Abstract
Purpose
Ventriculoatrial (VA) and ventriculopleural (VPL) shunts are used as alternatives when CSF diversion to the peritoneal compartment with a ventriculoperitoneal (VP) shunt is not possible. The objective of this study is to compare directly the shunt survival and complications for both procedures in this setting in children.
Methods
A retrospective analysis of 54 consecutive patients who underwent VA (36) or VPL (18) shunt insertion between January 2002 and December 2017 was conducted.
Results
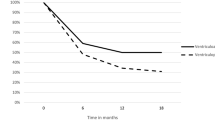
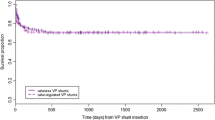
The overall mean follow-up was 4.1 (SD 4.3) years, 2.8 (SD 4.1) for VPL and 4.7 (SD 4.4) for VA shunts, respectively (p = 0.11). Twenty-four (66.7%) patients in the VA group and 9 (50.0%) in the VPL group underwent shunt revision (p = 0.236); mean number of revisions was 2.2 (SD 3.0) and 0.94 (SD 1.4) in the VA and VPL groups (p = 0.079). Median time to failure was 8.5 (IQr 78, range 0–176) months for VA and 5.50 (IQr 36, range 0–60) for VPL shunts (log rank (Mantel-Cox) 0.832). Shunt survival at 3, 6, 12 and 30 months was 60.6, 51.5, 36.4 and 27.3%, respectively, for VA and 56.3, 43.8, 37.5 and 37.5% for VPL shunts (log rank (Mantel-Cox) test value 0.727). The infection rate was 13.8% for VA and 5.6% for VPL shunts (p = 0.358). Four patients with VPL shunts (22.2%) developed pleural effusions. Fourteen deaths (25.9%) were recorded during follow-up, 8 (22.2%) in the VA and 6 (33.3%) in the VPL group (p = 0.380); two of the deaths in the VA group were shunt-related.
Conclusion
This study demonstrates that the outcomes of VA and VPL shunts, when used as second-line surgical treatment in paediatric hydrocephalus, were similar, as were the revision, infection and survival rates. The shorter longevity of these shunts compared with the general shunted population may reflect the complex nature of these children.

Similar content being viewed by others
References
Limbrick DD, Baird LC, Klimo P, Riva-Cambrin J, Flannery AM (2014) Pediatric hydrocephalus: systematic literature review and evidence-based guidelines. Part 4: cerebrospinal fluid shunt or endoscopic third ventriculostomy for the treatment of hydrocephalus in children J Neurosurg Pediatr 14 Suppl 1:30–34
Wright Z, Larrew TW, Eskandari R (2016) Pediatric hydrocephalus: current state of diagnosis and treatment. Pediatr Rev 37:478–490
Nulsen FE, Spitz EB (1951) Treatment of hydrocephalus by direct shunt from ventricle to jugular vain. Surg Forum:399–403
Hoffman HJ, Hendrick EB, Humphreys RP (1983) Experience with ventriculo-pleural shunts. Childs Brain 10:404–413
Jones RF, Currie BG, Kwok BC (1988) Ventriculopleural shunts for hydrocephalus: a useful alternative. Neurosurgery 23:753–755
Richardson MD, Handler MH (2013) Minimally invasive technique for insertion of ventriculopleural shunt catheters. J Neurosurg Pediatr 12:501–504
Zaman M, Akram H, Haliasos N, Bavetta S (2011) Cardiac tamponade and heart failure secondary to ventriculo-pleural shunt malfunction: a rare presentation. BMJ Case Rep 2011:bcr1220092548. https://doi.org/10.1136/bcr.12.2009.2548
Iosif G, Fleischman J, Chitkara R (1991) Empyema due to ventriculopleural shunt. Chest 99:1538–1539
Clark DJ, Chakraborty A, Roebuck DJ, Thompson DNP (2016) Ultrasound guided placement of the distal catheter in paediatric ventriculoatrial shunts-an appraisal of efficacy and complications. Childs Nerv Syst 32:1219–1225
Craven C, Asif H, Farrukh A, Somavilla F, Toma AK, Watkins L (2017) Case series of ventriculopleural shunts in adults: a single-center experience. J Neurosurg 126:2010–2016
Mazza C, Pasqualin A, Da Pian R (1980) Results of treatment with ventriculoatrial and ventriculoperitoneal shunt in infantile nontumoral hydrocephalus. Childs Brain 7:1–14
Girotti ME, Singh RR, Rodgers BM (2009) The ventriculo-gallbladder shunt in the treatment of refractory hydrocephalus: a review of the current literature. Am Surg 75:734–737
Matushita H, Cardeal D, Pinto FC, Plese JPP, de Miranda JS (2008) The ventriculoomental bursa shunt. Childs Nerv Syst 24:949–953
Beuriat P-A, Puget S, Cinalli G, Blauwblomme T, Beccaria K, Zerah M, Sainte-Rose C (2017) Hydrocephalus treatment in children: long-term outcome in 975 consecutive patients. J Neurosurg Pediatr 20:10–18
Paulsen AH, Lundar T, Lindegaard K-F (2010) Twenty-year outcome in young adults with childhood hydrocephalus: assessment of surgical outcome, work participation, and health-related quality of life. J Neurosurg Pediatr 6:527–535
Vinchon M, Rekate H, Kulkarni AV (2012) Pediatric hydrocephalus outcomes: a review. Fluids Barriers CNS 9:18
Drake JM, Kestle JR, Milner R et al (1998) Randomized trial of cerebrospinal fluid shunt valve design in pediatric hydrocephalus. Neurosurgery 43:294–303 discussion 303–5
