Abstract
Introduction
Despite the existence of diverse total knee implant designs, few data is available on the relationship between the level of implant constraint and the postoperative joint stability in the frontal plane and strain in the collateral ligaments. The current study aimed to document this relation in an ex vivo setting.
Materials and methods
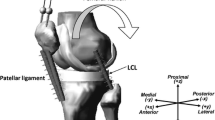
Six fresh-frozen lower limbs underwent imaging for preparation of specimen-specific surgical guides. Specimens were dissected and assessed for joint laxity using the varus–valgus stress tests at fixed knee flexion angles. A handheld dynamometer applied tensile loads at the ankle, thereby resulting in a knee abduction–adduction moment of 10 Nm. Tibiofemoral kinematics were calculated using an optical motion capture system, while extensometers attached to medial collateral (MCL) and lateral collateral ligament (LCL) measured strain. Native joint testing was followed by four TKA designs from a single implant line—cruciate retaining, posterior stabilised, varus–valgus constrained and hinged knee (HK)—and subsequent testing after each implantation. Repeated measures linear mixed-models (p < 0.05) were used to compare preoperative vs. postoperative data on frontal plane laxity and collateral ligament strain.
Results
Increasing implant constraint reduced frontal plane laxity across knee flexion, especially in deep flexion (r2 > 0.76), and MCL strain in extension; however, LCL strain reduction was not consistent. Frontal plane laxity increased with knee flexion angle, but similar trends were inconclusive for ligament strain. HK reduced joint laxity and ligament strain as compared to the native condition consistently across knee flexion angle, with significant reductions in flexion (p < 0.024) and extension (p < 0.001), respectively, thereby elucidating the implant design-induced joint stability. Ligament strain exhibited a strong positive correlation with varus–valgus alignment (r2 = 0.96), notwithstanding knee flexion angle or TKA implant design.
Conclusion
The study demonstrated that increasing the constraint of a TKA resulted in lower frontal plane laxity of the knee. With implant features impacting laxity in the coronal plane, consequentially affecting strain in collateral ligaments, surgeons must consider these factors when deciding a TKA implant, especially for primary TKA.
Level of evidence
V.






Similar content being viewed by others
References
Sharkey PF, Lichstein PM, Shen C, Tokarski AT, Parvizi J (2014) Why are total knee arthroplasties failing today—has anything changed after 10 years? J Arthroplasty 29:1774–1778. https://doi.org/10.1016/j.arth.2013.07.024
Song SJ, Park CH, Bae DK (2019) What to know for selecting cruciate-retaining or posterior-stabilized total knee arthroplasty. Clin Orthop Surg 11(2):142–150. https://doi.org/10.4055/cios.2019.11.2.142
Crawford DA, Lombardi AV Jr (2021) Ligament balancing and constraint in revision total knee arthroplasty. J Knee Surg 34(13):1382–1387. https://doi.org/10.1055/s-0041-1735162
Castagnini F, Bordini B, Cosentino M, Ancarani C, Lucchini S, Bracci G, Traina F (2022) Constraint in complex primary total knee arthroplasty: rotating hinge versus condylar constrained implants. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-04322-z
Grood E, Suntay W (1983) A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng 150:136–144. https://doi.org/10.1115/1.3138397
LaPrade RF, Bernhardson AS, Griffith CJ, MacAlena JA, Wijdicks CA (2010) Correlation of valgus stress radiographs with medial knee ligament injuries: an in vitro biomechanical study. Am J Sports Med 38:330–338. https://doi.org/10.1177/0363546509349347
LaPrade RF, Heikes C, Bakker AJ, Jakobsen RB (2008) The reproducibility and repeatability of varus stress radiographs in the assessment of isolated fibular collateral ligament and grade-III posterolateral knee injuries. An in vitro biomechanical study. J Bone Joint Surg Am 90:2069–2076. https://doi.org/10.2106/JBJS.G.00979
Delport H, Labey L, Innocenti B, De Corte R, Vander Sloten J, Bellemans J (2015) Restoration of constitutional alignment in TKA leads to more physiological strains in the collateral ligaments. Knee Surg Sports Traumatol Arthrosc 23:2159–2169. https://doi.org/10.1007/s00167-014-2971-z
Ghosh KM, Manning WA, Blain AP, Rushton SP, Longstaff LM, Amis AA, Deehan DJ (2016) Influence of increasing construct constraint in the presence of posterolateral deficiency at knee replacement: a biomechanical study. J Orthop Res 34(3):427–434. https://doi.org/10.1002/jor.23026
