Abstract
Purpose
Fetal cardiotocography is the most common method to assess fetal well-being during labor. Nevertheless, its predictive ability for acidemia is limited, both in low-risk and high-risk pregnancies (Nelson et al. in N Engl J Med 334: 613–9, 1996; Rinciples P et al. in Health and Human Development Workshop Report on Electronic Fetal Monitoring : Update on Definitions. no. 2007, 510–515, 2008), especially in high-risk pregnancies, such as those complicated by growth restriction. In this study we aim examine the association between deceleration and acceleration areas and other measure of fetal heart rate in intrapartum fetal monitoring and neonatal arterial cord blood pH in pregnancies complicated by growth restriction.
Materials and methods
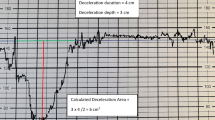
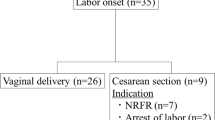
A retrospective cohort study of 100 deliveries complicated by growth restriction, delivered during 2018, was conducted. Known major fetal anomalies, non-vertex presentation and elective cesarean deliveries were excluded. Total deceleration and acceleration areas were calculated as the sum of the areas within the deceleration and acceleration, respectively.
Results
In deliveries complicated by growth restriction, cord blood pH is significantly associated with total deceleration area (p = 0.05) and correlates with cumulative duration of the decelerations (Spearman’s rank −0.363, p < 0.05), and total acceleration area (−0.358, p < 0.05). By comparing the cord blood pH in deliveries with a total deceleration area that was above and below the median total deceleration area, we demonstrated a significant difference between the categories.
Conclusions
Cord blood pH significantly correlates with total deceleration area and other fetal monitoring characteristics in neonates with growth restriction. Future studies using real-time, machine-learning based techniques of fetal heart rate monitoring, may provide population specific threshold values that will support bedside clinical decision making and perhaps achieve better outcomes.

Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Nelson KB, Dambrosia JM, Ting TY, Grether JK (1996) Uncertain value of electronic fetal monitoring in predicting cerebral palsyUncertain value of electronic fetal monitoring in predicting cerebral palsy. N Engl J Med 334(10):613–9
Rinciples P et al (2008) Health and Human Development Workshop Report on Electronic Fetal Monitoring : Update on Definitions. no. 2007, 510–515
Bailey RE (2019) Intrapartum fetal monitoring. Am Fam Physician 80(12):1388–1396
Ananth CV, Chauhan SP, Chen HY, D’Alton ME, Vintzileos AM (2013) Electronic fetal monitoring in the United States: temporal trends and adverse perinatal outcomes. Obstet Gynecol 121(5):927–933. https://doi.org/10.1097/AOG.0b013e318289510d
Khazin AF, Takemura H, Haven N (1970) Observations on heart rate and pH in the human fetus during labor. Obstet Gynecol Surv 25(2):115–118. https://doi.org/10.1097/00006254-197002000-00003
Robinson B (2008) A Review of NICHD standardized nomenclature for cardiotocography: the importance of speaking a common language when describing electronic fetal monitoring. Rev Obstet Gynecol 1(2):56–60
Ayres de Campos D, Spong CY, Chandraharan E, FIGO Intrapartum Fetal Monitoring Expert Consensus Panel (2015) FIGO consensus guidelines on intrapartum fetal monitoring: Cardiotocography. Int J Gynaecol Obstet 131(1):13–24. https://doi.org/10.1016/j.ijgo.2015.06.020
Cahill AG, Roehl KA, Macones GA, Odibo AO (2012) Association of atypical decelerations with acidemia. Obstetr Gynecol 120(6):1387–1393
Clark SL, Hamilton EF, Garite TJ, Timmins A, Warrick PA, Smith S (2017) The limits of electronic fetal heart rate monitoring in the prevention of neonatal metabolic acidemia. Am J Obstet Gynecol 216(2):163.e1-163.e6. https://doi.org/10.1016/j.ajog.2016.10.009
Andres RL et al (1999) Association between umbilical blood gas parameters and neonatal morbidity and death in neonates with pathologic fetal acidemia. Am J Obstet Gynecol 181(4):867–871. https://doi.org/10.1016/S0002-9378(99)70316-9
Yeh P, Emary K, Impey L (2012) The relationship between umbilical cord arterial pH and serious adverse neonatal outcome: analysis of 51,519 consecutive validated samples. BJOG Int J Obstet Gynaecol 119(7):824–831. https://doi.org/10.1111/j.1471-0528.2012.03335.x
Cahill AG, Tuuli MG, Stout MJ, López JD, Macones GA (2018) A prospective cohort study of fetal heart rate monitoring: deceleration area is predictive of fetal acidemia. Am J Obstet Gynecol 218(5):523.e1-523.e12. https://doi.org/10.1016/j.ajog.2018.01.026
Georgieva A (2021) Deceleration area and capacity during labour-like umbilical cord occlusions identify evolving hypotension: a controlled study in fetal sheep. BJOG: Int J Obstetr Gynaecol 128:1433–1442
Furukawa A, Neilson D, Hamilton E, Furukawa A, Neilson D, Cumulative EH (2019) Cumulative, “Cumulative deceleration area : a simplified predictor of metabolic acidemia.” J Matern Fetal Neonatal Med. https://doi.org/10.1080/14767058.2019.1678130
