Abstract
Objectives
To assess the contribution of whole-body magnetic resonance imaging (WBMRI) and bone scintigraphy (BS) in addition to skeletal survey (SS) in detecting traumatic bone lesions and soft-tissue injuries in suspected child abuse.
Methods
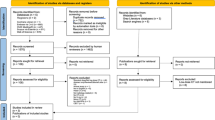
In this prospective, multicentre, diagnostic accuracy study, children less than 3 years of age with suspected physical abuse were recruited. Each child underwent SS, BS and WBMRI. A blinded first review was performed in consensus by five paediatric radiologists and three nuclear medicine physicians. A second review investigated discrepancies reported between the modalities using a consensus result of all modalities as the reference standard. We calculated the sensitivity, specificity and corresponding 95% confidence interval for each imaging modality (SS, WBMRI and BS) and for the combinations [SS + WBMRI] and [SS + BS].
Results
One hundred seventy children were included of which sixty-four had at least one lesion. In total, 146 lesions were included. The sensitivity and specificity of each examination were, respectively, as follows: 88.4% [95% CI, 82.0–93.1] and 99.7% [95% CI, 99.5–99.8] for the SS, 69.9% [95% CI, 61.7–77.2] and 99.5% [95% CI, 99.2–99.7] for WBMRI and 54.8% [95% CI, 46.4–63.0] and 99.7% [95% CI, 99.5–99.9] for BS. Sensitivity and specificity were, respectively, 95.9% [95% CI, 91.3–98.5] and 99.2% [95% CI, 98.9–99.4] for the combination SS + WBMRI and 95.2% [95% CI, 90.4–98.1] and 99.4% [95% CI, 99.2–99.6] for the combination SS + BS, with no statistically significant difference between them.
Conclusion
SS was the most sensitive independent imaging modality; however, the additional combination of either WBMRI or BS examinations offered an increased accuracy.
Key Points
• SS in suspected infant abuse was the most sensitive independent imaging modality in this study, especially for detecting metaphyseal and rib lesions, and remains essential for evaluation.
• The combination of either SS + BS or SS + WBMRI provides greater accuracy in diagnosing occult and equivocal bone injuries in the difficult setting of child abuse.
• WBMRI is a free-radiation technique that allows additional diagnosis of soft-tissue and visceral injuries.




Similar content being viewed by others
Abbreviations
- BS:
-
Bone scintigraphy
- CML :
-
Classic metaphyseal lesion
- FN:
-
False negative
- FP:
-
False positive
- FUSS:
-
Follow-up skeletal survey
- NPV:
-
Negative predictive value
- PEDIMA:
-
PEDiatric Imaging of Abuse
- PPV:
-
Positive predictive value
- SS:
-
Skeletal survey
- SPNBF:
-
Sub-periosteal new bone formation
- STIR:
-
Short tau inversion recovery
- TE:
-
Echo time
- TP:
-
True positive
- TR:
-
Repetition time
- WBMRI:
-
Whole-body magnetic resonance imaging
References
Leventhal JM, Martin KD, Asnes AG (2008) Incidence of fractures attributable to abuse in young hospitalized children: results from analysis of a United States database. Pediatrics 122:599–604
Wootton-Gorges SL, Soares BP, Alazraki AL et al (2017) ACR Appropriateness Criteria® suspected physical abuse—child. J Am Coll Radiol 14:S338–S349
Barber I, Perez-Rossello JM, Wilson CR, Kleinman PK (2015) The yield of high-detail radiographic skeletal surveys in suspected infant abuse. Pediatr Radiol 45:69–80
Haute Autorité de Santé - Syndrome du bébé secoué ou traumatisme crânien non accidentel par secouement. https://www.has-sante.fr/jcms/c_2794425/fr/syndrome-du-bebe-secoue-ou-traumatisme-cranien-non-accidentel-par-secouement. Accessed 20 Jan 2020
