Abstract
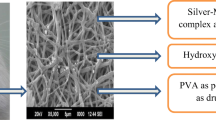
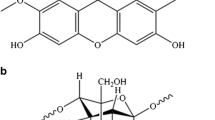
Periodontal disease is a set of inflammatory conditions affecting the tissues surrounding the teeth, which can be fairly preventable. In this research, antibacterial polymeric nanofibers were prepared for the management of periodontal disease treatment. New hybrid organic/inorganic nanofibers of chitosan/polyethylene oxide (CS/PEO) contains doxycycline hyclate (DOXH) (as an antibacterial drug) and silver/hydroxyapatite/silica (Ag/HA/Si) nanocomposite (CS/PEO-DOXH-Ag/HA/Si) fabricated by electrospinning technique. The nanofibers were characterized by Fourier transform infrared spectroscopy (FTIR), X-ray diffraction analysis (XRD), field emission scanning electron microscope (FE-SEM), thermogravimetric analysis (TGA) and transmission electron microscopy (TEM). In vitro release profile, degradation (DE) test, swelling (SW) test, antimicrobial activity and cell viability were also obtained. The DOXH release profile was measured by ultraviolet visible (UV–Vis) spectrophotometer in artificial saliva (pH 6.8) at 37 °C. The application of Ag/HA/Si increased the morphological integrity during the degradation process and decreased the rate of drug delivery. The electrospun nanofibers showed an enhanced antibacterial activity against Escherichia coli (E. coli), Staphylococcus aureus (S. aureus), and Streptococcus mutans (S. mutans) bacterium strains with the lowest DOXH amount, which can reduce the high dosage of antibiotics and side effects. Cell viability assays revealed that the prepared nanofibers had no cytotoxicity against the human gingival fibroblast 2 (HGF-2) cell line. The results suggest that the prepared organic/inorganic hybrid nanofibers with drug delivery properties could be a promising candidate for the treatment of periodontal diseases.










Similar content being viewed by others
References
Wong LB, Yap AU, Allen PF (2021) Periodontal disease and quality of life: umbrella review of systematic reviews. J Periodontal Res 56:1–17
Janakiram C (2000) Dye BA (2020) A public health approach for prevention of periodontal disease. Periodontol 84:202–214
Johnson A, Kong F, Miao S, Lin H-TV, Thomas S, Huang Y-C et al (2020) Therapeutic effects of antibiotics loaded cellulose nanofiber and κ-carrageenan oligosaccharide composite hydrogels for periodontitis treatment. Sci Rep 10:1–23
Balejo RDP, Cortelli JR, Costa FO, Cyrino RM, Aquino DR, Cogo-Müller K et al (2017) Effects of chlorhexidine preprocedural rinse on bacteremia in periodontal patients: a randomized clinical trial. J Appl Oral Sci 25:586–595
Pejčić A, Kesić L, Obradović R, Mirković D (2010) Antibiotics in the management of periodontal disease. Acta Fac med Naiss 27.
Jepsen K, Jepsen S (2016) Antibiotics/antimicrobials: systemic and local administration in the therapy of mild to moderately advanced periodontitis. J Periodontol 71:82–112
Dias AM, da Silva FG, de Figueiredo Monteiro AP, Pinzón-García AD, Sinisterra RD, Cortés ME (2019) Polycaprolactone nanofibers loaded oxytetracycline hydrochloride and zinc oxide for treatment of periodontal disease. Mater Sci Eng C 103:109798
Steinberg D, Friedman M (2020) Sustained-release delivery of antimicrobial drugs for the treatment of periodontal diseases: fantasy or already reality? J Periodontol 84:176–187
Nguyen S, Hiorth M (2015) Advanced drug delivery systems for local treatment of the oral cavity. Ther Deliv 6:595–608
Chadha VS, Bhat KM (2012) The evaluation of doxycycline controlled release gel versus doxycycline controlled release implant in the management of periodontitis. J Indian Soc Periodontol 16:200
Bapat RA, Joshi CP, Bapat P, Chaubal TV, Pandurangappa R, Jnanendrappa N et al (2019) The use of nanoparticles as biomaterials in dentistry. Drug Discov 24:85–98
Zięba M, Chaber P, Duale K, Martinka Maksymiak M, Basczok M, Kowalczuk M et al (2020) Polymeric carriers for delivery systems in the treatment of chronic periodontal disease. Polymers 12:1574
Eskitoros-Togay ŞM, Bulbul YE, Tort S, Korkmaz FD, Acartürk F, Dilsiz N (2019) Fabrication of doxycycline-loaded electrospun PCL/PEO membranes for a potential drug delivery system. Int J Pharm 565:83–94
