 < 4.5 kPa (p = 0.019) (Fig. 1); they also had the highest ETCO2 level (p < 0.005). The percentage number of inflations with a high tidal volume in the IVH and no IVH group was 22 versus 6.5% respectively, with a low ETCO2 in the IVH and no IVH group of 15 versus 0.26% respectively and the percentage of inflations with a high tidal volume and a low ETCO2 in the IVH and no IVH group was 3.6 versus 0% respectively. ETCO2 values as low as 1.8 and 1.5 kPa were recorded in the IVH and no IVH groups respectively (Tables 2 and 3). There was no significant difference in the time spent with a SaO2 > 95% between the IVH and non IVH group (p = 0.989). Thirteen of the 31 infants developed a severe IVH. Infants who developed a severe IVH rather than a non-severe IVH had a lower “lowest” ETCO2 (p = 0.038) (Table 3).
Forty-three infants developed BPD; they were more immature (p < 0.005) and of lower birth weight (p < 0.005) than those who did not develop BPD (Table 1). Infants who developed BPD compared to those who did not develop BPD received a higher number of inflations with an ETCO2 level < 4.5 mmHg (p = 0.003) and a higher number of inflations with both a VT > 6mls/kg and a ETCO2 level < 4.5 Kpa (p = 0.013), and the BPD group also had the lowest ETCO2 level (p = 0.007) (Table 4). None of these differences, however, remained significant after controlling for gestational age and birth weight (Table 4). There were no significant differences in the maximum saturation level (p = 0.14) between the two groups. There was a trend for infants who developed BPD to have a shorter time spent with oxygen saturations greater than 95% (p = 0.048), but this was no longer significant once corrected for gestational age and birth weight (p = 0.101).
Discussion
We have demonstrated that infants who developed an IVH received more inflations during the resuscitation in the labour suite resulting in a high tidal volume (> 6 mls/kg) or a low ETCO2 (< 4.5 Kpa). A greater number of inflations with a high tidal volume and/or a low ETCO2 in the IVH group would mean that those infants had been exposed to a longer time with such inflations. Those results remained significant after adjusting for gestational age and birth weight. In addition, infants who developed a severe IVH compared to a non-severe IVH had the lowest ETCO2 levels. The IVH group had significantly more inflations with a tidal volume greater than 6 mls/kg and ETCO2 levels less than 4.5 kPa suggesting that the high tidal volumes had resulted in a low ETCO2. We [18] and others [11, 25] have reported that there may be no ETCO2 immediately after birth, likely reflecting that pulmonary vasodilation had not occurred. Hence, we have reported analysis of positive pressure inflations during the duration of resuscitation, we did not analyse initial resuscitation when in the UK 2 to 3-s inflations are used. We found no significant differences in the Apgar scores at 5 min between those who did and did not develop an IVH suggesting that the IVH group was not sicker at initial resuscitation. In addition, there were no significant differences in the number of inflations analysed between the groups nor the duration of resuscitation. Furthermore, there were no significant differences in antenatal events such as corticosteroid exposure, chorioamnionitis or antepartum haemorrhage which could have affected their outcomes. Thus, our findings may suggest an association of the impact of resuscitation on outcomes. A recent study demonstrated infants born before 29 weeks of gestation were more likely to develop an IVH if they were resuscitated with tidal volumes greater than 6 ml/kg, but no data on ETCO2 levels were given [15]. In a prospective observational cohort study of infants born at less than 33 weeks of gestational age, hyperoxia, hypocarbia and hypercarbia did not significantly correlate with adverse inpatient outcomes or death [24]. Hyperoxia and hypercarbia, however, occurred infrequently, and the blood gas analysis was undertaken in the first hour after birth [24] and was not assessed in the delivery suite as in our study.