The radiological investigation of suspected physical abuse in children | The Royal College of Radiologists. https://www.rcr.ac.uk/publication/radiological-investigation-suspected-physical-abuse-children. Accessed 20 Jan 2020
Kleinman PK, Nimkin K, Spevak MR et al (1996) Follow-up skeletal surveys in suspected child abuse. Am J Roentgenol 167:893–896
Harper N, Lewis T, Eddleman S et al (2016) Follow-up skeletal survey use by child abuse pediatricians. Child Abuse Negl 51:336–342
Singh R, Squires J, Fromkin JB, Berger RP (2012) Assessing the use of follow-up skeletal surveys in children with suspected physical abuse. J Trauma Acute Care Surg 73:972–976
Sonik A, Stein-Wexler R, Rogers KK et al (2010) Follow-up skeletal surveys for suspected non-accidental trauma: can a more limited survey be performed without compromising diagnostic information? Child Abuse Negl 34:804–806
Bainbridge JK, Huey BM, Harrison SK (2015) Should bone scintigraphy be used as a routine adjunct to skeletal survey in the imaging of non-accidental injury? A 10 year review of reports in a single centre. Clin Radiol 70:e83–e89
Mandelstam SA, Cook D, Fitzgerald M, Ditchfield MR (2003) Complementary use of radiological skeletal survey and bone scintigraphy in detection of bony injuries in suspected child abuse. Arch Dis Child 88:387–390
Blangis F, Taylor M, Adamsbaum C et al (2020) Add-on bone scintigraphy after negative radiological skeletal survey for the diagnosis of skeletal injury in children suspected of physical abuse: a systematic review and meta-analysis. Arch Dis Child. https://doi.org/10.1136/archdischild-2020-319065
Van Rijn RR (2009) How should we image skeletal injuries in child abuse? Pediatr Radiol 39:226–229
Adamsbaum C, Méjean N, Merzoug V, Rey-Salmo C (2010) How to explore and report children with suspected non-accidental trauma. Pediatr Radiol 40:932–938
Chavhan GB, Babyn PS (2011) Whole-body MR imaging in children: principles, technique, current applications, and future directions. Radiographics 31:1757–1772
Perez-Rossello JM, Connolly SA, Newton AW et al (2010) Whole-body MRI in suspected infant abuse. Am J Roentgenol 195:744–750
Ruda MT, Greeley CS, Johnston JH, John SD (2016) Use of whole body MRI in detecting body injuries in suspected child abuse: a case report. J Forensic Radiol Imaging 5:59–61
Stranzinger E, Kellenberger CJ, Braunschweig S et al (2007) Whole-body STIR MR imaging in suspected child abuse: an alternative to skeletal survey radiography? Eur J Radiol Extra 63:43–47
Eltermann T, Beer M, Girschick HJ (2007) Magnetic resonance imaging in child abuse. J Child Neurol 22:170–175
Merlini L, Carpentier M, Ferrey S, Anooshiravani M, Poletti PA, Hanquinet S (2017) Whole-body MRI in children: would a 3D STIR sequence alone be sufficient for investigating common paediatric conditions? A comparative study. Eur J Radiol 88:155–162
Kleinman PK (2015) Diagnostic imaging of child abuse. Cambridge University Press, Cambridge
Sanchez TR, Grasparil AD, Chaudhari R, Coulter KP, Wootton-Gorges SL (2018) Characteristics of rib fractures in child abuse-the role of low-dose chest computed tomography. Pediatr Emerg Care 34:81–83
Shelmerdine SC, Langan D, Hutchinson JC et al (2018) Chest radiographs versus CT for the detection of rib fractures in children (DRIFT): a diagnostic accuracy observational study. Lancet Child Adolesc Health 2:802–811