Fakhri E, Eslami H, Maroufi P, Pakdel F, Taghizadeh S, Ganbarov K et al (2020) Chitosan biomaterials application in dentistry. Int J Biol Macromol 162:956–974
Divakar DD, Jastaniyah NT, Altamimi HG, Alnakhli YO, Alkheraif AA, Haleem S (2018) Enhanced antimicrobial activity of naturally derived bioactive molecule chitosan conjugated silver nanoparticle against dental implant pathogens. Int J Biol Macromol 108:790–797
Tao F, Cheng Y, Shi X, Zheng H, Du Y, **ang W et al (2020) Applications of chitin and chitosan nanofibers in bone regenerative engineering. Carbohydr Polym 230:115658
Abid S, Hussain T, Nazir A, Zahir A, Ramakrishna S, Hameed M et al (2019) Enhanced antibacterial activity of PEO-chitosan nanofibers with potential application in burn infection management. Int J Biol Macromol 135:1222–1236
Husain S, Al-Samadani KH, Najeeb S, Zafar MS, Khurshid Z, Zohaib S et al (2017) Chitosan biomaterials for current and potential dental applications. Materials 10:602
Yuan TT, Jenkins PM, DiGeorge Foushee AM, Jockheck-Clark AR, Stahl JM (2016) Electrospun chitosan/polyethylene oxide nanofibrous scaffolds with potential antibacterial wound dressing applications. J Nanomater 2016:1–10
Aliabadi M, Irani M, Ismaeili J, Piri H, Parnian MJ (2013) Electrospun nanofiber membrane of PEO/Chitosan for the adsorption of nickel, cadmium, lead and copper ions from aqueous solution. Chem Eng J 220:237–243
Chen C-K, Liao M-G, Wu Y-L, Fang Z-Y, Chen J-A (2020) Preparation of highly swelling/antibacterial cross-linked N-maleoyl-functional chitosan/polyethylene oxide nanofiber meshes for controlled antibiotic release. Mol Pharm 17:3461–3476
Chaturvedi TP, Srivastava R, Srivastava AK, Gupta V, Verma PK (2012) Evaluation of metronidazole nanofibers in patients with chronic periodontitis: a clinical study. Int J Pharm Investig 2:213
Chaturvedi T, Srivastava R, Srivastava A, Gupta V, Verma PK (2013) Doxycycline poly e-caprolactone nanofibers in patients with chronic periodontitis—a clinical evaluation. J Clin Diagn Res 7:2339
Carvalho LDd, Peres BU, Maezono H, Shen Y, Haapasalo M, Jackson J et al (2019) Doxycycline release and antibacterial activity from PMMA/PEO electrospun fiber mats. J Appl Oral Sci 27.
Khampieng T, Wnek GE, Supaphol PJJoBS, Polymer Edition (2014) Electrospun DOXY-h loaded-poly (acrylic acid) nanofiber mats: in vitro drug release and antibacterial properties investigation. J Biomater Sci Polym Ed 25:1292–1305
Bhushan J, Maini C (2019) Nanoparticles: a promising novel adjunct for dentistry. Indian J Dent Sci 11:167
Ebrahimi Z, Arezumand R, Ramazani A (2018) Nanobody as a new generation of functional proteins. Iran J Pharmaceutical Sci 14:91–106
Bapat RA, Chaubal TV, Joshi CP, Bapat PR, Choudhury H, Pandey M et al (2018) An overview of application of silver nanoparticles for biomaterials in dentistry. J Mater Sci 91:881–898
Zupančič Š, Casula L, Rijavec T, Lapanje A, Luštrik M, Fadda AM et al (2019) Sustained release of antimicrobials from double-layer nanofiber mats for local treatment of periodontal disease, evaluated using a new micro flow-through apparatus. J Control Release 316:223–235
Khan G, Yadav SK, Patel RR, Kumar N, Bansal M, Mishra B (2017) Tinidazole functionalized homogeneous electrospun chitosan/poly (ε-caprolactone) hybrid nanofiber membrane: development, optimization and its clinical implications. Int J Biol Macromol 103:1311–1326
Zupančič Š, Preem L, Kristl J, Putrinš M, Tenson T, Kocbek P et al (2018) Impact of PCL nanofiber mat structural properties on hydrophilic drug release and antibacterial activity on periodontal pathogens. Eur J Pharm Sci 122:347–358
Monteiro AP, Rocha CM, Oliveira MF, Gontijo SM, Agudelo RR, Sinisterra RD et al (2017) Nanofibers containing tetracycline/β-cyclodextrin: Physico-chemical characterization and antimicrobial evaluation. Carbohydr Polym 156:417–426
Kopytynska-Kasperczyk A, Dobrzynski P, Pastusiak M, Jarzabek B, Prochwicz W (2015) Local delivery system of doxycycline hyclate based on ϵ-caprolactone copolymers for periodontitis treatment. Int J Pharm 491:335–344
Ciobanu CS, Massuyeau F, Constantin LV, Predoi D (2011) Structural and physical properties of antibacterial Ag-doped nano-hydroxyapatite synthesized at 100 C. Nanoscale Res Lett 6:1–8.