Hypocarbia in infants ventilated on the neonatal unit has been reported to be associated with adverse outcomes. A review of clinical and blood gas data collected in the first four postnatal days from 849 infants with birth weights of 401 to 1250 g highlighted that those who developed an IVH had higher maximal and lower minimal PaCO2 levels [8]. A retrospective, cohort analysis of 314 infants of less than 29 weeks of gestational age demonstrated that those whose PaCO2 fell below 30 mmHg at any stage in the first 48 h had an increased risk of IVH, and those that had three such recordings in the first 24 h had an increased risk of BPD [7]. Kraybill reported that factors associated with BPD included the lowest PaCO2 at 48 h [14], and Garland reported that a PaCO2 of less than 29 mmHg prior to exogenous surfactant was associated with an increased risk of BPD [9]. All those results, however, were before the routine use of antenatal steroids and postnatal surfactant and none commented on the contribution of low PaCO2 levels in the labour suite. In contrast, arterial venous or arterial blood gas analysis performed within the first hour after birth in 75 infants, mean gestational age of 28 weeks with arterial blood gases demonstrated none had hypocarbia (< 30 mmHg) and 51% were hypercarbic (> 55 mmHg), 11% were hyperoxic (> 80 mmHg) and 22% had hypoxia (< 50 mmHg). Multivariable logistic regression analysis demonstrated no significant association of low or high PCO2 or PO2 with death or major inpatient morbidities [11]. In a more recent study, 59 preterm infants born less than 32 weeks of gestation were randomly assigned to the use of a disposable PediCapET CO2 detector or a Microstream side stream capnography device during face mask ventilation in the delivery suite. Normocarbia was defined as PaCO2 measure between 37.5 and 60 mmHg in the first hour after birth. No significant differences were found in incidence of the normocarbia and outcomes such as IVH or BPD [10].
We found no significant difference in the time with a SaO2 > 95%, i.e. hyperoxia between those who did and did not develop BPD. This is perhaps surprising as many studies have reported the injurious effects of perinatal supplemental oxygen on lung development [3]. Many of those studies, however, have reported the effect of prolonged exposure to hyperoxia [26, 28]. In our study, the maximum duration of resuscitation was only 16 min. It has also been shown that there is a dose-dependent effect on the severity of BPD [27]. In this study, we report infants initially resuscitation in a FiO2 of 0.21.
This study has strengths and some weaknesses. A large number of inflations were analysed independent of knowledge of the infants’ outcomes. We analysed the outcome of inflations as if we found an adverse association; this could lead to improvements in clinical practice, which is by reduction in the magnitude of delivered inflations. Although the data were analysed retrospectively, the respiratory function monitoring was carried out as part of a prospective study. The respiratory function monitoring was undertaken as a research study, and the wide range of tidal volumes and ETCO2 levels suggest that the clinical team were not routinely using the displayed information to guide the level of support. Indeed, we have previously shown that many paediatric trainees were unaware of the size of a “normal” tidal volume [16]. It is not clear whether routine respiratory function monitoring in the labour suite would improve outcomes [19]. No significant differences in the incidence of IVH were found in a randomised trial comparing use of a respiratory function monitor with the display which was visible or masked [20]. The trial, however, included 49 infants and the targeted tidal volume was 4–8 mls/kg, which meant that some infants may have received volumes above the “normal” tidal range [20]. We made the assumption that ETCO2 levels reflect changes in the arterial carbon dioxide levels, but this is not correct at the onset of resuscitation when ETCO2 levels may be as low as zero before the infant’s first active inspiration [18] and reflects lack of pulmonary vasodilation. We, however, analysed traces throughout the entirety of the recorded resuscitation, and in all cases, there were measurable ETCO2 levels during the resuscitation process. Although the ETCO2 levels may underestimate arterial CO2, there is no reason why this should differ between the groups, given our data do not suggest the IVH and BPD groups were sicker initially than those who did not develop those adverse outcomes. Our results are not from a randomised trial, but the researchers analysing the data were blind to the infants’ outcomes. The larger VT may be related to a sicker baby and a lower ETCO2 due to a higher physiological dead space, but we reported no significant differences in the Apgar scores of infants with and without adverse outcomes. Furthermore, the duration of resuscitation did not differ between those with and without adverse outcomes again suggesting those who developed an IVH or BPD were not initially sicker. Nevertheless, those who developed an IVH had both significantly more low ETCO2 levels and high tidal volumes. The inflation pressures used were those recommended by the Resuscitation Council (UK). The level of PEEP and flow rate were those routinely used in the UK, but in other countries, higher levels of PEEP are used. Whether the PEEP level might influence the results merits investigation. We did not collect data on possible confounders which occurred after resuscitation regarding the development of an IVH or BPD, but all IVHs had occurred on or before day 3, suggesting the delivery room events were associated with that adverse outcome.