Adamsbaum C, De Boissieu P, Teglas JP, Rey-Salmon C (2019) Classic metaphyseal lesions among victims of abuse. J Pediatr 209:154–159.e2
Thackeray JD, Wannemacher J, Adler BH, Lindberg DM (2016) The classic metaphyseal lesion and traumatic injury. Pediatr Radiol 46:1128–1133
Lindberg DM, Harper NS, Laskey AL, Berger RP (2013) Prevalence of abusive fractures of the hands, feet, spine, or pelvis on skeletal survey: perhaps “uncommon” is more common than suggested. Pediatr Emerg Care 29:26–29
Harlan SR, Nixon GW, Campbell KA et al (2009) Follow-up skeletal surveys for nonaccidental trauma: can a more limited survey be performed? Pediatr Radiol 39:962–968
Barber I, Perez-Rossello JM, Wilson CR et al (2013) Prevalence and relevance of pediatric spinal fractures in suspected child abuse. Pediatr Radiol 43:1507–1515
Sheets LK, Leach ME, Koszewski IJ et al (2013) Sentinel injuries in infants evaluated for child physical abuse. Pediatrics 131:701–707
Rutjes AW, Reitsma JB, Coomarasamy A, Khan KS, Bossuyt PM (2007) Evaluation of diagnostic tests when there is no gold standard. Health Technol Assess 11:1–86
Kemp A, Cowley L, Maguire S (2014) Spinal injuries in abusive head trauma: patterns and recommendations. Pediatr Radiol 44(Suppl 4):S604–S612
Acknowledgement
The PEDIMA Collaborative Study group includes the following: Lydie Abalea (Department of Pediatrics and Emergency Medicine, CHU Brest), Séverine Croly-Labourdette (Department of Pediatrics and Emergency Medicine, CHU Brest), Phong Dam Hieu (Department of Neurosurgery, CHU Brest), Murielle Dobrzynski (Pediatric Intensive Care Unit, CHU Brest), Bertrand Fenoll (Department of Pediatric Surgery, CHU Brest), Pierre Forlodou (Department of Pediatric Radiology, CHU Brest), Christiane Le Bot (Department of Pediatrics, CHU Brest), Jérémie Lefranc (Department of Pediatrics, CHU Brest), Mélanie Lesoeur (Department of Pediatric Radiology, CHU Brest), Philippe Meriot (Department of Pediatric Radiology, CHU Brest), Sylviane Peudenier (Department of Pediatrics, CHU Brest), Solène Querellou (Department of Nuclear Medicine, CHU Brest), Pierre-Yves Salaun (Department of Nuclear Medicine, CHU Brest), Pierre Olivier (Department of Nuclear Medicine, CHU Nancy), Laurent Martrille (Department of Forensic Medicine, CHU Nancy), Anne Borsa-Dorion (Department of Pediatrics and Emergency Medicine, CHU Nancy), Marie-Agnès Galloy (Department of Pediatric Radiology, CHU Nancy), Laurence Mainard-Simard (Department of Pediatric Radiology, CHU Nancy), Emmanuel Raffo (Department of Pediatrics, CHU Nancy), Sylvie Cavare-Vigneron (Department of Pediatrics and Emergency Medicine, CHU Nancy), Michel Claudon (Department of Pediatric Radiology, CHU Nancy), Olivier Klein (Department of Neurosurgery, CHU Nancy), Emmanuelle Schmitt (Department of Pediatric Radiology, CHU Nancy), Serge Le Tacon (Pediatric Intensive Care Unit, CHU Nancy), Olivier Morel (Department of Nuclear Medicine, CHU Nancy), Lucie Lapp (Department of Pediatrics and Emergency Medicine, CHU Nancy), Françoise Bodéré-Kraeber (Department of Nuclear Medicine, CHU Nantes), Caroline Bodet-Milin (Department of Nuclear Medicine, CHU Nantes), Juliette Fleury (Department of Pediatrics, CHU Nantes), Loïc Geffroy (Department of Pediatric Surgery, CHU Nantes), Sophie Hamel (Department of Pediatric Surgery, CHU Nantes), Antoine Hamel (Department of Pediatric Surgery, CHU Nantes), Thomas Lefrançois (Department of Pediatric Radiology,CHU Nantes), Marie-Pierre Longis (Department of Pediatric Surgery, CHU Nantes), Emmanuelle