Hao X, Hu X, Zhang C, Chen S, Li Z, Yang X et al (2015) Hybrid mesoporous silica-based drug carrier nanostructures with improved degradability by hydroxyapatite. ACS Nano 9:9614–9625
Zhuang Y, Yu H, Lin K (2019) Advance of nano-composite electrospun fibers in periodontal regeneration. Front Chem 7:495
Yassin FM, Fathy MM, Fahmy HM, Elshemey WM (2021) Low-angle X-ray scattering for the determination of the size of mesoporous silica nanoparticles. Radiat Phys Chem 179:109235
Kermanian M, Sadighian S, Ramazani A, Naghibi M, Hosseini SHJC (2021) A novel mesoporous superparamagnetic hybrid silica/hydroxyapatite nanocomposite as MRI contrast agent. ChemNanoMat 7:284–291
Qasim SB, Najeeb S, Delaine-Smith RM, Rawlinson A, Rehman IU (2017) Potential of electrospun chitosan fibers as a surface layer in functionally graded GTR membrane for periodontal regeneration. Dent Mater J 33:71–83
Scholz M, Reske T, Böhmer F, Hornung A, Grabow N, Lang H (2017) In vitro chlorhexidine release from alginate based microbeads for periodontal therapy. PLoS ONE 12:e0185562
Bajpai S, Jadaun M, Bajpai M, Jyotishi P, Shah FF, Tiwari SJ (2017) Controlled release of Doxycycline from gum acacia/poly (sodium acrylate) microparticles for oral drug delivery. Int J Biol Macromol 104:1064–1071
Praveen N, Rajesh A, Madan M, Chaurasia VR, Hiremath NV, Sharma AM (2014) In vitro evaluation of antibacterial efficacy of pineapple extract (bromelain) on periodontal pathogens. J Int Oral Health 6:96
Holešová S, Hundáková M, Tarasiuk Y, Barabaszová KČ, Pazdziora E (2021) Metronidazole/clay nanocomposites: synthesis, structure and antibacterial efficacy. Mater Today 37:1–27
Li W, ZhouXu JYJBr (2015) Study of the in vitro cytotoxicity testing of medical devices. Biomed Rep 3:617–620
Feura ES, Yang L, Schoenfisch MH (2021) Antibacterial activity of nitric oxide-releasing carboxymethylcellulose against periodontal pathogens. J Biomed Mater Res A 109:713–721
Amiri N, Ajami S, Shahroodi A, Jannatabadi N, Darban SA, Bazzaz BSF et al (2020) Teicoplanin-loaded chitosan-PEO nanofibers for local antibiotic delivery and wound healing. Int J Biol Macromol 162:645–656
Ramalingam R, Dhand C, Leung CM, Ong ST, Annamalai SK, Kamruddin M et al (2019) Antimicrobial properties and biocompatibility of electrospun poly-ε-caprolactone fibrous mats containing Gymnema sylvestre leaf extract. J Mater Sci 98:503–514
Su F, Wang Y, Liu X, Shen X, Zhang X, **ng Q et al (2018) Biocompatibility and in vivo degradation of chitosan based hydrogels as potential drug carrier. J Biomater Sci Polym Ed 29:1515–1528
Ni Z, Gu X, He Y, Wang Z, Zou X, Zhao Y et al (2018) Synthesis of silver nanoparticle-decorated hydroxyapatite (HA@ Ag) poriferous nanocomposites and the study of their antibacterial activities. RSC Adv 8:41722–41730.
Zamperini C, André R, Longo V, Mima E, Vergani CE, Machado AL et al (2013) Antifungal applications of Ag-decorated hydroxyapatite nanoparticles. J Nanomater. 2013:1–9
Kim S-G, Hagura N, Iskandar F, Okuyama K (2009) Characterization of silica-coated Ag nanoparticles synthesized using a water-soluble nanoparticle micelle. Adv Powder Technol 20:94–100
Yamada S, Nishikawa M, Tagaya M (2018) Mesoporous silica formation on hydroxyapatite nanoparticles. Mater Lett 211:220–224
Gorrasi G, Longo R, Viscusi G (2020) Fabrication and characterization of electrospun membranes based on “Poly (ε-caprolactone)”, “Poly (3-hydroxybutyrate)” and their blend for tunable drug delivery of curcumin. Polymers 12:2239
Naseri N, Algan C, Jacobs V, John M, Oksman K, Mathew AP (2014) Electrospun chitosan-based nanocomposite mats reinforced with chitin nanocrystals for wound dressing. Carbohydr Polym 109:7–15
Chen G, Fang D, Wang K, Nie J, Ma G (2015) Core–shell structure PEO/CS nanofibers based on electric field induced phase separation via electrospinning and its application. J Polym Sci, Part A-1: Polym Chem 53:2298–2311.