Lausman A et al (2013) Intrauterine growth restriction: screening, diagnosis, and management. J Obstet Gynaecol Can 35(8):741–748. https://doi.org/10.1016/S1701-2163(15)30865-3
Penn AA et al (2021) Placental contribution to neonatal encephalopathy. Semin Fetal Neonatal Med 26(4):101276. https://doi.org/10.1016/j.siny.2021.101276
Rosenberg A (2008) The IUGR newborn. Semin Perinatol 32(3):219–224. https://doi.org/10.1053/j.semperi.2007.11.003
Kramer MS, Olivier M, McLean FH, Willis DM, Usher RH (1990) Impact of intrauterine growth retardation and body proportionality on fetal and neonatal outcome. Pediatrics 86(5):707–713
Bernstein IM, Horbar JD, Badger GJ, Ohlsson A, Golan A (2000) Morbidity and mortality among very-low-birth-weight neonates with intrauterine growth restriction. The Vermont Oxford Network. Am J Obstet Gynecol 182(1 Pt 1):198–206. https://doi.org/10.1016/s0002-9378(00)70513-8
Dollberg S, Haklai Z, Mimouni FB, Gorfein I, Gordon E (2005) Birth weight standards in the live-born population in Israel. Isr Med Assoc J 7(5):311–314
Melamed N et al (2021) FIGO (international Federation of Gynecology and obstetrics) initiative on fetal growth: best practice advice for screening, diagnosis, and management of fetal growth restriction. Int J Gynaecol Obstet Off Organ Int Fed Gynaecol Obstet. 152:3–57. https://doi.org/10.1002/ijgo.13522
Abdi K et al (2022) Proceedings of the 13th International Newborn Brain Conference: Fetal and/or neonatal brain development, both normal and abnormal. J Neonatal-Perinat Med 15(2):411–426. https://doi.org/10.3233/NPM-229002
Geva Y et al (2022) Intrapartum deceleration and acceleration areas are associated with neonatal encephalopathy. Int J Gynaecol Obstet Off Organ Int Fed Gynaecol Obstet. https://doi.org/10.1002/ijgo.14638
Kubli FW, Hon EH, Khazin AF, Takemura H (1969) Observations on heart rate and pH in the human fetus during labor. Am J Obstet Gynecol 104(8):1190–1206. https://doi.org/10.1016/s0002-9378(16)34294-6
Cahill AG, Tuuli MG, Stout MJ, López JD, Macones GA (2018) A prospective cohort study of fetal heart rate monitoring: deceleration area is predictive of fetal acidemia. Am J Obstet Gynecol 218(5):523.e1-523.e12. https://doi.org/10.1016/j.ajog.2018.01.026
Gyllencreutz E, Varli IH, Lindqvist PG, Holzmann M (2021) Variable deceleration features and intrapartum fetal academia—the role of deceleration area. Eur J Obstet Gynecol Reprod Biol 267:192–197. https://doi.org/10.1016/j.ejogrb.2021.11.009
Dallasta A, Cagninelli G, Galli L, Frusca T, Ghi T (2021) Monitoring fetal well-being in labor in late fetal growth restriction. Minerva Obstet Gynecol 73(4):453–461. https://doi.org/10.23736/S2724-606X.21.04819-X
Hutcheon JA, Riddell CA, Himes KP (2021) A new approach for classifying fetal growth restriction. Epidemiol Camb Mass 32(6):860–867. https://doi.org/10.1097/EDE.0000000000001399
Geva N et al (2023) The association of intrapartum deceleration and acceleration areas with MRI findings in neonatal encephalopathy. Pediatr Res. https://doi.org/10.1038/s41390-023-02575-5
Morley LC, Debant M, Walker JJ, Beech DJ, Simpson NAB (2021) Placental blood flow sensing and regulation in fetal growth restriction. Placenta 113:23–28. https://doi.org/10.1016/j.placenta.2021.01.007
Macones GA, Hankins GDV, Spong CY, Hauth J, Moore T (2008) The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: update on definitions, interpretation, and research guidelines. Obstet Gynecol 112(3):661–666. https://doi.org/10.1097/AOG.0b013e3181841395
Gyllencreutz E et al (2018) Validation of a computerized algorithm to quantify fetal heart rate deceleration area. Acta Obstet Gynecol Scand 97(9):1137–1147. https://doi.org/10.1111/aogs.13370
Kouskouti C, Regner K, Knabl J, Kainer F (2017) Cardiotocography and the evolution into computerised cardiotocography in the management of intrauterine growth restriction. Arch Gynecol Obstet 295(4):811–816. https://doi.org/10.1007/s00404-016-4282-8
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
NG: manuscript writing and editing, data analysis. YG: data analysis, Manuscript editing. LK: data collection, Manuscript editing. YB: manuscript editing. RR: data analysis. AYW: project development, Manuscript editing. SYS: project development, Manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial personal, political, intellectual, or religious or other interests to disclose.
Ethical approval
This study received the approval of the Institutional Review Board (in accordance with the Helsinki declaration) at Soroka University Medical Center. The need for informed consent was waived as participants’ identities were kept strictly anonymous and data was retrospectively collected.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Geva, N., Geva, Y., Katz, L. et al. Correlation between total deceleration area in CTG records and cord blood pH in pregnancies with IUGR. Arch Gynecol Obstet (2024). https://doi.org/10.1007/s00404-023-07240-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00404-023-07240-0