Abstract
Introduction
Tranexamic acid (TXA) administration is supported by numerous evidence in reducing blood loss after total knee arthroplasty (TKA). The combination of intravenous (IV) and intra-articular (IA) TXA administration revealed good result in blood loss reduction with less evidence of venous thromboembolism event (VTE). Several literature reviews portray that peri-articular (PA) administration yields similar hemostasis in comparison to IV route. However, there is no report on the clinical effect of combining PA + IA TXA in blood loss reduction and its complications, compared to combining IV + IA TXA after TKA.
Materials and methods
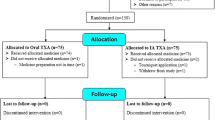
We conducted a double-blind, randomized controlled trial comparing the use of PA + IA TXA administration and IV + IA TXA administration in 70 patients who were scheduled for unilateral primary TKA. Thirty-five patients were assigned for PA + IA injection (Group 1) and anoter 35 patients were assigned for IV + IA injection (Group 2). Primary outcomes included total blood loss at 48 h, and the need for blood transfusion. Secondary outcomes included thigh and leg circumference, degree of knee flexion, and postoperative complications.
Results
The calculated blood loss at 48 h showed no difference between Groups 1 and 2 (617 ml vs. 632 ml, p = 0.425). The total hemoglobin and hematocrit changes were not different (1.89 g/dL vs. 1.97 g/dL, p = 0.371 and 5.66% vs. 5.87%, p = 0.391). There was no need for blood transfusion in either group. However, lower thigh swelling was significant in Group 1 (2.15 cm vs. 2.79 cm, p = 0.04). Leg circumferences at 48 h was also lower in Group 1 (42.12 cm vs. 42.77 cm, p = 0.04). There was no significant difference in knee flexion decrease between the two groups (38° vs. 37°, p = 0.425). There were no VTE complications or infections found in either group.
Conclusions
Combined PA + IA TXA administration had similar efficacy in blood loss reduction and blood transfusion when compared to combined IV + IA TXA. The first group displayed less soft tissue swelling. The combination of PA + IA TXA administration can be used as an alternative regimen to avoid IV TXA administration.

Similar content being viewed by others
References
Madjdpour C, Spahn DR (2005) Allogeneic red blood cell transfusions: efficacy, risks, alternatives and indications. Br J Anaesth 95(1):33–42. https://doi.org/10.1093/bja/aeh290
Fiebig E (1998) Safety of the blood supply. Clin Orthop Relat Res 3576–18. https://doi.org/10.1097/00003086-199812000-00003
Sabbag OD, Abdel MP, Amundson AW, Larson DR, Pagnano MW (2017) Tranexamic acid was safe in Arthroplasty patients with a history of venous thromboembolism: a matched outcome study. J Arthroplasty 32(9s):S246–s250. https://doi.org/10.1016/j.arth.2017.02.008
Fillingham YA, Ramkumar DB, Jevsevar DS et al (2019) Tranexamic acid in total joint arthroplasty: the endorsed clinical practice guides of the American Association of Hip and knee surgeons, American Society of Regional Anesthesia and Pain Medicine, American Academy of Orthopaedic Surgeons, Hip Society, and Knee Society. Reg Anesth Pain Med 44(1):7–11. https://doi.org/10.1136/rapm-2018-000024
Kim TK, Chang CB, Koh IJ (2014) Practical issues for the use of tranexamic acid in total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc 22(8):1849–1858. https://doi.org/10.1007/s00167-013-2487-y
Porter SB, White LJ, Osagiede O, Robards CB, Spaulding AC (2020) Tranexamic acid administration is not Associated with an increase in complications in high-risk patients undergoing primary total knee or total hip arthroplasty: a retrospective case-control study of 38,220 patients. J Arthroplasty 35(1):45–51e43. https://doi.org/10.1016/j.arth.2019.08.015
Whiting DR, Gillette BP, Duncan C, Smith H, Pagnano MW, Sierra RJ (2014) Preliminary results suggest tranexamic acid is safe and effective in arthroplasty patients with severe comorbidities. Clin Orthop Relat Res 472(1):66–72. https://doi.org/10.1007/s11999-013-3134-0
Fillingham YA, Ramkumar DB, Jevsevar DS et al (2018) The Safety of Tranexamic Acid in Total Joint Arthroplasty: a direct Meta-analysis. J Arthroplasty 33(10):3070–3082e3071. https://doi.org/10.1016/j.arth.2018.03.031
Gianakos AL, Hurley ET, Haring RS, Yoon RS, Liporace FA (2018) Reduction of blood loss by Tranexamic Acid following total hip and knee arthroplasty: a Meta-analysis. JBJS Rev 6(5):e1. https://doi.org/10.2106/JBJS.RVW.17.00103
**ong H, Liu Y, Zeng Y, Wu Y, Shen B (2018) The efficacy and safety of combined administration of intravenous and topical tranexamic acid in primary total knee arthroplasty: a meta-analysis of randomized controlled trials. BMC Musculoskelet Disord 19(1):321. https://doi.org/10.1186/s12891-018-2181-9
Pinsornsak P, Rojanavijitkul S, Chumchuen S (2016) Peri-articular tranexamic acid injection in total knee arthroplasty: a randomized controlled trial. BMC Musculoskelet Disord 17:313. https://doi.org/10.1186/s12891-016-1176-7