Mallakpour S, Abbasi M (2020) Hydroxyapatite mineralization on chitosan-tragacanth gum/silica@ silver nanocomposites and their antibacterial activity evaluation. Int J Biol Macromol 151:909–923
Sadighian S, Rostamizadeh K, Hosseini M-J, Hamidi M, Hosseini-Monfared H (2017) Magnetic nanogels as dual triggered anticancer drug delivery: toxicity evaluation on isolated rat liver mitochondria. Toxicol Lett 278:18–29
Stie MB, Gätke JR, Wan F, Chronakis IS, Jacobsen J, Nielsen HM (2020) Swelling of mucoadhesive electrospun chitosan/polyethylene oxide nanofibers facilitates adhesion to the sublingual mucosa. Carbohydr Polym 242:116428
Shahryari F, Rabiei Z, Sadighian S (2020) Antibacterial activity of synthesized silver nanoparticles by sumac aqueous extract and silver-chitosan nanocomposite against Pseudomonas syringae pv. syringae. J Plant Pathol 102:469–475
Kumar S, Koh J (2012) Physiochemical, optical and biological activity of chitosan-chromone derivative for biomedical applications. Int J Mol Sci 13:6102–6116
Hashemikia S, Farhangpazhouh F, Parsa M, Hasan M, Hassanzadeh A, Hamidi M (2021) Fabrication of ciprofloxacin-loaded chitosan/polyethylene oxide/silica nanofibers for wound dressing application: In vitro and in vivo evaluations. Int J Pharm, 120313.
Ramya R, Sudha P, Mahalakshmi J (2012) Preparation and characterization of chitosan binary blend. Int J Sci Res Publ 2:1–9
An J, Zhang H, Zhang J, Zhao Y, Yuan XJC, Science P (2009) Preparation and antibacterial activity of electrospun chitosan/poly (ethylene oxide) membranes containing silver nanoparticles. Colloid Polymer Sci 287:1425–1434.
Kohsari I, Shariatinia Z, Pourmortazavi SMJCp (2016) Antibacterial electrospun chitosan–polyethylene oxide nanocomposite mats containing bioactive silver nanoparticles. Int J Biol Macromol 140:287–298.
Qasim SB, Najeeb S, Delaine-Smith RM, Rawlinson A, Rehman IU (2017) Potential of electrospun chitosan fibers as a surface layer in functionally graded GTR membrane for periodontal regeneration. Dent Mater 33:71–83
Abid S, Hussain T, Nazir A, Zahir A, Ramakrishna S, Hameed M et al (2019) Enhanced antibacterial activity of PEO-chitosan nanofibers with potential application in burn infection management. Int J Biol Macrool 135:1222–1236
Hashemikia S, Farhangpazhouh F, Parsa M, Hasan M, Hassanzadeh A, Hamidi M (2021) Fabrication of ciprofloxacin-loaded chitosan/polyethylene oxide/silica nanofibers for wound dressing application: in vitro and in vivo evaluations. Int J Pharm 597:120313
Kouhi M, Morshed M, Varshosaz J, Fathi MH (2013) Poly (ε-caprolactone) incorporated bioactive glass nanoparticles and simvastatin nanocomposite nanofibers: preparation, characterization and in vitro drug release for bone regeneration applications. Chem Eng J 228:1057–1065
Wu J, Zhang Z, Zhou W, Liang X, Zhou G, Han CC et al (2020) Mechanism of a long-term controlled drug release system based on simple blended electrospun fibers. J Control Release 320:337–346
Kataria K, Gupta A, Rath G, Mathur R, Dhakate S (2014) In vivo wound healing performance of drug loaded electrospun composite nanofibers transdermal patch. Int J Pharm 469:102–110
Goudouri O-M, Kontonasaki E, Lohbauer U, Boccaccini AR (2014) Antibacterial properties of metal and metalloid ions in chronic periodontitis and peri-implantitis therapy. Acta Biomater 10:3795–3810
Acknowledgements
We thank the research deputy of Zanjan University of Medical Science (ZUMS) for the financial support of this project (Grant Number: A-12-349-44 and ethical code: IR.ZUMS.REC.1399.339).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hakimi, F., Hashemikia, S., Sadighian, S. et al. Nanofibrous chitosan/polyethylene oxide silver/hydroxyapatite/silica composite as a potential biomaterial for local treatment of periodontal disease. Polym. Bull. 80, 8703–8723 (2023). https://doi.org/10.1007/s00289-022-04466-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00289-022-04466-x