Abstract
Introduction
Colorectal cancer (CRC) is the second leading cause of cancer mortality in the USA. We aimed to determine racial and socioeconomic disparities in the surgical management and outcomes of patients with CRC in a contemporary, national cohort.
Methods
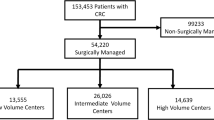
We performed a retrospective analysis of the National Inpatient Sample for the period 2009–2015. Adult patients diagnosed with CRC and who underwent colorectal resection were included. Multivariable linear and logistic regressions were used to assess the effect of race, insurance type, and household income on patient outcomes.
Results
A total of 100,515 patients were included: 72,552 (72%) had elective admissions and 27,963 (28%) underwent laparoscopic surgery. Patients with private insurance and higher household income were consistently more likely to have laparoscopic procedures, compared to other insurance types and income levels, p < 0.0001. Black patients, compared to white patients, were more likely to have postoperative complications (OR 1.23, 95% CI, 1.17, 1.29). Patients with Medicare and Medicaid, compared to private insurance, were also more likely to have postoperative complications (OR 1.30, 95% CI, 1.24, 1.37 and OR 1.40, 95% CI, 1.31, 1.50). Patients in low-household-income areas had higher rates of any complication (OR 1.11, 95% CI 1.06, 1.16).
Conclusions
The use of laparoscopic surgery in patients with CRC is strongly influenced by insurance type and household income, with Medicare, Medicaid and low-income patients being less likely to undergo laparoscopic surgery. In addition, black patients, patients with public insurance, and patients with low household income have significant worse surgical outcomes.


Similar content being viewed by others
References
Siegel RL, Miller KD, Fedewa SA et al (2017) Colorectal cancer statistics, 2017. CA Cancer J Clin 67(3):177–193
Chen CF, Lin YC, Tsai HL, et al (2018) Short-and long-term outcomes of laparoscopic-assisted surgery, mini-laparotomy and conventional laparotomy in patients with Stage I–III colorectal cancer. J Minim Access Surg, epub ahead of print
Shavers VL (2007) Racial/ethnic variation in the anatomic subsite location of in situ and invasive cancers of the colon. J Natl Med Assoc 99:733–748
Dignam JJ, Colangelo L, Tian W et al (1999) Outcomes among African–Americans and Caucasians in colon cancer adjuvant therapy trials: findings from the National Surgical Adjuvant Breast and Bowel Project. J Natl Cancer Inst 91:1933–1940
Doubeni CA, Field TS, Buist DS et al (2007) Racial differences in tumor stage and survival for colorectal cancer in an insured population. Cancer 109:612–620
Aarts MJ, Lemmens VE, Louwman MW et al (2010) Socioeconomic status and changing inequalities in colorectal cancer? A review of the associations with risk, treatment and outcome. Eur J Cancer 46:2681–2695
Zhang Q, Wang Y, Hu H et al (2017) Impact of socioeconomic status on survival of colorectal cancer patients. Oncotarget 8:106121–106131
Jemal A, Siegel R, Ma J et al (2015) Inequalities in premature death from colorectal cancer by state. J Clin Oncol 33:829–835
Schlottmann F, Strassle PD, Charles AG et al (2018) Esophageal cancer surgery: spontaneous centralization in the US contributed to reduce mortality without causing health disparities. Ann Surg Oncol 25(6):1580–1587
Schlottmann F, Gaber C, Strassle PD, et al (2018) Cholecystectomy vs. cholecystostomy for the management of acute cholecystitis in elderly patients. J Gastrointest Surg, epub ahead of print
Weeks JC, Nelson H, Gelber S et al (2002) Short-term quality-of-life outcomes following laparoscopic-assisted colectomy vs open colectomy for colon cancer: a randomized trial. JAMA 287(3):321–328
Kaiser AM, Kang JC, Chan LS et al (2004) Laparoscopic-assisted vs. open colectomy for colon cancer: a prospective randomized trial. J Laparoendosc Adv Surg Tech 14(6):329–334
Milsom JW, Bohm B, Hammerhofer KA et al (1998) A prospective, randomized trial comparing laparoscopic versus conventional techniques in colorectal cancer surgery: a preliminary report. J Am Coll Surg 187(1):46–54
Bagshaw PF, Allardyce RA, Frampton CM et al (2012) Long-term outcomes of the Australasian randomized clinical trial comparing laparoscopic and conventional open surgical treatments for colon cancer: the Australasian Laparoscopic Colon Cancer Study trial. Ann Surg 256(6):915–919
Soneji S, Iyer SS, Armstrong K, Asch DA (2010) Racial disparities in stage-specific colorectal cancer mortality: 1960–2005. Am J Public Health 100:1912–1916
Siegel R, Naishadham D, Jemal A (2013) Cancer statistics, 2013. CA Cancer J Clin 63:11–30
Tammana VS, Laiyemo AO (2014) Colorectal cancer disparities: issues, controversies and solutions. World J Gastroenterol 20(4):869–876
Bolen JC, Rhodes L, Powell-Griner EE et al (2000) State-specific prevalence of selected health behaviors, by race and ethnicity—behavioral risk factor surveillance system, 1997. MMWR CDC Surveill Summ 49:1–60
Advani AS, Atkeson B, Brown CL et al (2003) Barriers to the participation of African–American patients with cancer in clinical trials: a pilot study. Cancer 97:1499–1506
Gregg J, Curry RH (1994) Explanatory models for cancer among African–American women at two Atlanta neighborhood health centers: the implications for a cancer screening program. Soc Sci Med 39:519–526
Ravi P, Sood A, Schmid M et al (2015) Racial/ethnic disparities in perioperative outcomes in major procedures: results from national surgical quality improvement program. Ann Surg 262(6):955–964
Alnasser M, Schneider EB, Gearhart SL et al (2014) National disparities in laparoscopic colorectal procedures for colon cancer. Surg Endosc 28(1):49–57
Mehtsun WT, Figueroa JF, Zhang J et al (2017) Racial disparities in surgical mortality: the gap appears to have narrowed. Health Affairs 36(6):64
Robbins AS, Chen AY, Stewart AK et al (2010) Insurance status and survival disparities among nonelderly rectal cancer patients in the national cancer data base. Cancer 116:4178–4186
Robbins AS, Pavluck AL, Fedewa SA et al (2009) Insurance status, comorbidity level, and survival among colorectal cancer patients age 18 to 64 years in the national cancer data base from 2003 to 2005. J Clin Oncol 27:3627–3633
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cairns, A.L., Schlottmann, F., Strassle, P.D. et al. Racial and Socioeconomic Disparities in the Surgical Management and Outcomes of Patients with Colorectal Carcinoma. World J Surg 43, 1342–1350 (2019). https://doi.org/10.1007/s00268-018-04898-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-04898-5