Manning WA, Ghosh K, Blain A, Longstaff L, Deehan DJ (2017) Tibiofemoral forces for the native and post-arthroplasty knee: relationship to maximal laxity through a functional arc of motion. Knee Surg Sports Traumatol Arthrosc 25:1669–1677. https://doi.org/10.1007/s00167-016-4093-2
Hunt NC, Ghosh KM, Blain AP, Athwal KK, Rushton SP, Amis AA, Longstaff LM, Deehan DJ (2014) How does laxity after single radius total knee arthroplasty compare with the native knee? J Orthop Res 32:1208–1213. https://doi.org/10.1002/jor.22645
Cheung A, Yan CH, Chan PK, Chiu KY (2020) The medial collateral ligament in primary total knee arthroplasty: anatomy, biomechanics, and injury. J Am Acad Orthop Surg 28(12):e510–e516. https://doi.org/10.5435/JAAOS-D-19-00355
Delport H, Labey L, De Corte R, Innocenti B, Vander Sloten J, Bellemans J (2013) Collateral ligament strains during knee joint laxity evaluation before and after TKA. Clin Biomech (Bristol, Avon) 28(7):777–782. https://doi.org/10.1016/j.clinbiomech.2013.06.006
Becker R, Hirschmann MT, Karlsson J (2017) The role of ligament tension and sensomotoric system in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:1663–1665. https://doi.org/10.1007/s00167-017-4581-z
Colyn W, Neirynck J, Vanlommel E, Bruckers L, Bellemans J (2022) Primary constrained-condylar-knee designs outperform posterior-stabilized and cruciate-retaining designs in high-grade varus osteoarthritic knees during short-term follow-up: a pilot study. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-022-04447-9
Heyse TJ, Tucker SM, Rajak Y, Kia M, Lipman JD, Imhauser CW, Westrich GH (2015) Frontal plane stability following UKA in a biomechanical study. Arch Orthop Trauma Surg 135:857–865. https://doi.org/10.1007/s00402-015-2198-6
Lujan TJ, Dalton MS, Thompson BM, Ellis BJ, Weiss JA (2007) Effect of ACL deficiency on MCL strains and joint kinematics. J Biomech Eng 129:386. https://doi.org/10.1115/1.2720915
Robinson JR, Bull AMJ, Thomas RRDW, Amis AA (2006) The role of the medial collateral ligament and posteromedial capsule in controlling knee laxity. Am J Sports Med 34:1815–1823. https://doi.org/10.1177/0363546506289433
Barsoum WK, Lee HH, Murray TG, Colbrunn R, Klika AK, Butler S, Van Den Bogert AJ (2011) Robotic testing of proximal tibio-fibular joint kinematics for measuring instability following total knee arthroplasty. J Orthop Res 29:47–52. https://doi.org/10.1002/jor.21207
Heyse TJ, Slane J, Peersman G, Dirckx M, van de Vyver A, Dworschak P, Fuchs-Winkelmann S, Scheys L (2017) Kinematics of a bicruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25(6):1784–1791. https://doi.org/10.1007/s00167-016-4414-5
Victor J, Labey L, Wong P, Innocenti B, Bellemans J (2010) The influence of muscle load on tibiofemoral knee kinematics. J Orthop Res 28:419–428. https://doi.org/10.1002/jor.21019
Acknowledgements
The authors gratefully acknowledge the contributions of Mr. Kristof Reyniers and Mr. Jo Verbinnen in preparing the specimens.
Funding
Smith and Nephew provided financial support and contributed to the study design and data collection.
Author information
Authors and Affiliations
Contributions
PB was involved in the study design, data acquisition, data interpretation, manuscript preparation and manuscript review. DSS was involved in the data analysis, data interpretation, manuscript preparation and manuscript review. OT was involved in the study design, data acquisition, data analysis, data interpretation and manuscript review. JS was involved in the study design, data acquisition and manuscript review. RDC was involved in data interpretation and manuscript review. LS was involved in the study design, data interpretation and manuscript review. HV was involved in the study design, data interpretation and manuscript review. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The author’s institution (IORT) receives research funding from Smith and Nephew. RD is an employee of Smith and Nephew. No other conflicts of interest.
Ethical approval
Ethical approval obtained for the cadaver study from the local research ethics committee (NH019, dated 2016-06-03).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Berger, P., Shah, D.S., Taylan, O. et al. Impact of increasing total knee replacement constraint within a single implant line on coronal stability: an ex vivo investigation. Arch Orthop Trauma Surg 143, 2165–2173 (2023). https://doi.org/10.1007/s00402-022-04534-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04534-x