Abstract
Objective
The aim of our study was to evaluate the clinical feasibility and diagnostic value of a new MRI metal artefact reduction pulse sequence called MAVRIC-SL in a 3 T MRI environment.
Subjects and methods
Two MAVRIC-SL sequences obtained in 61 patients with symptomatic total hip replacement were compared with standard FSE-STIR sequences optimized for imaging around metal. Artefact size was measured on the slice of greatest extent. Image quality, fat saturation, image distortion, visibility of anatomical structures, and detectability of joint abnormalities were visually assessed and graded on qualitative scales. Differences between MAVRIC-SL and FSE sequences were tested with the Wilcoxon signed-rank test.
Results
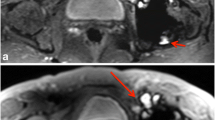
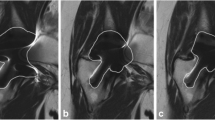
MAVRIC-SL sequences at 3 T showed significantly smaller metal artefacts compared to FSE-STIR sequences (p < 0.0001). The general image quality of MAVRIC-SL sequences was reduced with regard to spatial resolution, noise and contrast (p = 0.001), and fat saturation (p < 0.0001). The reduction of artefact size and image distortion significantly improved visualization of joint anatomy (p < 0.0001) and diagnostic confidence regarding implant-associated abnormalities (p = 0.0075 to <0.0001).
Conclusion
Although the image quality of MAVRIC-SL sequences is limited at 3 T, its clinical application is feasible and provides important additional diagnostic information for the workup of patients with symptomatic hip replacement through substantially reduced metal artefacts.
Key Points
• Metal artefacts compromise imaging of total hip replacement with MRI.
• Metal artefacts are aggravated with 3 Tesla MRI.
• MAVRIC-SL is a technique to suppress metal artefacts.
• MAVRIC-SL effectively reduces metal artefacts at 3 Tesla and improves diagnostic quality.







Similar content being viewed by others
References
Le DH, Goodman SB, Maloney WJ, Huddleston JI (2014) Current Modes of Failure in TKA: Infection, Instability, and Stiffness Predominate. Clin Orthop Relat Res 472:2197–2200
Gallo J, Goodman SB, Konttinen YT, Raska M (2013) Particle disease: biologic mechanisms of periprosthetic osteolysis in total hip arthroplasty. Innate Immun 19:213–224
Williams DH, Greidanus NV, Masri BA, Duncan CP, Garbuz DS (2011) Prevalence of pseudotumor in asymptomatic patients after metal-on-metal hip arthroplasty. J Bone Joint Surg Am 93:2164–2171
Willert HG, Buchhorn GH, Fayyazi A, Flury R et al (2005) Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study. J Bone Joint Surg Am 87:28–36
Culliford D, Maskell J, Judge A, Arden NK, the COAST Study group (2013) A population-based survival analysis describing the association of body mass index on time to revision for total hip and knee replacements: results from the UK general practice research database. BMJ Open 3:e003614
Shon WY, Gupta S, Biswal S, Han SH et al (2009) Pelvic osteolysis relationship to radiographs and polyethylene wear. J Arthroplasty 24:743–750
Koch KM, Lorbiecki JE, Hinks RS, King KF (2009) A multispectral three-dimensional acquisition technique for imaging near metal implants. Magn Reson Med 61:381–390
Lu W, Pauly KB, Gold GE, Pauly JM, Hargreaves BA (2009) SEMAC: Slice Encoding for Metal Artifact Correction in MRI. Magn Reson Med 62:66–76
Lu W, Pauly KB, Gold GE, Pauly JM, Hargreaves BA (2011) Slice encoding for metal artifact correction with noise reduction. Magn Reson Med 65:1352–1357
den Harder JC, van Yperen GH, Blume UA, Bos C (2014) Ripple artifact reduction using slice overlap in slice encoding for metal artifact correction. Magn Reson Med. doi:10.1002/mrm.25127
Koff MF, Shah P, Koch KM, Potter HG (2013) Quantifying image distortion of orthopedic materials in magnetic resonance imaging. J Magn Reson Imaging 38:610–618
Hayter CL, Koff MF, Shah P, Koch KM et al (2011) MRI after arthroplasty: comparison of MAVRIC and conventional fast spin-echo techniques. AJR Am J Roentgenol 197:W405–W411
Farrelly C, Davarpanah A, Brennan SA, Brennan S et al (2010) Imaging of soft tissues adjacent to orthopedic hardware: comparison of 3-T and 1.5-T MRI. AJR Am J Roentgenol 194:W60–W64
Yanny S, Cahir JG, Barker T, Wimhurst J et al (2012) MRI of aseptic lymphocytic vasculitis-associated lesions in metal-on-metal hip replacements. AJR Am J Roentgenol 198:1394–1402
Nawabi DH, Gold S, Lyman S, Fields K et al (2014) MRI predicts ALVAL and tissue damage in metal-on-metal hip arthroplasty. Clin Orthop Relat Res 472:471–481
Koch KM, Hargreaves BA, Pauly KB, Chen W et al (2010) Magnetic resonance imaging near metal implants. J Magn Reson Imaging 32:773–787
Liebl H, Heilmeier U, Lee S, Nardo L et al (2014) In vitro assessment of knee MRI in the presence of metal implants comparing MAVRIC-SL and conventional fast spin echo sequences at 1.5 and 3 T field strength. J Magn Reson Imaging. doi:10.1002/jmri.24668
Acknowledgments/Disclosures
Scientific guarantor of this publication is Prof Thomas M. Link. The authors of this manuscript declare relationships with the following companies: General Electric Healthcare. This study has received funding by General Electric Healthcare and National Institutes of Health (NIH). Grant numbers U01 AR059507, R01 AR057336 and P50 AR060752. We thank General Electric Healthcare for research funding and support. M.K. recieved grants from the Gottfried and Julia Bangerter-Rhyner Foundation. One of the authors Mrs Gabby B. Joseph has significant statistical expertise. Institutional review board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. Methodology: prospective, cross sectional study performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kretzschmar, M., Nardo, L., Han, M.M. et al. Metal artefact suppression at 3 T MRI: comparison of MAVRIC-SL with conventional fast spin echo sequences in patients with Hip joint arthroplasty. Eur Radiol 25, 2403–2411 (2015). https://doi.org/10.1007/s00330-015-3628-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-3628-0