Zhang S, Wang C, Shi L, Xue Q (2019) Multi-route applications of tranexamic acid to reduce blood loss after total knee arthroplasty: a randomized controlled trial. Med (Baltim) 98(30):e16570. https://doi.org/10.1097/MD.0000000000016570
Nadler SB, Hidalgo JH, Bloch T (1962) Prediction of blood volume in normal human adults. Surgery 51(2):224–232
Wu JZ, Liu PC, Ge W, Cai M (2016) A prospective study about the preoperative total blood loss in older people with hip fracture. Clin Interv Aging 11:1539–1543. https://doi.org/10.2147/cia.S120526
Wei W, Dang S, Duan D, Wei L (2018) Comparison of intravenous and topical tranexamic acid in total knee arthroplasty. BMC Musculoskelet Disord 19(1):191. https://doi.org/10.1186/s12891-018-2122-7
Nielsen CS, Jans O, Orsnes T, Foss NB, Troelsen A, Husted H (2016) Combined intra-articular and intravenous tranexamic acid reduces blood loss in total knee arthroplasty: a Randomized, Double-Blind, placebo-controlled trial. J Bone Joint Surg Am 98(10):835–841. https://doi.org/10.2106/JBJS.15.00810
Tsukada S, Wakui M (2017) Combined intravenous and intra-articular tranexamic acid in simultaneous bilateral total knee arthroplasty without Tourniquet Use. JB JS Open Access 2(2):e0002. https://doi.org/10.2106/JBJS.OA.17.00002
Mi B, Liu G, Lv H et al (2017) Is combined use of intravenous and intraarticular tranexamic acid superior to intravenous or intraarticular tranexamic acid alone in total knee arthroplasty? A meta-analysis of randomized controlled trials. J Orthop Surg Res 12(1):61. https://doi.org/10.1186/s13018-017-0559-2
Jules-Elysee KM, Tseng A, Sculco TP et al (2019) Comparison of topical and intravenous tranexamic acid for total knee replacement: a Randomized double-blinded controlled study of effects on tranexamic acid levels and thrombogenic and inflammatory marker levels. J Bone Joint Surg Am 101(23):2120–2128. https://doi.org/10.2106/JBJS.19.00258
Pinsornsak P, Phunphakchit J, Boontanapibul K (2021) Efficacy and Systemic Absorption of Peri-articular Versus Intra-articular Administration of Tranexamic Acid in total knee arthroplasty: a prospective Randomized Controlled Trial. Arthroplast Today 11:1–5. https://doi.org/10.1016/j.artd.2021.06.005
Fillingham YA, Ramkumar DB, Jevsevar DS et al (2018) The efficacy of Tranexamic Acid in total knee arthroplasty: a Network Meta-Analysis. J Arthroplasty 33(10):3090–3098e3091. https://doi.org/10.1016/j.arth.2018.04.043
Zhang YM, Yang B, Sun XD, Zhang Z (2019) Combined intravenous and intra-articular tranexamic acid administration in total knee arthroplasty for preventing blood loss and hyperfibrinolysis: a randomized controlled trial. Med (Baltim) 98(7):e14458. https://doi.org/10.1097/MD.0000000000014458
Fan D, Ma J, Liu X, Zhang L (2022) Peri-articular administration of tranexamic acid is an alternative route in total knee arthroplasty: a systematic review and meta-analysis. J Orthop Surg Res 17(1):211. https://doi.org/10.1186/s13018-022-03095-4
Hirose H, Ogawa H, Matsumoto K, Akiyama H (2019) Periarticular injection of tranexamic acid promotes early recovery of the range of knee motion after total knee arthroplasty. J Orthop Surg (Hong Kong) 27(3):2309499019864693. https://doi.org/10.1177/2309499019864693
Richardson MK, Liu KC, Mayfield CK, Kistler NM, Lieberman JR, Heckmann ND (2024) Tranexamic acid is safe in patients with a history of venous thromboembolism undergoing total joint arthroplasty. J Bone Joint Surg Am 106(1):30–38. https://doi.org/10.2106/JBJS.23.00254
Acknowledgements
We thank Mr. Michael Everts for reviewing the article and language help. We also thank all participants for providing the data used in this study.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Piya Pinsornsak, Ranet Thaveekitikul and Prem Pinsornsak. The first draft of the manuscript was written by Yot Tanariyakul and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Thammasat University (MTU-EC-OT-1-277/61).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
The authors affirm that human research participants provided informed consent for publication of the images in Fig. 1.
Conflict of interest
All the authors declare no conflict of interest.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pinsornsak, P., Thaveekitikul, R., Pinsornsak, P. et al. Comparative effectiveness of combined peri-articular and intra-articular injection versus intravenous and intra-articular injection of tranexamic acid in total knee arthroplasty: a randomized controlled trial study. Arch Orthop Trauma Surg 144, 2753–2759 (2024). https://doi.org/10.1007/s00402-024-05337-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-024-05337-y