In conclusion, infants who developed IVHs were resuscitated with significantly more inflations resulting in large tidal volumes and low ETCO2 levels after correcting for differences in gestational age and birth weight than those who did not develop IVHs.
Abbreviations
- BPD:
-
Bronchopulmonary dysplasia
- CO2 :
-
Carbon dioxide
- ETCO2 :
-
End tidal carbon dioxide
- FiO2 :
-
Inspired oxygen fraction
- IVH:
-
Intraventricular haemorrhage
- PEEP:
-
Positive end expiratory pressure
- VT :
-
Tidal volumes
- VTE :
-
Expiratory tidal volumes
References
Ambalavanan N, Carlow WA, Wrage LA, Das A, Laughon M, Cotton CM, Kennedy KA, Laptook AR, Shankaran S, Walsh MC, Higgins RD, Support Study Group of the NICHD Neonatal Research Network (2015) PaCO2 in surfactant, positive pressure and oxygenation randomised trial (SUPPORT). Arch Dis Child Fetal Neonatal Ed 100:F145–F149
Auden S, Smolkin T, Bental Y, Haramati Z, Blazer S, Litig E, Biton R, Dolberg S, Makhoul IR (2011) Does admission hypothermia predispose to intraventricular haemorrhage in very low birth weight infants? Neonatology 100:373–379
Balany J, Bhandari V (2015) Understanding the impact of infection, inflammation and their persistence in the pathogenesis of bronchopulmonary dysplasia. Front Med 2:90
Bjorklund LJ, Ingimarsson J, Curstedt T, John J, Robertson B, Werner O, Vilstrup CT (1997) Manual ventilation with a few large breaths at birth compromises the therapeutic effect of subsequent surfactant replacement in immature lambs. Pediatr Res 42:348–355
Chowdhury O, Bhat P, Rafferty GF, Hannam S, Milner AD, Greenough A (2016) In vitro assessment of the effect of proportional assist ventilation on the work of breathing. Eur J Pediatr 175:639–643
Dreyfuss D, Saumon G (1998) Ventilator-induced lung injury: lessons from experimental studies. Am J Respir Crit Care Med 157:294–323
Erickson SJ, Grauaug A, Gurrin L, Swaninathan M (2002) Hypercarbia in the ventilated preterm infants and its effect on intraventricular haemorrhage and bronchopulmonary dysplasia. J Paediatr Child Health 38:560–562
Fabres J, Carlo WA, Phillips V, Howard G, Ambalavanan N (2007) Both extremes of arterial carbon dioxide pressure and the magnitude of fluctuations in arterial carbon dioxide pressure are associated with severe intraventricular hemorrhage in preterm infants. Pediatrics 1199:299–305
Garland JS, Buck RK, Allred EN, Leviton A (1995) Hypocarbia before surfactant therapy appears to increase bronchopulmonary dysplasia risk in infants with respiratory distress syndrome. Arch Pediatr Adolesc Med 149:617–622
Hawkes GA, Finn D, Kenosi M, Livingstone V, O’Toole JM, Boylan GB, O’Halloran KD, Ryan AC, Dempsey EM (2017) A randomised controlled trial of end-tidal carbon dioxide detection of preterm infants in the delivery room. J Pediatr 182:74–78
Huang H, Cheung PY, O’Reilly M, van Os S, Solevag AL, Aziz K, Schmolzer GM (2017) Impact of changing clinical practices on early blood gas analyses in very preterm infants and their associated inpatient outcomes. Front Pediatr 5:11
Jobe AH, Bancalari E (2001) Bronchopulmonary dysplasia. Am J Respir Crit Care Med 163:1723–1729
Kong JY, Rich W, Finer NN, Leone TA (2013) Quantitative end-tidal carbon dioxide monitoring in the delivery room: a randomised controlled trial. J Pediatr 163:104–108
Kraybill EN, Runyan DK, Bose CL, Khan JH (1989) Risk factors for chronic lung disease in infants with birth weights of 751-1000 grams. J Pediatr 115:115–120
Mian Q, Cheung PY, O’Reilly M, Barton SK, Polglase GR, Schmolzer GM (2018) Impact of delivered tidal volume on the occurrence of intraventricular haemorrhage in preterm infants during positive pressure ventilation in the delivery room. Arch Dis Child Fetal Neonatal Ed