Pollack IF, Albright AL, Adelson PD (1999) A randomized, controlled study of a programmable shunt valve versus a conventional valve for patients with hydrocephalus. Hakim-Medos Investigator Group Neurosurgery 45:1399–1408 discussion 1408–11
Riva-Cambrin J, Kestle JRW, Holubkov R, Butler J, Kulkarni AV, Drake J, Whitehead WE, Wellons JC, Shannon CN, Tamber MS, Limbrick DD, Rozzelle C, Browd SR, Simon TD, _ _ (2016) Risk factors for shunt malfunction in pediatric hydrocephalus: a multicenter prospective cohort study. J Neurosurg Pediatr 17:382–390
Tervonen J, Leinonen V, Jääskeläinen JE, Koponen S, Huttunen TJ (2017) Rate and risk factors for shunt revision in pediatric patients with hydrocephalus-a population-based study. World Neurosurg 101:615–622
Kulkarni AV, Riva-Cambrin J, Butler J, Browd SR, Drake JM, Holubkov R, Kestle JRW, Limbrick DD, Simon TD, Tamber MS, Wellons JC, Whitehead WE, _ _ (2013) Outcomes of CSF shunting in children: comparison of hydrocephalus clinical research network cohort with historical controls: clinical article. J Neurosurg Pediatr 12:334–338
Paulsen AH, Lundar T, Lindegaard K-F (2015) Pediatric hydrocephalus: 40-year outcomes in 128 hydrocephalic patients treated with shunts during childhood. Assessment of surgical outcome, work participation, and health-related quality of life. J Neurosurg Pediatr 16:633–641
Fernell E, Wendt von L, Serlo W, Heikkinen E, Andersson H (1985) Ventriculoatrial or ventriculoperitoneal shunts in the treatment of hydrocephalus in children? Z Kinderchir 40(Suppl 1):12–14
White IK, Shaikh KA, Nyarenchi OM, Kundu MG, Boaz JC, Fulkerson DH (2015) Analysis of the potential risk of central intravenous lines and/or total parenteral nutrition with ventriculoatrial shunts. Childs Nerv Syst 31:563–568
Kulkarni AV, Drake JM, JRW K, Mallucci CL, Sgouros S, Constantini S, Canadian Pediatric Neurosurgery Study Group (2010) Endoscopic third ventriculostomy vs cerebrospinal fluid shunt in the treatment of hydrocephalus in children: a propensity score-adjusted analysis. Neurosurgery 67:588–593
Kulkarni AV, Riva-Cambrin J, Browd SR (2011) Use of the ETV Success Score to explain the variation in reported endoscopic third ventriculostomy success rates among published case series of childhood hydrocephalus. J Neurosurg Pediatr 7:143–146
Cochrane DD, Kestle J (2002) Ventricular shunting for hydrocephalus in children: patients, procedures, surgeons and institutions in English Canada, 1989-2001. Eur J Pediatr Surg 12(Suppl 1):S6–S11
Ransohoff J, SHULMAN K, FISHMAN RA (1960) Hydrocephalus: a review of etiology and treatment. J Pediatr 56:399–411
Piatt JH (1994) How effective are ventriculopleural shunts? Pediatr Neurosurg 21:66–70
Farach SM, Danielson PD, Chandler NM (2015) Diagnostic laparoscopy for intraabdominal evaluation and ventriculoperitoneal shunt placement in children: a means to avoid ventriculoatrial shunting. J Laparoendosc Adv Surg Tech A 25:151–154
Al-Schameri AR, Hamed J, Baltsavias G, Winkler P, Machegger L, Richling B, Emich S (2016) Ventriculoatrial shunts in adults, incidence of infection, and significant risk factors: a single-center experience. World Neurosurg 94:345–351
Simon TD, Kronman MP, Whitlock KB, Gove NE, Mayer-Hamblett N, Browd SR, Cochrane DD, Holubkov R, Kulkarni AV, Langley M, Limbrick DD, Luerssen TG, Oakes WJ, Riva-Cambrin J, Rozzelle C, Shannon C, Tamber M, Wellons JC, Whitehead WE, Kestle JRW (2018) Reinfection after treatment of first cerebrospinal fluid shunt infection: a prospective observational cohort study. J Neurosurg Pediatr 21:346–358
Steinbok P, Milner R, Agrawal D, Farace E, Leung GKK, Ng I, Tomita T, Wang E, Wang N, Chu Wong GK, Zhou LF (2010) A multicenter multinational registry for assessing ventriculoperitoneal shunt infections for hydrocephalus. Neurosurgery 67:1303–1310
Hanak BW, Bonow RH, Harris CA, Browd SR (2017) Cerebrospinal fluid shunting complications in children. Pediatr Neurosurg 52:381–400
Pascual JM, Prakash UB (1993) Development of pulmonary hypertension after placement of a ventriculoatrial shunt. Mayo Clin Proc 68:1177–1182
Author information
Authors and Affiliations
Contributions
Data collection and analysis: DF, SP, TH, KA; conception and design of the study: KA; analysis and discussion: SP, KA, GJ, DT; approval for publication: all authors.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any conflicts of interest or competing interests to declare.
Ethics approval
As this is a retrospective review, we are not required to obtain ethical approval from our institution or regional ethics board.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Forte, D., Peraio, S., Huttunen, T.J. et al. Ventriculoatrial and ventriculopleural shunts as second-line surgical treatment have equivalent revision, infection, and survival rates in paediatric hydrocephalus. Childs Nerv Syst 37, 481–489 (2021). https://doi.org/10.1007/s00381-020-04887-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-020-04887-x