Mayrargue (Department of Pediatric Surgery, CHU Nantes), Georges Picherot (Department of Pediatrics, CHU Nantes), Marie-Pierre Quéré (Department of Pediatric Radiology, CHU Nantes), Jean-Christophe Rozé (Pediatric Intensive Care Unit, CHU Nantes), Nathalie Vabres (Department of Pediatrics, CHU Nantes), Renaud Bouvet (Department of Forensic Medicine, CHU Rennes), Mariannick Le Gueut (Department of Forensic Medicine, CHU Rennes), Laurent Riffaud (Department of Neurosurgery, CHU Rennes), Martine Balençon (Department of Pediatrics, CHU Rennes), Pierre Bétrémieux (Pediatric Intensive Care Unit, CHU Rennes), Bertrand Bruneau (Department of Pediatric Radiology, CHU Rennes), Madeleine Chapuis (Department of Pediatric Surgery, CHU Rennes), Véronique Chasle (Department of Pediatrics and Emergency Medicine, CHU Rennes), Alain Dabadie (Department of Pediatrics, CHU Rennes), Léna Damaj (Department of Pediatrics, CHU Rennes), Pierre Darnault (Department of Pediatric Radiology, CHU Rennes), François De La Brière (Department of Anesthesiology, CHU Rennes), Séverine Delahaye (Pediatric Intensive Care Unit, CHU Rennes), Régis Duvauferrier (Department of Pediatric Radiology, CHU Rennes), Céline Farges (Department of Pediatrics and Emergency Medicine, CHU Rennes), Bernard Fraisse (Department of Pediatric Surgery, CHU Rennes), Théophile Gaillot (Pediatric Intensive Care Unit, CHU Rennes), Maryse Gardin (Department of Anesthesiology, CHU, Rennes), Cécile Gauvrit (Department of Anesthesiology, CHU Rennes), Marie-Aline Guitteny (Department of Pediatrics and Emergency Medicine, CHU Rennes), Sylvette Marleix (Department of Pediatric Surgery, CHU Rennes), Silvia Napuri (Department of Pediatrics, CHU Rennes), Michel Roussey (Department of Pediatrics, CHU Rennes), Céline Rozel (Department of Pediatric Radiology, CHU Rennes), Olivier Tirel (Pediatric Intensive Care Unit, CHU, Rennes), Catherine Tréguier (Department of Pediatric Radiology, CHU Rennes), Catherine Vignaud (Department of Anesthesiology, CHU Rennes), Philippe Violas (Department of Pediatric Surgery, CHU Rennes), Eric Wodey (Department of Anesthesiology, CHU Rennes), Marion Pierre (Department of Pediatrics and Emergency Medicine, CHU Rennes), Patrick Pladys (Department of Pediatrics, CHU Rennes), Saad Abu-Amara (Department of Pediatric Surgery, CHU Rouen), Bruno Bachy (Department of Pediatric Surgery, CHU Rouen), Marie Brasseur-Daudruy (Department of Pediatric Radiology, CHU Rouen), Jean-Nicolas Dacher (Department of Radiology, CHU, Rouen), Pascal Delmon (Department of Anesthesiology, CHU Rouen), Joël Lechevallier Amara (Department of Pediatric Surgery, CHU,Rouen), Bénédicte Lerebours (Department of Pediatrics, CHU Rouen), Julien Leroux (Department of Pediatric Surgery, CHU, Rouen), François Proust (Department of Neurosurgery, CHU Rouen), Sophie Rigal (Department of Pediatrics and Emergency Medicine CHU Rouen), Pierre-Hugues Vivier (Department of Pediatric Radiology, CHU Rouen), Jean-Louis Baulieu (Department of Nuclear Medicine, CHU Tours), Yann Venel (Department of Nuclear Medicine, CHU Tours), Elodie Carpentier (Department of Pediatric Radiology, CHU Tours), Alain Chantepie (Department of Pediatrics, CHU Tours), Julie Chantreuil (Intensive Care Unit, CHU Tours), Mathieu Come (Department of Pediatrics and Emergency Medicine, CHU Tours), Benoît De Courtivron (Department of Pediatric Surgery, CHU Tours), François Labarthe (Department of Pediatrics, CHU Tours), Yves Marot (Department of Pediatrics and