Milner A, Murthy V, Bhat P, Fox G, Campbell ME, Milner AD, Greenough A (2015) Evaluation of respiratory function monitoring at the resuscitation of prematurely born infants. Eur J Pediatr 174:205–208
Murthy V, Dattani N, Peacock JL, Fox GF, Campbell M, Milner AD, Greenough A (2012) The first five inflations during resuscitation of prematurely born infants. Arch Dis Child Fetal Neonatal Ed 97:F249–F253
Murthy V, O’Rourke-Potocki A, Dattani N, Fox GF, Campbell M, Milner AD, Greenough A (2012) End tidal carbon dioxide levels during the resuscitation of prematurely born infants. Early Hum Dev 88:783–787
O’Donnell CP, Schmolzer GM (2012) Resuscitation of preterm infants: delivery room interventions and their effect on outcomes. Clin Perinatol 39:857–869
Papile LA, Burstein J, Burstein R, Koffler H (1978) Incidence and evolution of subependymal and intraventricular haemorrhage: a study of infants with birth weights less than 1500 gm. J Pediatr 92:529–534
Patel DS, Sharma A, Prendergast M, Rafferty GF, Greenough A (2009) Work of breathing and different levels of volume-targeted ventilation. Pediatrics 123:e679–e684
Patel DS, Rafferty GF, Lee S, Hannam S, Greenough A (2010) Work of breathing and volume targeted ventilation in respiratory distress. Arch Dis Child Fetal Neonatal Ed 95:F443–F446
Resuscitation Council (UK) (2010) Newborn life support guidelines
Schmölzer GM, Mian Q, Cheung PY, O'Reilly M, Polglase G, Aziz K (2015) Tidal volume delivery during mask ventilation and brain injury in newborns <29 weeks gestation. Paediatr Child Health 20:e33–e34
Tracy M, Downe L, Holberton J (2004) How safe is intermittent positive pressure ventilation in preterm babies ventilated from delivery to newborn intensive care unit? Arch Dis Child Fetal Neonatal Med 89:F84–F87
Warner BB, Stuart LA, Papes RA, Wispe JR (1998) Functional and pathological effects of prolonged hyperoxia in neonatal mice. Am J Phys 275:L110–L117
Yee M, Chess PR, McGrath-Morrow SA, Wang Z, Gelein R, Zhou R, Dean DA, Notter RH, O’Reilly MA (2009) Neonatal oxygen adversely affects lung function in adult mice without altering surfactant composition or activity. Am J Physiol Lung Cell Mol Physiol 297:L641–L649
Zhang X, Wang H, Shi Y, Peng W, Zhang S, Zhang W, Xu J, Mei Y, Feng Z (2012) Role of bone marrow-derived mesenchymal stem cells in the prevention of hyperoxia induced lung injury in newborn mice. Cell Biol Int 36:589–594
Funding
Dr. Murthy was supported by a grant from the Guy’s and St Thomas’ Charity. Dr. Bhat and Dr. Hunt were supported by a grant from the Charles Wolfson Charitable Trust. Additionally, Dr. Hunt was supported by SLE. The research was supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Author information
Authors and Affiliations
Contributions
AP collected and analysed the data.
KH collected and analysed the data.
VM collected the data.
PB collected the data.
AG designed the study and analysed the data.
AM designed the study and analysed the data.
All the authors were involved in writing the manuscript and approved the final version.
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Infants whose parents gave informed, written consent were recruited.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Communicated by Patrick Van Reempts
Anoop Pahuja and Katie Hunt are joint first authors.
Rights and permissions
About this article
Cite this article
Pahuja, A., Hunt, K., Murthy, V. et al. Relationship of resuscitation, respiratory function monitoring data and outcomes in preterm infants. Eur J Pediatr 177, 1617–1624 (2018). https://doi.org/10.1007/s00431-018-3222-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-018-3222-y