Emergency Medicine, CHU Tours), Myriam Pepin-Donat (Department of Pediatrics and Emergency Medicine, CHU Tours), Catherine Sembely-Taveau (Department of Pediatric Radiology, CHU Tours), Dominique Sirinelli (Department of Pediatric Radiology, CHU Tours), Nadine Travers (Department of Neurosurgery, CHU Tours), Annie Urvois-Grangé (Department of Pediatrics, CHU Tours), Patrick O’Byrne (Department of Forensic Medicine, CHU Tours), Antoine Listrat (Department of Neurosurgery, CHU Tours), Anne Devillers (Department of Nuclear Medicine, CRLC Rennes), Marie-Luce Barge-Galerne (Department of Nuclear Medicine, CRLC Rennes), Joseph Le Cloirec (Department of Nuclear Medicine, CRLC Rouen), Pierre Vera (Department of Nuclear Medicine, CRLC Rouen), Catherine Adamsbaum (Department of Pediatric Radiology, CHU Kremlin Bicêtre) Isabelle Koné-Paut (Department of Pediatrics, CHU Kremlin Bicêtre), Kumaran Deiva (Department of Pediatrics, CHU Kremlin Bicêtre), Philippe Chaumet-Riffaud (Department of Nuclear Medicine, CHU Kremlin Bicêtre), Gilles Grimon (Department of Nuclear Medicine, CHU Kremlin Bicêtre), Frédérique Archambaud (Department of Nuclear Medicine, CHU Kremlin Bicêtre), Ferielle Zenkhri (Department of Pediatrics and Emergency Medicine, CHU Kremlin Bicêtre), Caroline Galeotti (Department of Pediatrics, CHU Kremlin Bicêtre), Nancy Sevette-Béchard (Department of Pediatric Radiology, CHU Montpellier), Olivier Prodhomme (Department of Pediatric Radiology, CHU Montpellier), Céline Leconte (Department of Forensic Medicine, CHU Montpellier), Armelle Haquet (Department of Pediatrics and Emergency Medicine, CHU Montpellier), Aurélie Bourdon (Department of Nuclear Medicine, CHU Montpellier), Mélanie Sainmont (Department of Nuclear Medicine, CHU Montpellier), Loïc De Pontual (Department of Pediatrics, CHU Bondy), Nicolas Sellier (Department of Pediatric Radiology, CHU, Bondy), Thanh-Van Trieu (Department of Pediatrics and Emergency Medicine, CHU Bondy), and Claire De Labriolle-Vaylet (Department of Nuclear Medicine, CHU Trousseau Paris). We thank our radiologist, nuclear medicine physicians and technicians colleagues who helped during the research study; pediatricians with dedicated training in abuse from all the centers for patient inclusion in the study; colleagues of the Public Health and Epidemiology Department for the statistical study and management of images; and Tracey Westcott for English languge editing.
Funding
This study has received funding from the French Ministry for Health as part of its interregional PHRC (grant number API11/R/051). The funder of the study had no role in study design, data collection, data analysis, data interpretation or writing of the report.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr Catherine Treguier.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
Dr. Emma Bajeux and Stephanie Hamonic kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Prospective
• Diagnostic or prognostic study
• Multicentre study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Study group members are listed at the end of the article.
Rights and permissions
About this article
Cite this article
Proisy, M., Vivier, PH., Morel, B. et al. Whole-body MR imaging in suspected physical child abuse: comparison with skeletal survey and bone scintigraphy findings from the PEDIMA prospective multicentre study. Eur Radiol 31, 8069–8080 (2021). https://doi.org/10.1007/s00330-021-07896-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-07896-9